Best Pneumonia Treatment in Hyderabad, India | Expert Lungs Care
PACE Hospitals stands as the leading hospital for pneumonia treatment in Hyderabad, Telangana, India, offering advanced medical technology and a multidisciplinary team of specialists. Our expert pulmonologists and chest specialists provide top-tier care for community-acquired pneumonia (CAP), hospital-acquired pneumonia (HAP), and aspiration pneumonia, ensuring effective treatment and faster recovery.
Early detection is crucial for successful treatment, and at PACE Hospitals, we utilize cutting-edge diagnostic tools such as chest X-rays, blood tests, and sputum analysis to assess the type and severity of pneumonia. Committed to delivering world-class pneumonia care in Hyderabad, we provide specialized treatment for high-risk patients, including elderly individuals, children, and those with chronic lung conditions, asthma, or weakened immune systems.
Book an appointment for Pneumonia Treatment
Pneumonia treatment appointment
Why Choose PACE Hospitals for Pneumonia Treatment?
State-of-the-art Advanced Diagnostic Facilities – CT Scan, MRI Scan
Best Pulmonologists & Chest Specialists in Hyderabad, India
24/7 Emergency & Critical Care Support, Specialized ICU for Severe Pneumonia
Affordable & Reliable Pneumonia Treatment, High-Quality Treatments
Diagnostic evaluation of Pneumonia
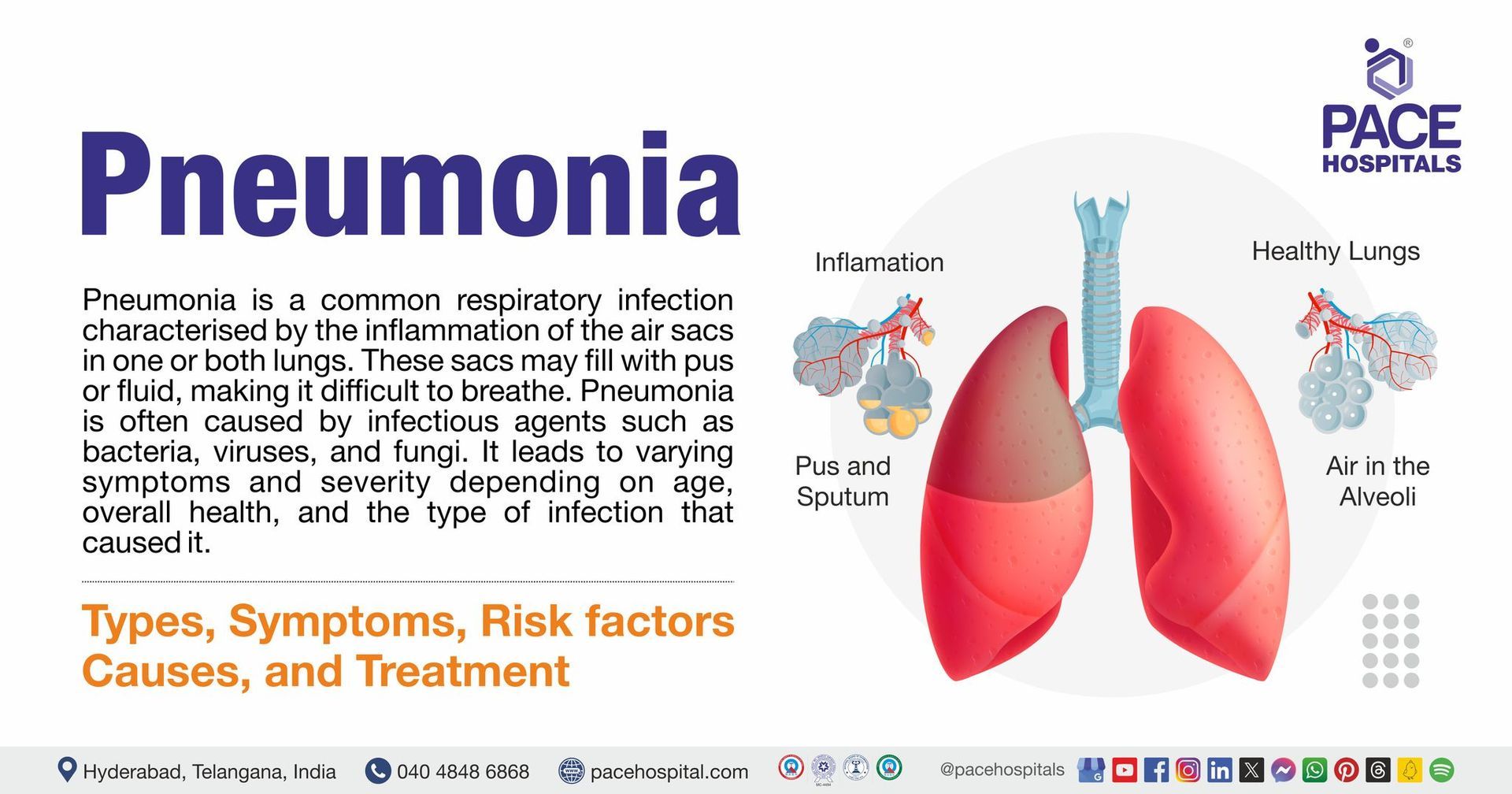
Pneumonia continues to be a major cause of illness and death regardless of advancements in treatment and therapy. Diagnosing pneumonia mainly involves evaluating the patient's clinical signs and symptoms of an acute lower respiratory tract infection, risk factors, and diagnostic tests. A chest X-ray can confirm the diagnosis by showing new areas of infection in the lungs that aren't caused by other conditions, including fluid buildup or a blood clot.
The pulmonologist can make the initial diagnosis and treatment based on the severity assessment and evaluates the following before selecting the appropriate tests to diagnose pneumonia:
- The presented signs and symptoms
- Age, family history, and general health of the suspected patient
- Medical and medication history
- Results of previous medical tests
- Physical Examination
The presented signs and symptoms: Individuals with pneumonia may present with a productive cough (with mucus or phlegm) or dry cough, fever, chills, generalised weakness, and sharp, pleuritic pain that worsens with coughing or deep breathing, often associated with shortness of breath. These symptoms are specific to lung infections and may be associated with certain complications.
Signs and symptoms more frequently seen in older adults include falls, decreased appetite, or functional impairment. A change in mental status should prompt evaluation for an infectious cause. Hence, pulmonologists always consider the possibility of pneumonia in any adult or child presenting with acute-onset fever or chills, cough, and the above-mentioned other symptoms.
