Fatty Liver Treatment
in Hyderabad, India
PACE Hospitals is one of the best hospitals for fatty liver treatment in Hyderabad, India, offering expert care for Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD). Our experienced hepatologists and liver specialists provide a multidisciplinary approach to managing fatty liver disease through dietary counseling, lifestyle modifications, medications, and advanced liver care therapies.
If you are experiencing fatigue, abdominal discomfort, or abnormal liver function tests, it is crucial to seek early intervention. At PACE Hospitals, we offer state-of-the-art diagnostics, liver function tests, ultrasound, and FibroScan to assess the severity of liver damage. Our personalized treatment plans focus on reversing fatty liver and preventing complications like liver fibrosis, cirrhosis, or liver failure.
Request an Appointment for Fatty Liver Treatment
Fatty liver treatment - appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
PACE Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
PACE Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Fatty Liver Treatment?
Fatty liver diagnosis
The evaluation of fatty liver disease involves a thorough medical history, alcohol consumption, physical examination, and risk factors for metabolic disorders, which assist the gastroenterologist or hepatologist in determining the diagnosis.
The earlier the diagnosis is made, and lifestyle modifications are implemented, the better the chances of reversing fatty liver disease and preventing progression to more serious conditions such as cirrhosis.
The gastroenterologist or hepatologist considers the following before selecting the appropriate tests to detect fatty liver.
- The presented signs and symptoms: In majority of the patients, the fatty liver disease is asymptomatic. However, some patients do have symptoms such as fatigue, nausea, and upper right abdominal pain.
- Age, family history, and general health of the suspected patient: Gastroenterologists would like to know about the patient’s age, condition, family history and general health of the suspected patient.
- Lifestyle habits: During the medical assessment, gastroenterologists gather information regarding the aspects of patient’s lifestyle to better understand the potential contributors to fatty liver disease. Gastroenterologist or hepatologist will inquire about the dietary and lifestyle habits that could potentially increase the risk of developing fatty liver. This may include factors such as insufficient physical activity, consumption of a diet rich in sugar, consumption of alcohol or regular intake of sugary beverages.
- Medical history and medication history: Medication and medical history that incudes diabetes, presence of metabolic syndrome, pregnancy, alcohol intake status can be considered before choosing tests.
- The results of previous medical tests: Gastroenterologists may go through the patient’s medical background, physical examination, other diagnostic tests and previous surgeries to determine fatty liver and its types.
- Physical examination: During a physical examination, gastroenterologist typically assess the patient’s condition by conducting a thorough physical examination such as abdominal palpation and calculate patient’s body mass index (BMI) by collecting their body weight and height.
However, gastroenterologist specifically look for the following physical signs:
- Hepatomegaly (Enlarged liver): Gastroenterologist will assess the size of patient’s liver by palpating or feeling their abdomen, because an enlarged liver might be a sign of fatty liver disease.
- Signs of insulin resistance: The darkened pigmentation around neck, armpits, elbows and knees known as acanthosis nigricans, that associates with insulin resistance. It is commonly seen in non-alcoholic fatty liver disease.
- Signs of Alcoholic hepatitis: On physical exam, the patients with alcoholic hepatitis will present with tachycardia (increase in heart rate), fever, tachypnoea (rapid breathing).
- Signs of cirrhosis: Gastroenterologist will look for some signs of advanced liver disease, such as an enlarged spleen (splenomegaly), the presence of fluid accumulation in the abdomen (ascites), and muscle loss, which can be a sign of cirrhosis.
Only a small percentage of individuals show physical signs and symptoms that are typically associated with chronic liver disease, such as:
- Spider angiomas (small, dilated blood vessels resembling spider legs)
- Palmar erythema (redness of the palms)
- Jaundice (yellowing of the skin and eyes) and
- Features of portal hypertension
The major sign of liver fibrosis, such as ascites (abnormal fluid accumulation in the abdominal cavity), variceal haemorrhage (enlarged veins bleeds in the region of oesophagus or stomach).
