Dengue Fever Treatment
in Hyderabad, India
PACE Hospitals, is renowned for its excellence in Dengue fever treatment in Hyderabad, India; delivering compassionate care and optimal outcomes. Our expert team of infectious disease specialists and healthcare professionals are dedicated to diagnosing and managing dengue fever effectively with advanced medical technology, we tailor personalized treatment plans for patients of all ages, ensuring comprehensive care and speedy recovery from Dengue fever.
Request an Appointment for Dengue Fever Treatment
Dengue fever treatment - appointment
Why Choose PACE Hospitals for Dengue Fever Treatment?
PACE Hospitals is widely recognized as the best hospital for dengue treatment in Hyderabad, offering a comprehensive and personalized approach to patient care. Our team of highly skilled and experienced medical professionals is dedicated to providing the highest level of care to every patient. We understand that dengue can be a serious and life-threatening illness, which is why we ensure that our patients receive the most effective and efficient treatment possible. Whether you are experiencing mild symptoms or require more intensive care, you can trust us to provide you with the best dengue treatment in Hyderabad.
Our state-of-the-art facilities are equipped with the latest diagnostic tools and treatment options, allowing us to quickly and accurately diagnose and treat dengue fever. We offer a range of services, including inpatient and outpatient care, 24/7 emergency services, and access to specialized dengue care teams.
46000+ Patients treated with dengue fever
Precision & Cost effective Dengue Fever Treatment
Team of the Best general physician doctors
All insurance accepted with No-cost EMI option
Dengue is the most common arthropod-borne virus in the world, spread by mosquitoes and posing a serious threat to global health. This condition is also referred to by different terminologies including "breakbone" or "7-day fever." It is accompanied by severe joint pain, severe muscle cramps, and a high fever that reflects the extent and duration of symptoms. Dengue fever can sometimes be severe and can cause death, even though the majority of cases are asymptomatic.
Based on the onset of symptoms, the diagnostic procedure to be carried out in patients are differentiated as Acute phase with 0-7 days onset of symptoms and convalescent phase with more than 7 days of symptoms onset.
Acute phase of dengue fever: first 0-7 days post onset of symptoms
Within the first seven days, the serum samples are tested, and laboratory diagnosis should be made using either of the following test combinations:
- NAAT test/ nucleic acid amplification test like RT-PCR and an Immunoglobulin-M antibody test (IgM) or
- Nonstructural protein 1 (NS1) antigen test and detection test of Immunoglobulin-M antibody test (IgM)
- A serum sample test
Interpretation guidelines:
- A test positive for NAAT does not require any further testing of confirmation as this test would detect dengue virus RNA in serum, plasma and blood. Most of these tests would also identify the serotype of infecting dengue virus.
- If nonstructural protein 1 is found in serum during the first 7 days of disease, it indicates an ongoing or recent dengue infection. Usually, the use of commercial NS1 tests and its interpretation of a positive result varies.
- Physician can not rule out the possibility of infection if RT-PCR or NS1 tests negative.
- If RT-PCR or NS1 tests positive, it is a dengue virus as per the standard definition of national notifiable disease surveillance system (NNDSS)
Convalescent phase of dengue fever: Greater than 7 days after onset of symptoms
A convalescent serum sample can be obtained and evaluated in cases when acute (0-7 days) sample is not available or tested negative.
- The primary test after 7 days of onset of symptoms is IgM ELISA. However, a few patients may test positive on NAAT or NS1 antigen test even after 7 days of infection.
- IgM antibody test should be performed to detect IgM antibodies in case of 3 months or longer after infections.
Interpreting test results
- Patients who have a confirmed acute dengue virus infection are those who have a positive NAAT (such as RT-PCR) or NS1 test.
- Patients are considered to have a presumed recent dengue virus infection if they show IgM antibodies against the virus in a single sample.
- Patients are currently infected with dengue if their matched sample results (first taken during the first seven days of sickness, and second sample taken after symptoms have subsided) show a shift from negative to positive IgM.