Age, family history, and general health of the suspected patient: Pneumonia can affect all ages people. However, babies and children who are 2 years old or younger are at increased risk because their immune systems are still developing, and older adults, aged 65 or older, are also at increased risk because their immune systems generally weaken as they age.
The pulmonologist considers the age, family history, and overall health of the suspected patient to evaluate the potential risks and guide diagnostic testing. Habits including smoking cigarettes and consuming alcohol can cause trouble clearing mucus from airways and weaken the immune system. Hence, pulmonologists review patients' habits to estimate their risk of pneumonia. Recent hospitalisation or ventilation is a significant concern, especially with mechanical ventilation.
Medical and medication history: Pulmonologists will review the medical and medication usage history of patients because having a history of lung diseases, including asthma, COPD, bronchiectasis, cystic fibrosis, brain disorders such as stroke, and other serious conditions, including heart failure and diabetes, can increase the risk of pneumonia.
In modern health care settings, concurrent consumption of several drugs, including antipsychotic drugs (APs), anticholinergic drugs, opioid analgesics, antidepressants, and cancer chemotherapeutic and immunosuppressive agents, raises the pneumonia risk, especially in older populations, has also more generally been associated with increased rates of hospitalisation and earlier death.
Knowing the medication history can help the pulmonologist monitor its effects and decrease the risk and complications of pneumonia.
Results of previous medical tests: A pulmonologist may ask about reports of earlier medical tests to obtain valuable information to confirm the presence of lung infections or pneumonia in a patient and to choose the proper diagnosis and treatment.
Physical Examination: After reviewing the signs, symptoms, risk factors, and medical and medication history of the patient, the pulmonologist inspects the following to evaluate objective anatomic findings, to assess respiratory symptoms and evaluate signs of infection or complications:
Auscultation (the act of listening to the sounds of the heart, lungs, arteries and abdomen)
- Vital signs: Tachycardia (fast heart rate) or bradycardia (slow heart rate), fever or hypothermia, hypoxia (low oxygen saturation) and hypotension
- Breathing: Dyspnoea (difficulty breathing), wheezing (may be noted in some cases, especially in viral or aspiration pneumonia), and crackles
- Chest sounds: Decreased or bronchial breath sounds, dullness on percussion, and crackles in the lungs can be heard over the affected lung.