Based on on the above information and the patient’s intake of alcohol the gastroenterologist would further diagnose the patient’s condition into two categories such as:
- Non-alcoholic fatty liver disease
- Alcoholic fatty liver disease
✅Fatty liver diagnosis tests
The majority of the tests and examinations will be similar in both non-alcoholic fatty liver disease and alcoholic fatty liver disease. Based on the patient’s symptoms, and physical examination, the gastroenterologists might predict the patient's condition as a fatty liver or liver disease (provisional diagnosis). Therefore, the gastroenterologists would like to go for the following fatty liver test to confirm the diagnosis, such as:
Fatty liver diagnosis tests
- Lab tests
- Imaging tests
- Advanced tests
- Biopsy tests
Fatty liver lab tests
A sample of blood will be collected and sent to the laboratory for further examination. The following are the some of the tests that can be performed alone or combination by the healthcare professional to diagnose the fatty liver.
- ALT and AST: ALT and AST are enzymes present in the liver, when liver cells are damaged or inflamed, these enzymes are released and elevated in the bloodstream.
- Gamma-glutamyl transferase (GGT): GGT is an enzyme found in the liver. When elevated, it can indicate a liver damage or dysfunction.
- Albumin: Albumin is a protein synthesised by the liver. In the case of abnormal liver function, the liver might decrease albumin production.
- Bilirubin: Bilirubin is the byproduct of the red blood cell damage, excreted by the liver. Due to any instance of liver damage, it may not eliminate bilirubin efficiently, leading to accumulation of bilirubin in the blood (jaundice), resulting in hyperbilirubinemia.
- Prolonged prothrombin time: The liver produces several coagulating factors, when liver is not functioning properly. The production of coagulation factors is decreased, and it leads to prolonged prothrombin time (easy bleeding or bruising, means takes so much time to clot the blood).
- International normalized ratio (INR): This test is used to evaluate the time it takes for blood to clot. It can also be used to monitor the effect of blood-thinning medication on patients with liver problems (liver cirrhosis).
- Immunoglobulins Blood Test: Immunoglobulins measure the amounts of IgA, IgG and IgM in the blood that are usually elevated due to impaired clearance by the liver.
- Basic Metabolic Profile (BMP): BMP is a blood test that provides information about metabolism.
- Complete blood count (CBCs): This provides the complete information of the red and white blood cell count. Macrocytic anaemia (increased size of red blood cells) is typical lab finding of alcoholic liver cirrhosis. Leukopenia (reduced white blood cells) and thrombocytopenia (decreased platelet count) are also seen due to spleen enlargement and alcohol suppression effect on the bone marrow.
- Homeostasis Model Assessment Insulin Resistance (HOMA-IR) and (QUICKI): These two common lab tests used to evaluate insulin resistance in non-alcoholic fatty liver.
Imaging tests
If there is any sign of liver abnormality from the above-mentioned fatty liver lab tests, the gastroenterologist might prescribe the following imaging tests to confirm the fatty liver disease and its stages.
- Ultrasound: It is an efficient diagnostic procedure used to evaluate the size and shape of the liver. It can be used for identifying cirrhosis and its complications, such as:
- Splenomegaly (increased spleen size)
- Portal hypertension (blood pressure increase in the vein supplying blood to the liver)
- Ascites (distended abdomen)
- Hepatocellular cancer (liver cancer)
- Computed Tomography (CT) scan: A non-invasive diagnostic imaging procedure, computed tomography of the liver (CT scan) utilises the effect of computerised X-rays producing horizontal or axial images of the body (often called slices). It produces much more detailed images of the body.
- Magnetic Resonance Imaging (MRI Scan): MRI of the liver, a non-invasive diagnostic imaging procedure, that utilises the effect of radio waves to provide detailed images of the liver (often called slices).
Advanced tests
From the above-mentioned tests, if the there are any abnormalities, the gastroenterologist further prescribe the following advanced tests to confirm advanced stages like fibrosis or cirrhosis.
- Ascitic Fluid SAAG (Serum-Ascites Albumin Gradient): Ascites often seen in advanced liver disease or cirrhosis. It helps to determine the underlying cause of ascites.
- Endoscopy: UGI endoscopy is helpful in diagnosing abnormal blood vessels called oesophageal varices; this can happen due to blood flow being blocked in the portal vein because of liver cirrhosis.
- Elastography is a more recent imaging technique that can assist in assessing the advanced stages of liver. It provides information about the stiffness or elasticity of the liver.