Dengue fever diagnosis
Physicians should consider the possibility of dengue in fever patients who reside in or visited recently the areas with high risk of dengue. Other than fever, common symptoms might include intense headache, pain in the cavities behind the eyes (retro-orbital pain), muscle pain (myalgia) and joint pains. Nonstructural protein 1 (NS1) and Immunoglobulin M (IgM) or nucleic acid amplification test (NAAT) and immunoglobulin M (IgM) tests should be ordered for acute diagnosis of dengue disease. In dengue suspected cases, physicians should start related management, instead of waiting for confirmatory results of dengue diagnostic test.
In order to ascertain if the recent ill health of a patient is associated with dengue virus, the physician must review:
- Past medical history of the patient
- Correlation of patient’s residence or recent travel history
- History of immunization (especially for dengue, yellow fever and encephalitis)
Few diagnostic tests available to determine the virulence of dengue fever are:
- IgG testing
- Molecular testing
- NS1 antigen testing
- IgM antibody test
- Plaque reduction neutralization test
IgG testing
- Serologic testing with IgG in a single specimen is not advised for the diagnosis of acute dengue in patients because it may identify antibodies from previous dengue infections or other flavivirus infections.
- Patients are considered to have current dengue infections if their IgG results in paired samples (the first taken during the first seven days of illness, and the second taken after symptoms have subsided) change from negative to positive.
Molecular tests
- For the first 0–7 days of the illness, dengue virus RNA may typically be found using molecular testing in individuals who exhibit symptoms of the virus. Molecular testing might not be as sensitive after day 7.
NS1 antigen tests
- During the acute stage of dengue virus infections, NS1 can be found. In the first 0–7 days after onset of symptoms, NS1 testing can be just as sensitive as molecular testing. NS1 tests might not be as sensitive after day 7.
IgM antibody test
- After the third day of sickness, IgM antibody testing can detect the majority of recent dengue infections. These tests should be run on samples with negative NS1 and PCR results, particularly after day 3 of illness. Interpreting positive IgM results is complicated because of cross-reactivity with other flaviviruses, like Zika.
Plaque Reduction Neutralization Tests
- Plaque Reduction Neutralization Tests (PRNT) can help identify the causative virus in some situations and can also be used to resolve false-positive IgM antibody results resulting from non-specific reactivity. However, PRNT might not be able to confirm a significant percentage of IgM positive results in regions with high dengue and Zika virus neutralizing antibody prevalence.
✅Diagnosis of dengue in special cases
The dengue virus can be diagnosed in slightly different approach of tests in few exceptional cases for those living in areas with flavivirus and dengue together, pregnant women etc.
Areas with co-circulating flaviviruses
- Plaque reduction neutralization test (PRNT) must be ordered by doctors for individuals residing in or visiting regions where flaviviruses are concurrently prevalent in order to rule out dengue on IgM-positive specimens. When ruling out dengue by PRNT, other flaviviruses such as Zika, Japanese encephalitis, St. Louis encephalitis, West Nile, and yellow fever viruses should be considered.
- A definitive diagnosis result is not usually obtained by PRNT, especially in patients who have previously been exposed to multiple flaviviruses. There is no cross-reactivity between dengue molecular tests (such RT-PCR) and NS1 testing and other flaviviruses of concern.
Pregnant people
Test for Zika should be done in addition to dengue test if the patient is pregnant, symptomatic, and resides in or has visited a region at risk for the virus.
✅Dengue fever stages
The 3 phases of dengue fever include
- Febrile
- Critical
- Recovery stage
The febrile phase of dengue
- High-grade fever: Sudden onset of high-grade fever can be seen in the individuals during the febrile phase, that could rise up to 40°C lasting for around 2 to 7 days. Saddleback or biphasic fever can occur in about 6% of cases, especially in patients who have severe dengue fever and dengue hemorrhagic fever. Usually, the fever lasts for at least 24 hours before rising again for at least one more day.
- Symptomatic phase: Facial flushing, skin erythema, myalgias, arthralgias, headache, sore throat, conjunctival injection, anorexia, nausea, and vomiting are associated symptoms during this period. Within one to two days of the fever starting and again on the last day, skin erythema appears as a generalized, blanchable macular rash. On the other hand, a second maculopapular rash could appear within a day.