- Other: Tactile fremitus (vibration felt on chest during speech), egophony (abnormal voice sounds on auscultation, "E" becomes "A"), pleural friction rub (rough sound due to inflamed pleura), and cyanosis (bluish discolouration of skin due to low oxygen).
On examination, the signs may include:
- Fever of > 38°C
- Raised respiratory rate
- Focal chest signs: decreased entry of air, dullness on percussion, decreased chest expansion, crackles and bronchial breathing (none, some, or all of these may be present).
✅Pneumonia diagnosis
After completing the initial assessment, the pulmonologist proceeds with further testing, if needed, based on the severity of the illness and the person's risk of complications. The following are diagnostic tests that pulmonologists may advise to diagnose pneumonia:
- Imaging tests
- Chest X-ray
- Chest CT scan
- Ultrasound
- MRI
- Laboratory blood tests:
- Complete Blood Count (CBC)
- Procalcitonin
- C-reactive Protein (CRP)
- Blood Cultures
- Oxygen Saturation and Respiratory Function Tests
- Pulse Oximetry
- Arterial Blood Gas (ABG)
- Microbiological tests
- Sputum Culture
- Urine Antigen Tests
- Polymerase Chain Reaction (PCR) Test
- Pleural fluid culture
- Minimally invasive procedures
- Bronchoscopy
- Thoracentesis
Imaging Tests
- Chest X-ray: This is the key diagnostic test for pneumonia. It looks for the location and extent of inflammation in the lungs. It shows the areas of infiltrates or consolidation to distinguish pneumonia from other conditions, such as cancer or heart failure. Common patterns include lobar consolidation (bacterial pneumonia), interstitial patterns (viral pneumonia), and patchy infiltrates (atypical pneumonia).
- Chest CT scan: This common imaging procedure combines computer technology and X-rays to produce sharp, detailed horizontal or axial images (often called slices) of the body. The CT scan is more detailed than regular X-rays. It provides clear images of any body part, including the lungs and shows airways in detail, identifying pneumonia and its complications, such as pleural effusions, abscesses, multilobar pneumonia, etc.
- Ultrasound of the chest: It may be used if fluid surrounding the lungs is suspected to determine the amount of fluid present and its cause.
- MRI of the chest: MRI is applicable for diagnosing pneumonia among adult outpatients with lower respiratory tract infections. While CT scans are superior to MRI in diagnosing pneumonia in immunocompromised patients, MRI remains a significant imaging technique for follow-up in these patients, reducing the risk of ionising radiation exposure. Generally, MRI is not used to assess for pneumonia but to examine the chest wall structures, heart, and vessels. In some cases, such as such as when there is fluid, a tumor, or infection in the lungs, MRI offers additional insights into these abnormalities.
Laboratory blood tests
Blood tests are suggested to determine whether infection is present and whether it has spread to the bloodstream.
- Complete Blood Count (CBC): Elevated white blood cell count (leucocytosis) may suggest a bacterial infection, though it can be be normal or only mildly elevated in viral pneumonia.
- Procalcitonin: This biomarker helps differentiate between bacterial and viral infections. Elevated levels suggest a bacterial cause.
- C-reactive Protein (CRP): Another inflammatory marker, though it is not specific to pneumonia.
- Blood Cultures: Performed in severe cases or when the patient is immunocompromised to identify the causative organism.
Oxygen Saturation and Respiratory Function Tests
- Pulse Oximetry: Pulse oximetry is a tiny machine that measures the amount of oxygen in the blood by placing the sensor on the finger.
- Arterial Blood Gas (ABG): This test assesses the patient's oxygenation (the amount of oxygen and carbon dioxide) in the blood, acid-base status, and adequacy of ventilation and is typically used in severe cases of pneumonia. This test can help determine the proper treatment for a patient's breathing problems. Such as such as determining whether supplemental oxygen is needed for severe hypoxia (low oxygen levels).