- There are several common types of elastography:
- Vibration-Controlled Transient Elastography (VCTE): VCTE is a specialised form of ultrasound-based elastography used to find liver fibrosis.
- Shear Wave Elastography (SWE): SWE is another ultrasound-based elastography method to find fibrosis and its severity.
- Magnetic Resonance Elastography (MRE): MRE is a specialised type of MRI that is used to measure liver stiffness and liver cirrhosis.
Scoring systems can assess the severity and prognosis of liver disease such as ALBI (Albumin-Bilirubin) score, Child’s Turcotte-Pugh classification, and MELD (Model for End stage Liver Disease) score.
Liver biopsy
- If the abnormality was confirmed, the gastroenterologists or hepatologists may conduct liver biopsy to confirm the significant stage of the liver. It is advantageous in detecting early-stage fibrosis that other non-invasive tests like elastography may not see.
- It is the gold standard for confirming diagnosis of fatty liver and its detailed information, liver biopsy is a procedure of collecting small samples of liver tissue and taken to assess the severity of condition. However, it is not recommended for all the patients, but it is used for individuals with a higher likelihood of advanced fibrosis or when other tests suggest progressive liver disease or cirrhosis.
Fatty liver treatment
Patients with alcoholic liver disease engage in heavy alcohol consumption, while NAFLD patients are typically characterised by obesity and the presence of insulin resistance and/or metabolic syndrome. This is reversible stage; therefore, lifestyle modifications can aid in treating this condition in addition to medical management.
Non-alcoholic fatty liver disease treatment
- Pharmacological treatment options
- Anti-obesity preparations
- Insulin sensitizers
- Lipid lowering agents
- Vitamin E Therapy
- Incretin analogues
- Non-pharmacological treatment options
- Weight loss
- Dietary modification
- Regular exercise
- Management of risk factors
- Surgical treatment
- Bariatric surgery
Alcoholic fatty liver treatment
- Pharmacological treatment options
- Glucocorticosteroids
- Non-pharmacological treatment options
- Stopping/quitting alcohol intake
- Withdrawal symptoms
- Nutritional support
- Surgical treatment
- Liver transplant
Non-alcoholic fatty liver disease treatment
Pharmacological treatment options
- Anti-obesity preparations: This class of drugs are prescribed to manage body weight, as these are lipase inhibitors act by hindering fat absorption in the liver and intestines effectively. This results in curbing appetite and ultimately leading to weight loss.
- Insulin sensitizers: This plays a crucial role in the treatment of NAFLD due to its strong correlation with obesity and metabolic syndrome, both of which contribute to insulin resistance. By improving the body's response to insulin, these agents aid in mitigating insulin resistance and can have a positive impact on the management of NAFLD and related conditions.
- Lipid lowering agents: These are commonly used to reduce elevated cholesterol and triglyceride levels in the bloodstream. By effectively lowering lipid levels, they can help in reducing the accumulation of fat in the liver and mitigate the progression of fatty liver disease. NAFLD correlates with obesity and metabolic syndrome, characterised by increased cholesterol and triglyceride levels. Consequently, the utilisation of lipid-lowering agents can be advantageous.
- Vitamin E Therapy: The development of NAFLD, results in oxidative stress, which leads to inflammation and harm to liver cells. Vitamin E comprises of antioxidative and anti-inflammatory properties, that aids in reducing the inflammation of liver cells. However, the potential therapeutic role of vitamin E has been investigated.
- Incretin analogues: Studies have shown that GLP-1 receptor agonists have beneficial effects on fatty liver disease. They can improve insulin sensitivity, reduce liver fat accumulation, and decrease inflammation in the liver. Additionally, GLP-1 receptor agonists have been associated with weight loss, which is beneficial for individuals with fatty liver disease, as excess weight can contribute to liver disease development and its progression.
However, further research is needed to establish the precise mechanisms and long-term effects of incretin analogues in fatty liver disease.
Non-pharmacological treatment options
Lifestyle modifications are advised for all individuals diagnosed with non-alcoholic fatty liver disease (NAFLD).
- Weight loss: For individuals with simple (fatty liver) steatosis, it is recommended to achieve a reduction in weight ranging from 3 to 5%. In the case of advanced liver diseases (NASH), a weight loss of 7% to 10% is recommended.