The critical phase of dengue
- Defervescence: It occurs between days 3 and 7, indicates a time during the critical phase when the temperature usually drops to about 37.5 to 38 °C or lower. This stage usually lasts one to two days and is linked to increased capillary permeability.
- Stage of leukopenia: Prior to the critical period, the platelet count frequently drops rapidly and the hematocrit levels rise. Leukopenia can also develop up to 24 hours prior to a decline in platelet count and the emergence of warning symptoms. The critical phase can develop into shock, organ failure, disseminated intravascular coagulation, or bleeding if treatment is not received.
Dengue fever recovery phase
The extravascular fluid is gradually reabsorbed over the course of two to three days during the healing period. Patients frequently have bradycardia at this time.
✅Diagnostic evaluation of dengue fever
Elevated aspartate aminotransferase levels, leukopenia, and thrombocytopenia are common laboratory findings. Clinical evaluations classify the disease as
- Probable dengue
- Severe dengue
- Warning signs of dengue
- dengue shock syndrome.
Probable dengue: The patient should have visited or resided in Dengue-endemic region. Fever and two or more of the following symptoms like leukopenia, myalgias, arthralgias, rash, nausea, vomiting, and rash are present.
Severe dengue: Severe dengue is associated with dengue fever along with severe plasma leakage, hemorrhage, altered consciousness, cardiac dysfunction, lung dysfunction, organ failure, transaminitis greater than 1000 IU/L.
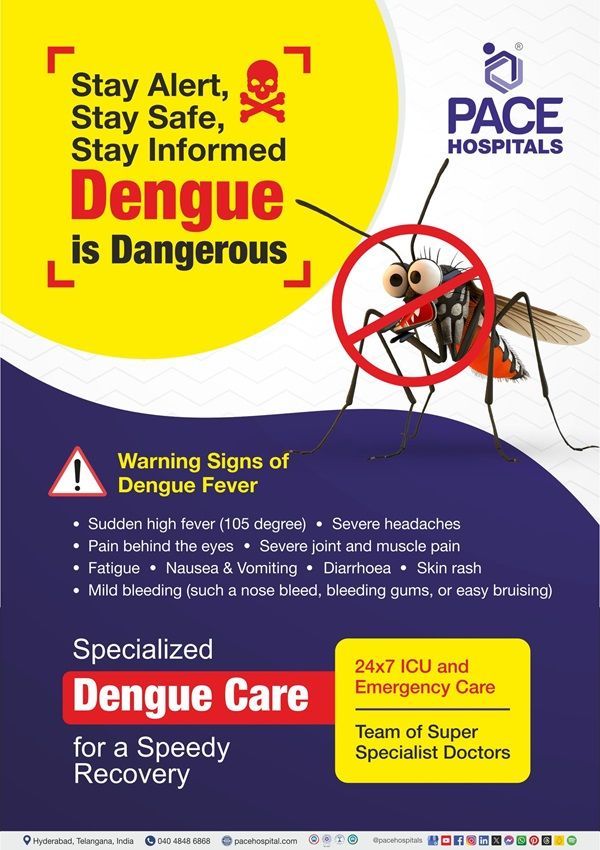
Warning signs of dengue: The symptoms of dengue include thrombocytopenia, fatigue, mucosal bleeding, ascites or pleural effusion, recurrent vomiting, abdominal pain, and an increase in hematocrit and thrombocytopenia.
Dengue shock syndrome clinical warnings: Rapidly rising hematocrit, severe abdominal pain, continuous vomiting, and low or nonexistent blood pressure are among the symptoms.
✅Dengue differential diagnosis
As there are many diseases that display similar kind of clinical signs and symptoms of dengue fever, it is often challenging to diagnose dengue. A Few differential diagnoses include:
- Measles
- Ebola virus
- Leptospirosis
- Influenza
- Zika virus disease
- West Nile infection
- Chikungunya
- Malaria
- Yellow fever
Acquiring a comprehensive medical history including vaccinations, travel, and exposures is essential for diagnosing dengue fever. Serological testing and the identification of the NS1 antigen are necessary for the quick laboratory diagnosis of the dengue virus. Only a few days after infection may, serological testing be useful, and they may result in false positives from other Flavivirus illnesses such as Zika or yellow fever.