Microbiological tests
- Sputum Culture: This test is performed on sputum (material coughed up from the lungs and into the mouth) and is often used to check for an infection in the lungs and detect the causative organism, particularly in severe or complicated pneumonia cases.
- Urine Antigen Tests: This non-invasive laboratory test detects antigens from pathogens in urine, including Streptococcus pneumoniae and Legionella pneumophila. These antigens help identify bacterial causes in patients with severe pneumonia.
- Polymerase Chain Reaction (PCR) Test: It detects viral pathogens, including respiratory syncytial virus (RSV) or influenza.
- Pleural fluid culture: This test examines which bacteria are causing pneumonia by taking a fluid sample using a long, thin needle from the pleural space (the space between the chest wall and lungs).
Minimally invasive procedures
- Bronchoscopy: This is a direct exam of the lungs' airways (bronchi) using a flexible tube known as a bronchoscope, helping to evaluate and diagnose lung problems, assess blockages, and take out tissue and fluid samples for testing.
- Thoracentesis: Thoracentesis may be performed in cases of suspected pleural effusion (fluid in the pleural cavity) to drain the fluid and identify the pathogen. It is carried out by removing a small sample of pleural fluid (about 60mL [2 ounces]) to determine the cause and guide healthcare professionals in selecting the best treatment.
✅Pneumonia differential diagnosis
The following conditions can mimic pneumonia and should be considered in the differential diagnosis:
- Chronic Obstructive Pulmonary Disease (COPD) exacerbation
- Asthma
- Pulmonary Embolism (PE)
- Pulmonary oedema
- Bronchiolitis
- Pleurisy
- Congestive Heart Failure (CHF)
- Lung Cancer
- Tuberculosis (TB)
- Interstitial Lung Disease (ILD)
If differentiation becomes difficult, parameters such as C-reactive protein (CRP), leucocyte count, procalcitonin levels, erythrocyte sedimentation rate (ESR), and body temperature can be checked to establish a diagnosis.
✅Stages of pneumonia
Pneumonia, which can be viral or bacterial, occurs in four stages: congestion, red hepatization, grey hepatization, and resolution.
- Congestion: The first stage usually lasts about 24 hours. The lungs may look red from increased blood flow and swelling of the lung tissue. Symptoms include coughing, fatigue, fever, chest pain, and a wet cough with sputum (phlegm).
- Red hepatization: The second stage usually lasts a few days. Red cells, white cells, bacteria, and cellular debris can clog the lung airways. Symptoms include worsening symptoms, weakness or tiredness, decreased sputum production, coughing, and shortness of breath. The affected lung becomes more dry, airless and granular, and resembles the consistency of the liver.
- Grey hepatization: This more severe phase, which can last up to 8 days. The lung looks grey or yellow in colour but still has the consistency of the liver. Symptoms include shortness of breath, swelling in the alveoli and fibrous strands around the alveoli.
- Resolution: This is the final recovery stage and occurs over 8-10 days. Symptoms improve, and patients begin to feel better as inflammatory fluids and damaged cells in the lungs start to disappear.
Pneumonia treatment
Pneumonia treatment depends on the causative organism (bacterial, viral, or fungal), the patient's age, comorbidities, severity of the disease, and clinical condition. At first, healthcare professionals use simple scoring systems to help distinguish between patients who may need intensive care and those who can be managed at home with simple treatments.
The Pneumonia Severity Index (PSI) evaluates 20 variables to classify patients into one of five risk categories (I–V) based on their risk of death within 30 days.
The British Thoracic Society introduced another assessment tool similar to the PSI in 2003. It calculates the risk of 30-day mortality but only uses five variables, including confusion, urea, respiratory rate, blood pressure, and age >65 (CURB65). One point is awarded for each if present, making the tool easier to use.
CURB65 and CRB65 help identify high-risk patients. A score of 0 or 1 defines a low risk of mortality and indicates that a patient can be managed in ambulatory care (outpatient setting). A score of 3 or higher suggests hospital admission. When making treatment decisions, healthcare professionals consider the patient's social circumstances and treatment preferences.
Pneumonia Treatment approaches:
- Conservative management
- Antibiotics
- Supportive Care
- Antiviral Therapy
- Antifungal Therapy
- Chest Physiotherapy
- Minimally invasive approaches
- Surgical management
Effective treatment of lung infections depends on the rapid and accurate detection of the offending pathogen.