- Dietary modification: Dietary adjustments are essential as they significantly impact the development of obesity, insulin resistance, and non-alcoholic fatty liver disease (NAFLD). Diet rich in carbohydrates, particularly high-fructose content, is recognised as the primary contributor to these conditions.
- Regular exercise: Increased physical activity plays a beneficial role in preventing and halting the progression of liver-related conditions associated with fat accumulation and fibrosis.
- Management of risk factors: It is necessary to effectively manage risk factors such as high cholesterol levels, hypertension, and maintain appropriate glycaemic control.
Surgical treatment
- Bariatric surgery: It is a medical procedure commonly performed on severely obese individuals who is diagnosed with non-alcoholic fatty liver disease (NAFLD). While steady weight loss achieved through exercise and lifestyle changes, that has been shown to improve insulin sensitivity and liver health in NAFLD patients, the rapid weight loss induced by bariatric surgery poses an increased risk of hepatic failure, particularly in patients with cirrhosis of the liver. Therefore, bariatric surgery is typically recommended for non-cirrhotic NAFLD patients who are morbidly obese.
However, it is not recommended as the primary mode of treatment in morbidly obese patients due to the potential risk of liver failure following the surgery. The gastroenterologists would prefer bariatric surgery for patient diagnosed with NAFLD based on risk by benefit analysis.
Interventions such as weight loss surgery, vitamin E supplementation, and pharmaceutical treatment with anti-obesity agents have demonstrated potential advantages. However, the available data are restricted, and these therapies are not commonly regarded as standard treatments.
Alcoholic fatty liver treatment
Currently, there is no particular medical treatment for Alcoholic fatty liver disease. The first line of treatment for this condition is to stop or quit the intake of alcohol for the rest of the patient's life. This treatment can stop the risk of further damage and gives the best chance to recover the liver.
Pharmacological treatment options
- Glucocorticosteroids: There is limited evidence proving the effectiveness of medicines in treating alcoholic fatty liver. A gastroenterologist may prescribe glucocorticosteroids to reduce the inflammation of the liver.
Prompt diagnosis and appropriate treatment of Hepatitis B and C can significantly improve outcomes and minimize the risk of liver-related complications.
Non-pharmacological treatment options
- Stopping/quitting alcohol intake: The first line of treatment for alcoholic fatty liver is to stop or quit the intake of alcohol. This condition is called alcohol abstinence; the damage may be reversed if one decreases or stops alcohol consumption, which might take months to years.
- Withdrawal symptoms: After quitting the alcohol, one may experience alcohol-withdrawal symptoms like disturbed sleep, which peak in the first 48 hours since the last intake
- Hepatologists advise reducing the amount of alcohol intake in a planned manner to prevent withdrawal symptoms and provide cognitive behavioural therapy to help with withdrawal symptoms.
- Some patients may need to stay in hospitals and rehabilitation centres initially.
- Nutritional support: Malnutrition is commonly seen in patients with alcoholic fatty disease, so balanced nutrition is highly recommended.
- Avoid salty foods to reduce the risk of swelling in the legs caused by fluid accumulation.
- A damaged liver can’t store glycogen; therefore, the patient’s body depends on muscles to generate energy, leading to muscle wasting and weakness. Hence patients need to consume healthy protein and nutrients.
Surgical treatment
- Liver transplant
- It is a surgery to replace the damaged liver with the healthy liver. In the most severe alcoholic liver disease patients, the liver cannot function properly, leading to irreversible liver failure, where liver transplant is the only treatment for such conditions.
- The surgical hepatologists may consider a liver transplant if the patient is having the following conditions such as:
- Progressive liver failure, despite not consuming alcohol or alcohol abstinence.
- Having a suitable condition to survive a liver transplant.
✅Treatment for fibrosis
Continuous inflammation leads to fibrosis development. Fibrosis progresses into advanced stages if it is not appropriately treated, but in some cases, fibrosis is reversible if it is detected early and know the cause. An essential and very effective treatment for fibrosis is lifestyle modification.
Anti-inflammatory drugs are used to decrease inflammation and stop further progression such as:
- Corticosteroids are used in patients who have autoimmune hepatitis and acute alcoholic hepatitis. These agents act by suppressing inflammatory genes, that results in inflammation.
