Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Madeenaguda, Miyapur, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: PACE Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: PACE Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code via Any Payment App (GPay, Paytm, PhonePe, BHIM, Bank Apps, PayZapp, Amazon, Airtel, Truecaller, WhatsApp, etc).
CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
Accreditations




Follow PACE Hospitals
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
SPECIALITIES
- Gastroenterology
- Hepatology
- Organ Transplant
- Bariatric and Metabolic Surgery
- Urology
- Nephrology
- Cardiology
- Cardiothoracic & Vascular Surgery
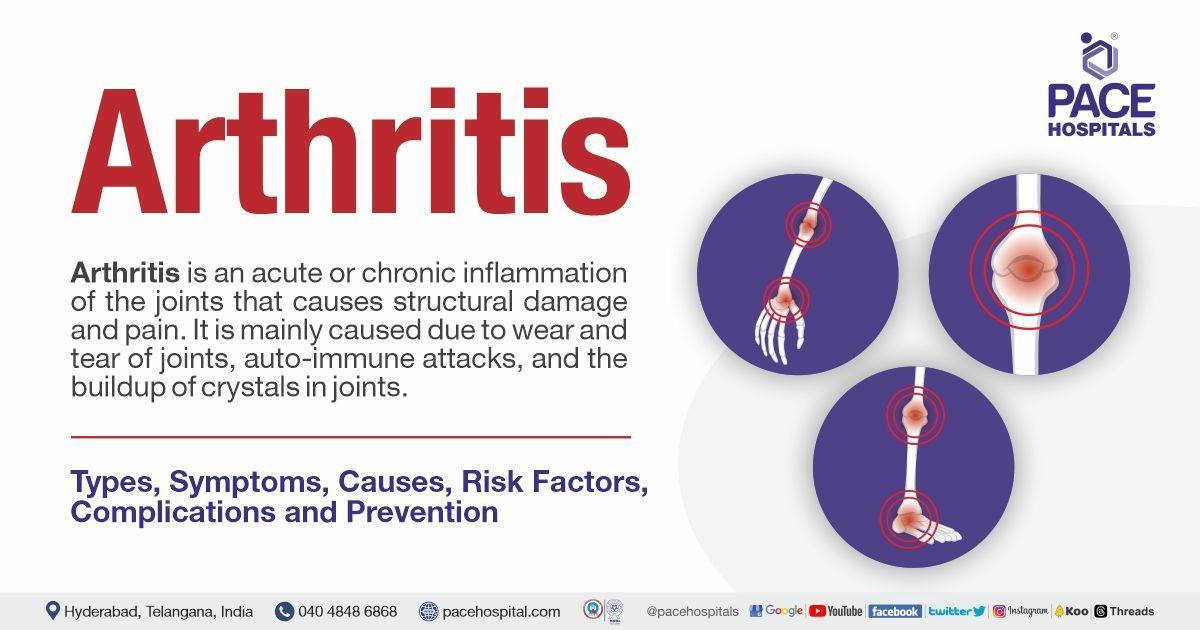
- Orthopaedics
- Spine Surgery
- Sports Medicine
- Gynaecology
- Oncology
- Internal Medicine
- Endocrinology
- Diabetology
- Pulmonology
- Neurology
- Neurosurgery
- Paediatrics
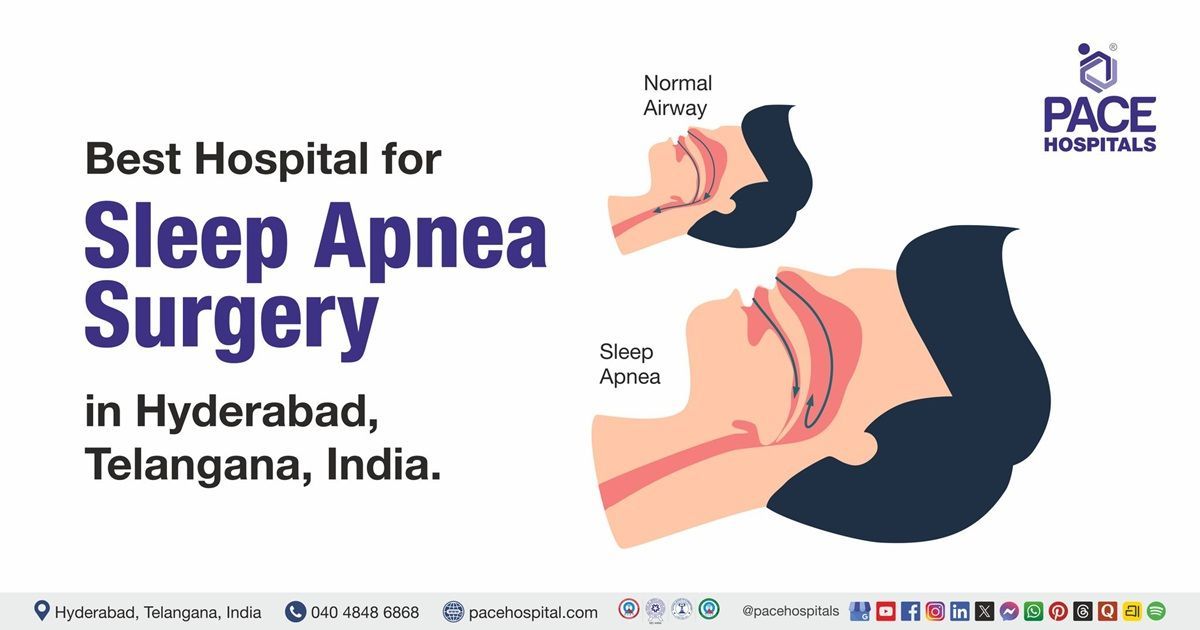
- ENT
- Interventional Radiology
- Plastic & Reconstructive Surgery
- Dermatology
- Psychiatry
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital in Hyderabad, India.
All Rights Reserved | PACE Hospitals