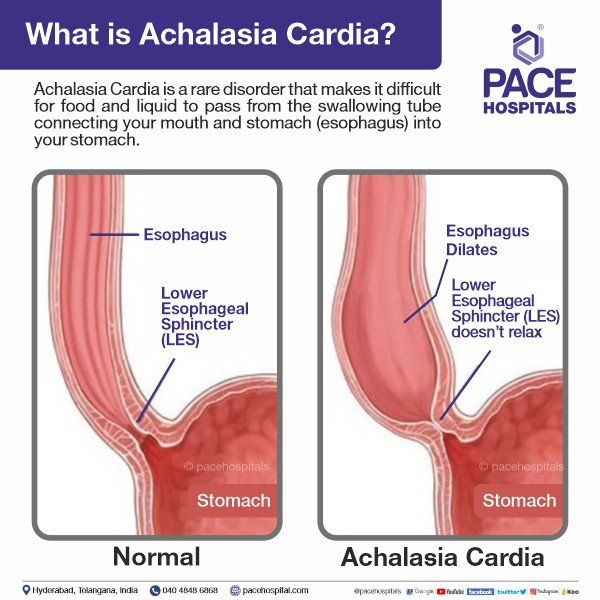
Achalasia Cardia: Symptoms, Diagnosis and Treatment
Achalasia Cardia is a rare disorder that makes it difficult for food and liquid to pass from the swallowing tube connecting your mouth and stomach (esophagus) into your stomach.
Achalasia Cardia occurs when nerves in the esophagus become damaged. As a result, the esophagus becomes paralyzed and dilated over time and eventually loses the ability to squeeze food down into the stomach. Food then collects in the esophagus, sometimes fermenting and washing back up into the mouth, which can taste bitter. Some people mistake this for gastroesophageal reflux disease (GERD). However, in achalasia the food is coming from the esophagus, whereas in GERD the material comes from the stomach.
There's no cure for Achalasia Cardia. Once the esophagus is paralyzed, the muscle cannot work properly again. But symptoms can usually be managed with endoscopy, minimally invasive therapy or surgery.
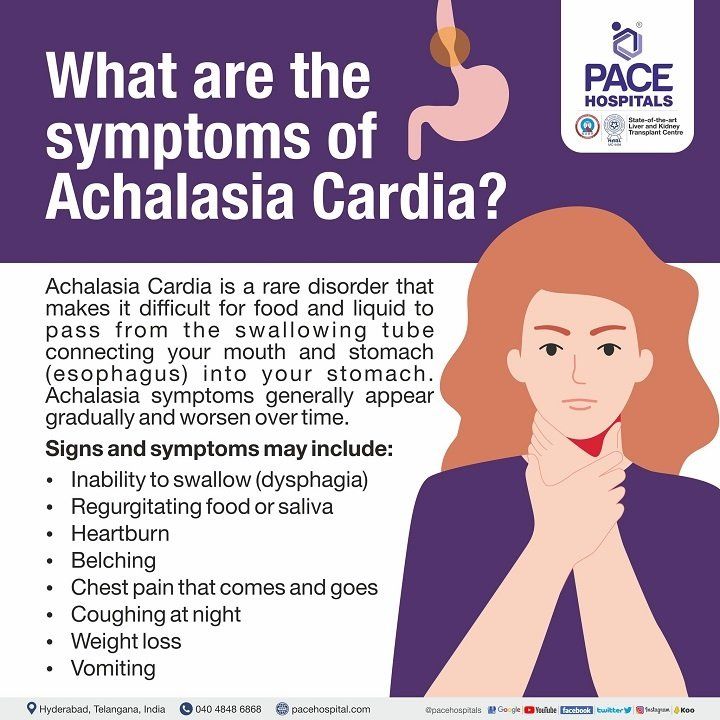
What are the Symptoms of Achalasia Cardia?
Achalasia symptoms generally appear gradually and worsen over time. Signs and symptoms may include:
- Inability to swallow (dysphagia), which may feel like food or drink is stuck in your throat
- Regurgitating food or saliva
- Heartburn
- Belching
- Chest pain that comes and goes
- Coughing at night
- Pneumonia (from aspiration of food into the lungs)
- Weight loss
- Vomiting
Types of Achalasia Cardia
Achalasia is a heterogeneous disease categorized into three distinct types based on manometric patterns of the oesophagus (pressure and movement measurements of oesophagal contractions during swallowing), including:
- Type I: It is also called classic achalasia. The oesophagus doesn’t move food down well in this condition but shows minimal contractility (very little activity).