- Anti-oxidants aid in preventing generation of free radicals, thereby it further prevents oxidative stress, resulting in reduction of liver cell inflammation.
- Antifibrotic therapy is developing, such as Angiotensin, Endothelian inhibitors, PPAR antagonists, and TGF-beta1 inhibitors, which helps in inhibiting the accumulation of fibrogenic cells.
✅Treatment for hepatitis
Yearly, there is 10% to 20% of alcoholic hepatitis patients are likely to advance into cirrhosis; abstinence of alcohol and adequate nutritional support are effective for the management of alcoholic hepatitis patients. Medication treatment for alcoholic hepatitis has been controversial. Corticosteroids are used to reduce inflammation and liver transplantation may be recommended for patients who are not responsive to corticosteroids.
✅Treatment for cirrhosis
Cirrhosis is the advanced stage of fibrosis. Liver cirrhosis treatment depends on the cause and extent of the liver damage. The goals of treatment are to:
- Slow the progression of scar tissue in the liver and
- Treat symptoms and prevent complications of cirrhosis.
The various treatment modalities which can be administered to treat liver cirrhosis are as follows:
- Management of the underlying cause
- Dietary and lifestyle changes
- Immunisation for hepatitis (B or C)
- Reducing the load on the liver
- Managing complications
- Avoiding drug-induced liver injury
- Regular endoscopic procedures
- Monitoring for liver cancer
Medications: Medical management of liver cirrhosis may involve medications such as:
- Beta blockers to reduce hypertension and risk of bleeding.
- Diuretics to remove excess fluid.
- Antiviral drugs to treat viral hepatitis.
- Steroids and immunosuppressive agents to treat autoimmune hepatitis.
Surgical management of liver cirrhosis may be recommended in patients who are suffering with more-severe complications of liver cirrhosis. The following are the few surgical treatments for liver cirrhosis that include:
- Liver transplant
- Shunt surgery
- Liver resection (hepatectomy)
- Copper chelating therapy
- Iron chelation and phlebotomy
It's important to understand that surgical treatment for liver cirrhosis may not be the best option for everyone, as it depends on the following factors such as severity of liver damage, overall patients’ health, and other factors. The gastroenterologist will pay close attention to the patient factors and work with a liver specialist to frame the best treatment plan.
Know More ➡️ Liver Transplant in Hyderabad, India
Frequently Asked Questions (FAQs) on Fatty Liver Disease
Does smoking cause fatty liver?
Yes, smoking can cause fatty liver. Smoking is a recognised cause (risk factor) for fatty liver, characterized by the accumulation of fat in the liver and the potential advancement towards more severe liver inflammation. As per 2022 study, nicotine deposits in the intestine, results in activation of AMPK alpha protein. This protein is responsible for accumulation of lipids and ceramides in the liver, resulting in NAFLD progression .
How to know if you have fatty liver?
Fatty liver disease often lacks noticeable symptoms, causing individuals to be unaware of its presence. However, in some cases, individuals may experience with fatigue, obesity, swelling, jaundice, fluid accumulation in the legs, feet, and abdomen and pain in the upper right area of the abdomen (right upper quadrant pain). These symptoms indicate the presence of liver problems.
Is fatty liver dangerous?
No, fatty liver is not dangerous if treated early. Therefore, early detection plays a crucial role in achieving effective reversal. But, if left untreated, it can progress to an advanced stage known as cirrhosis, which poses significant risks.