Conservative management of pneumonia
Antibiotics: The type of antibiotic depends on the likely cause of the infection and the patient's risk factors. Empiric antibiotic therapy will be started as soon as pneumonia is suspected and tailored later based on culture results:
- Community-Acquired Pneumonia (CAP)
- Outpatient Treatment: This typically involves macrolide or tetracycline antibiotics. A respiratory fluoroquinolone or a beta-lactam plus macrolide is used for patients with comorbidities or regions with high resistance.
- Local resistance patterns should guide the treatment of CAP when available. In previously healthy patients who are appropriate for outpatient treatment, the recommended first-line treatment is a macrolide antibiotic that targets the most common causal pathogen, S. pneumoniae.
- Patients with comorbidities such as diabetes, chronic heart, lung, renal, or liver disease, alcoholism, asplenia, impaired immune system, or recent antibiotic use within the last 3 months have an increased risk for drug-resistant S pneumoniae. As such, a respiratory fluoroquinolone or b-lactam plus a macrolide is recommended.
- Klebsiella pneumoniae treatment includes a 14-day course of a third or fourth-generation cephalosporin or a respiratory quinolone.
- Inpatient Treatment: For moderate to severe cases, a combination of beta-lactam and a macrolide, or fluoroquinolone alone, is recommended.
- Hospital-acquired Pneumonia (HAP): Hospital-acquired pneumonia (HAP) is treated with a combination of antibiotics (targeting multi-drug-resistant organisms (e.g., MRSA and Pseudomonas), oxygen, and sometimes a ventilator. Generally, 7 days of treatment with appropriate antibiotics is recommended for uncomplicated ventilator-acquired pneumonia (VAP) and hospital-acquired pneumonia (HAP). If the illness is more severe, HAP is managed in the hospital ward or the intensive care unit (ICU).
- Atypical Pneumonia (Mycoplasma, Chlamydia, Legionella): Atypical pneumonia treatment involves macrolides or tetracycline antibiotics for milder cases. In more severe cases, fluoroquinolones may be used. Antibiotics are usually given for two weeks or more, even if the patient feels better. Stopping antibiotics too soon can make the reoccurrence of pneumonia making it harder to treat
Supportive Care
- Oxygen Therapy: Oxygen therapy is widely used to treat lung diseases. If the patient is hypoxic (oxygen saturation < 90%), supplemental oxygen is administered via nasal cannula or face mask and can be continued for one to two weeks or until the patient can get enough oxygen from the air without effort. Mechanical ventilation may be required in severe pneumonic cases. The effectiveness of oxygen therapy for pneumonia is not well known. One review found that non-invasive ventilation may be more effective than standard oxygen supplementation.
- Hydration: Adequate fluid intake is essential for patients with pneumonia because it can help loosen mucus in the lungs, prevent dehydration, and speed recovery.
- Analgesia: If pleuritic chest pain is present, NSAIDs or acetaminophen are recommended for pain relief.
Antiviral Therapy
- For viral pneumonia (e.g., influenza), antiviral medications are suggested to reduce the duration of illness within 48 hours of symptom onset. They are also used in suspected cases of viral pneumonia due to herpes simplex virus (HSV).
- COVID-19: Supportive care and antivirals for moderate to severe cases.
Antifungal Therapy
- Treatment depends on the type of fungi, often requiring long-term antifungal therapy. Antifungal treatments are mainly recommended in immunocompromised patients or those at risk for fungal pneumonia (e.g., Histoplasma, Coccidioides, or Aspergillus infections).
- Azole and polyene antifungal drugs will be recommended depending on the suspected pathogen.
Chest Physiotherapy: In cases with thick mucus or large amounts of sputum, chest physiotherapy or postural drainage may help clear the lungs.
Minimally invasive approaches
- Drainage: In patients with significant pleural effusion or abscess, drainage is recommended to remove fluid often using tube or catheter.
- Thoracentesis: This minimally invasive procedure removes fluid from the pleural space using a needle.
- Intubation and Ventilation: For severe pneumonia with respiratory failure or shock, endotracheal intubation and mechanical ventilation may be required.