- Type II: In this type, pressure builds up in the esophagus, causing it to become compressed with intermittent periods of panesophageal pressurization, where the entire esophagus exerts pressure to push food down, but this doesn’t happen consistently.
- Type III: It is also known as spastic achalasia because it involves premature or spastic contractions in the lower part (bottom) of the oesophagus, where it meets the stomach, which is the most severe type of achalasia. The contractions may cause chest pain that can wake a person from sleep and mimic the symptoms of a heart attack.
What are the Causes of Achalasia Cardia?
The exact cause of achalasia cardia is not known clearly. Super specialist suspect it may be caused by a loss of nerve cells in the esophagus. There are scientific papers about what causes this, but viral infection or autoimmune responses have been suspected. Very rarely, achalasia cardia may be caused by an inherited genetic disorder or infection.
How to diagnose Achalasia Cardia?
Achalasia Cardia can be overlooked or misdiagnosed because it has symptoms similar to other digestive disorders. To test for achalasia cardia, we recommend:
- Esophageal manometry: This test measures the rhythmic muscle contractions in your esophagus when you swallow, the coordination and force exerted by the esophagus muscles, and how well your lower esophageal sphincter relaxes or opens during a swallow. This test is the most helpful when determining which type of motility problem you might have.
- X-rays of your upper digestive system (esophagram): X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows doctor to see a silhouette of your esophagus, stomach and upper intestine. You may also be asked to swallow a barium pill that can help to show a blockage of the esophagus.
- Upper endoscopy: Gastroenterologist inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat, to examine the inside of your esophagus and stomach. Endoscopy can be used to define a partial blockage of the esophagus if your symptoms or results of a barium study indicate that possibility. Endoscopy can also be used to collect a sample of tissue (biopsy) to be tested for complications of reflux such as Barrett's esophagus.
What are the treatment options available for Achalasia Cardia?
Achalasia Cardia treatment focuses on relaxing or stretching open the lower esophageal sphincter so that food and liquid can move more easily through your digestive tract.
Specific treatment depends on your age, health condition and the severity of the achalasia.
Medication: Gastroentrologist might suggest muscle relaxant before eating. These medications have limited treatment effect and severe side effects. Medications are generally considered only if you're not a candidate for pneumatic dilation or surgery, and other medications hasn't helped. This type of therapy is rarely indicated.
Surgical options for treating achalasia cardia include:
Heller Myotomy: The surgeon cuts the muscle at the lower end of the esophageal sphincter to allow food to pass more easily into the stomach. The procedure can be done non-invasively (Laparoscopic Heller Myotomy). Some people who have a Heller myotomy may later develop gastroesophageal reflux disease (GERD).
To avoid future problems with GERD, a procedure known as fundoplication might be performed at the same time as a Heller myotomy. In fundoplication, the surgeon wraps the top of your stomach around the lower esophagus to create an anti-reflux valve, preventing acid from coming back (GERD) into the esophagus. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure.
Peroral endoscopic myotomy (POEM): In the POEM procedure, the Gastroenterologists uses an endoscope inserted through your mouth and down your throat to create an incision in the inside lining of your esophagus. Then, as in a Heller myotomy, the surgeon cuts the muscle at the lower end of the esophageal sphincter.
POEM may also be combined with or followed by later fundoplication to help prevent GERD. Some patients who have a POEM and develop GERD after the procedure are treated with daily oral medication.
Frequently Asked Questions:
Is achalasia cardia hereditary?
No, achalasia cardia is not an inherited genetic disorder.
Can achalasia cause heart problems?
No, achalasia cardia can never cause heart disease or condition.
Can you die from achalasia cardia?
Yes, a person can die from achalasia cardia because of large food or water content into the esophagus; regurgitating into the windpipe (trachea) causing aspiration, pneumonia and choking.
How to differentiate achalasia cardia from carcinoma of oesophagus?
We can differentiate by doing special test like endoscopy, CT scan, esophageal manometry and Biopsy.
What is incidence of Achalasia Cardia?
Incidence of achalasia cardia in India is
0.6% to 1% of 1,00,000 population.
What are the complications of Achalasia Cardia?
These are some complications of achalasia cardia:
- Fungal infection of food pipe or the esophagus (esophagitis)
- GI bleeding from the food pipe
- Pneumonia
- Lung infections
- Esophageal cancer
Is achalasia cardia autoimmune disorder?
Yes, chronic infection of food pipe activates auto immune antibody response against ganglionic cells causing loss of neurons and achalasia cardia.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Hafeezpet, Madeenaguda, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc).

CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
FOLLOW US
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital near me.