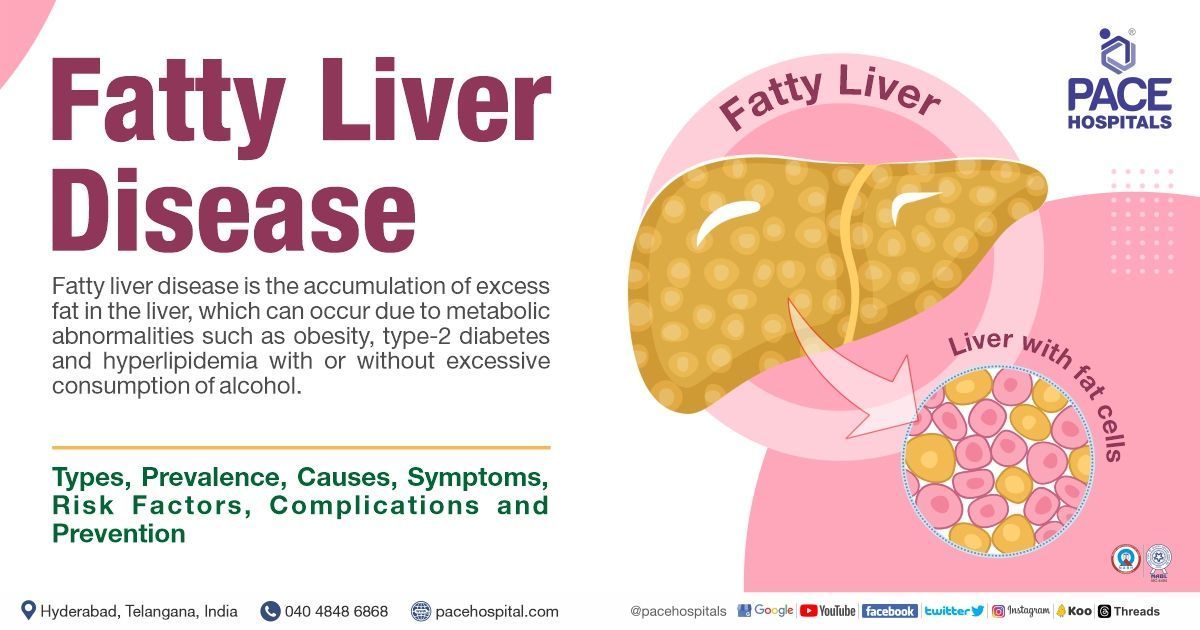
What is fatty liver disease?
Fatty liver disease means the accumulation of excess fat in the liver, which can occur with or without excess alcohol consumption. It is a common hepatic condition associated with metabolic abnormalities such as obesity,
type 2 diabetes, and hyperlipidaemia. Mild fatty liver typically poses no immediate harm, but its progression can result in severe liver impairment, including cirrhosis.
What are the fatty liver signs and symptoms?
The majority of patients with fatty liver do not exhibit symptoms. However, some patients may experience some symptoms including fatigue, abdominal pain Etc. And others may experience different symptoms such as acanthosis nigricans (darkened pigmentation around the neck and joints due to insulin resistance), but if disease progression occurs then, one may experience jaundice, weight loss, loose stools and hepatomegaly.
Does fatty liver cause pain?
No, most patients with the condition do not experience any noticeable symptoms (i.e. asymptomatic). However, in some cases, individuals may present with signs of tiredness or fatigue and pain in the upper right area of the abdomen (right upper quadrant pain).
What are the fatty liver symptoms in female?
Women are more susceptible to developing this condition than men, primarily due to hormonal fluctuations during pregnancy and menopause, polycystic ovary syndrome (PCOS), and the utilisation of oral contraceptives. Women may develop symptoms such as fatigue, swelling in the legs, abdominal pain or discomfort.
Why fatty liver occurs?
Fatty liver can occur due to two primary reasons.
- It arises when the amount of fat in the liver exceeds its capacity to handle or metabolise it effectively, and it is frequently associated with metabolic syndrome, such as obesity, diabetes, and hyperlipidaemia.
- Fatty liver can also develop due to liver cell impairment, which hinders the proper breakdown and processing of the accumulated fat. Various factors contribute to this impairment, including alcohol consumption, starvation, and chronic illnesses.
Does fatty liver cause gas?
Yes, it might cause gas; several studies show a particular relation between excessive intestinal gas and liver steatosis (fatty liver). However, the underlying reasons for this finding and its clinical implications are yet to be fully defined.
What is hepatomegaly with fatty liver?
Hepatomegaly refers to the enlargement of the liver, which can be caused by the accumulation of excess fat in the liver. This condition may or may not manifest with noticeable symptoms. Discomfort or pain can occur in the upper right area of the abdomen, which is a common symptom associated with hepatomegaly and fatty liver.
What is fatty infiltration of the liver?