Surgical management of pneumonia
Although most patients with pneumonia do not require surgery, it may become necessary if complications arise, such as lung abscesses or empyema. Surgical interventions may include:
- Drainage: Severe cases of pneumonia complicated by abscess formation can be treated with drainage via a percutaneous catheter or surgical intervention.
- Lobectomy or Pneumonectomy: In rare cases, surgical resection of the affected lung tissue may be required when pneumonia results in significant lung destruction.
- Thoracotomy: During this procedure, surgeons make an incision to open the chest and view the lungs so that damaged and dead lung tissue can be removed.
Monitoring and Follow-up
A follow-up X-ray may be needed to ensure the resolution of pneumonia, especially if a complication like an abscess or pleural effusion is present. Previous Infectious Diseases Society of America (IDSA) guidelines recommended chest radiography as the standard method for diagnosing CAP.
Frequently Asked Questions (FAQs) on Pneumonia Treatment
What helps pneumonia heal faster?
Rest, staying hydrated, and following the pulmonologist-prescribed treatment (antibiotics for bacterial pneumonia or antivirals for viral pneumonia) can help to heal faster. Breathing treatments, humidifiers, and avoiding smoking or air pollutants can also help with recovery.
How to prevent pneumonia in babies?
To prevent pneumonia in babies, ensure they receive their vaccinations, including the pneumococcal vaccine. Avoid exposure to sick individuals, maintain good hygiene practices like handwashing, and avoid second-hand smoke, which can increase the risk of respiratory infections.
Does smoking cause pneumonia?
Yes, smoking damages the lungs and weakens the immune system, making the body more susceptible to infections like pneumonia. It also slows the healing process and increases the risk of complications in those with pneumonia.
Why do I have pneumonia?
Pneumonia can occur due to various causes, including bacterial, viral, or fungal infections. Risk factors include smoking, weakened immune system, age (young children or elderly), chronic illnesses, or exposure to harmful pathogens. The infection leads to lung inflammation, causing fluid and pus buildup in the alveoli, impairing normal breathing.
Is pneumonia viral or bacterial?
Both viral and bacterial infections can cause pneumonia. Bacterial pneumonia (e.g., from Streptococcus pneumoniae) is typically more severe, while viral pneumonia (e.g., from influenza or respiratory syncytial virus) can range from mild to moderate in severity.
How does pneumonia progress?
Pneumonia typically starts with symptoms such as fever, cough, chills, and shortness of breath. If left untreated, symptoms can worsen, leading to severe problems. Inflammation in the lungs can spread, resulting in complications, such as septic shock, respiratory problems, and pleural abscesses, especially in older people or those with pre-existing health issues.
How can pneumonia affect your health?
Pneumonia can cause severe respiratory problems, leading to low oxygen levels, fatigue, and difficulty breathing. In some patients, it can lead to complications, such as lung abscesses, sepsis, or respiratory failure, especially in vulnerable populations, including the elderly and those with chronic illnesses.
When should I get vaccinated to prevent pneumonia?
Vaccination is recommended for people of different ages. For children, vaccines like the PCV13 (Pneumococcal Conjugate Vaccine) should be included in their regular immunisation schedule. Adults aged 65 and older are recommended to receive PPSV23 (Pneumococcal Polysaccharide Vaccine), and individuals with certain chronic conditions may require it earlier. Smoking adults and those with weakened immune systems may also benefit from pneumococcal vaccination.
What is Streptococcus pneumoniae treatment?
Streptococcus pneumoniae infections are treated with antibiotics. Other antibiotics, like cephalosporins or macrolides, are suggested if the strain is resistant. However, severe cases may require intravenous antibiotics and hospitalisation.
What not to do when you have pneumonia?
If symptoms worsen or don't improve, seeking medical attention is needed, and completing the prescribed antibiotic course is essential. Smoking worsens lung function and delays healing. Always follow the healthcare professional's (pulmonologist) treatment plan.
Can pneumonia come back?
Yes, pneumonia can recur if the initial infection isn't completely treated or the immune system is compromised. It can also reappear if the individual is exposed to new bacteria or viruses.
What is severe pneumonia treatment?
Severe pneumonia treatment includes intravenous antibiotics, oxygen therapy, and sometimes mechanical ventilation if the patient has trouble breathing. Hospitalisation is often required for patients with severe symptoms, and supportive care (e.g., fluids, pain relievers) is provided.