Fatty infiltration (or fatty liver) of the liver, also known as hepatic steatosis, refers to the accumulation of excess fat within the liver cells. Normally, the liver contains a small amount of fat, but when it reaches 5% to 10% of the liver's weight, it can cause liver problems. Fatty infiltration of the liver can progress to more severe conditions, such as inflammation (steatohepatitis) or liver scarring (cirrhosis) if left untreated.
How many stages of fatty liver?
It is an increasingly recognized fatty liver disease where fat builds up in the liver without excessive alcohol intake. It can lead to significant damage over the years. This condition is further divided into four stages:
- Non-alcoholic Fatty Liver (NAFL)
- Non-alcoholic Steatohepatitis (NASH)
- Fibrosis
- Cirrhosis
Alcoholic liver disease is also divided into 4 stages:
- Alcoholic fatty liver
- Alcoholic hepatitis
- Cirrhosis
Does high cholesterol cause fatty liver?
Yes, high cholesterol can cause fatty liver. The accumulation of triglycerides in the liver is a primary cause of non-alcoholic fatty liver disease (NAFLD). It is important to note that hypercholesterolemia, or high cholesterol levels in the blood, also plays a significant role in the developing NAFLD.
What foods cause fatty liver?
In general, consuming a diet that is high in calories, particularly those derived from trans fats, saturated fats, cholesterol, and fructose-sweetened beverages, can contribute to the accumulation of fat around internal organs (visceral adiposity) and the buildup of fat in the liver, leading to the progression of inflammation of the liver.
These are examples of foods to avoid with fatty liver include Red meat, processed meat, baked and fried foods, sodas, snack foods, full-fat cheese, sweets.
Does fatty liver always lead to cirrhosis?
No, fatty liver always doesn’t lead to cirrhosis. Early detection and proper management of fatty liver (Non-alcoholic and alcoholic) can halt its progression and reduce liver fat accumulation. Implementing timely interventions such as lifestyle changes (healthy diet & exercise), abstaining from alcohol and medical treatments can effectively control NAFLD and alcoholic liver disease.
What is fatty liver in children?
Fatty liver is a hepatic condition characterized by the accumulation of fat in the liver. It is a prevalent disease in obese children. Children with fatty liver are at a higher risk of developing type 2 diabetes. The best way to prevent fatty liver is to control weight and eat a healthy diet.
- Most children are asymptomatic, but some show NAFLD/NASH symptoms like abdominal discomfort (nonspecific) below the rib cage, fatigue, bloating, acid reflux, sleepiness and muscle pain.
- Some might have dark pigmentation in certain body areas such as knuckles, knees, armpits, elbows or neck, as a sign of insulin resistance.
Why liver becomes fatty?
The consumption of excessive calories leads to the accumulation of fat in the liver. An excessive fat buildup occurs when the liver fails to metabolise and process fats as it typically would. Individuals with specific underlying conditions such as obesity, diabetes, or elevated triglyceride levels are prone to developing fatty liver. Additionally, excessive alcohol consumption, rapid weight loss, and malnutrition can contribute to the development of fatty liver.
What stage is after fatty liver?
Non-alcoholic fatty liver disease (NAFLD) can progress through several stages, including fatty liver, steatohepatitis, fibrosis, cirrhosis, and hepatocellular carcinoma.
Starting from uncomplicated fat accumulation (simple steatosis) and advancing to inflamed fatty liver (steatohepatitis), followed by the development of scar tissue (fibrosis) and potentially leading to liver scarring (cirrhosis), and in severe cases, it can progress to hepatocellular carcinoma, a form of liver cancer.
What are the medications to avoid in fatty liver disease?
As per the studies, these drugs induce fatty liver, including corticosteroids, antidepressants, antipsychotics, and antineoplastic agents. Additionally, antiarrhythmics can potentially provoke fatty liver disease and hepatic injury. The relationship between medication-induced fatty liver and the liver's response to weight gain, often associated with certain antidepressants or antipsychotics, remains unclear.
What are the 3 signs of a fatty liver?
The main visible signs in most fatty liver patients include fatigue (tiredness), sudden weight loss, weakness and aching pain in the top right of the abdomen (over the lower right side of the ribs).
Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Hafeezpet, Madeenaguda, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc).

CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
FOLLOW US
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital near me.