✅Considerations of physician while treating dengue
The clinical considerations of a physician while treating dengue would be based on the severity of the disease.
Dengue clinical management
- Using EPA-registered insect repellent, dressing in long sleeves and long pants, and adopting other preventive measures when traveling can help tourists from contracting dengue by keeping themselves safe from mosquito bites.
- In most cases, dengue is a minor disease. But in around 5 percent of instances, it can worsen into a serious condition that is accompanied by significant bleeding, shock, or organ damage.
- In patients who are left untreated, the death rate from dengue can reach up to 13%. Unrecognized or prolonged shock, undetected bleeding, and subsequent infections are common causes of death.
- Fever, headache, myalgias, arthralgias, retroorbital pain, nausea, vomiting, and rash or petechiae are among the common symptoms of dengue. After a period of five to seven days of incubation, symptoms appear suddenly. A fever could last for two to seven days.
Severe dengue
- Defervescence lasts one to two days and indicates the start of the critical phase, where temperature rises to 38.0°C or 100.4°F.
- Doctors should keep a watchful eye out for any warning indicators that point to the development of severe dengue. It is necessary to assess these patients for either inpatient care or observation.
- Prolonged vomiting, intense abdominal pain, mucosal bleeding, postural hypotension, pleural effusion, ascites, lethargy/restlessness, liver enlargement, and a steadily rising hematocrit are all warning signs.
Testing and treatment
- Within seven days of the onset of symptoms, patients with dengue-like symptoms can be examined using both IgM antibody testing and nucleic acid amplification assays (NAAT). Test only with IgM antibody testing after 7 days from the start of symptoms.
- The mainstream of treatment includes intravenous (IV) hydration therapy and management of complications. Frequent monitoring of vital signs and hematocrit levels is necessary for the management of hospitalized dengue patients in order to assess the severity of the disease and response to fluid replacement therapy.
- There aren't any vaccines to prevent dengue or specific antivirals that are advised for treating the illness at this time.
✅ Dengue complications and management
- Cardiac Complications: Due to a significant risk of congestive heart failure and pulmonary edema, dengue patients with myocarditis and cardiogenic shock require extremely cautious fluid resuscitation followed by an early start of inotropic medications.
- Hepatitis and Liver Failure: Hepatocytes experience apoptosis as a direct result of the dengue virus's cytopathic impact. also has a role in Dengue hemorrhagic fever-related liver damage.
- Acute Kidney Injury: In addition to the direct consequences of dengue virus and immune-mediated damage, hypoperfusion, rhabdomyolysis, and hemolysis can cause renal impairment in dengue.
- Respiratory Complications: Therapeutic pleural fluid drainage may be necessary in rare cases if a child's severe pleural effusion prevents them from being able to breathe on their own. Pleural tap should be avoided in cases of dengue.
Dengue treatment
The treatment of dengue fever includes managing viral symptoms, complications, and providing symptomatic treatment based on the diagnosis and symptoms.
Dengue hemorrhagic fever fluid management
- The most severe form of dengue hemorrhagic fever, known as dengue shock syndrome (DSS), is characterized by an apparent increase in vascular permeability.
- The quick restoration of the circulating plasma volume is the primary objective of dengue shock syndrome treatment.
- When it comes to treating patients with refractory shock, the World Health Organization's initial 1975 recommendations suggested replacing lost volume with crystalloid solutions first, then with colloids. Extravasated fluid is drawn back into circulation by colloids because they prolong their half-life in the blood and raise colloid oncotic pressure.
- It has been suggested that in order to achieve the same level of resuscitation, substantially larger amounts of crystalloids must be infused than colloids; nevertheless, doing so may result in fluid excess or pulmonary edema.
Transfusion of blood products in dengue fever
- Whether or not to transfuse platelet products to a specific dengue patient is an often-perplexing question for doctors who treat dengue patients. The platelet inventory is in danger due to the exponential increase in demand for platelet concentrates that follows most dengue epidemics.
- Furthermore, bleeding tendencies can happen in kids with normal platelet counts as well as ones that don't always correspond with them. This emphasizes the necessity of elucidating the indications for platelet transfusions in patients with thrombocytopenic dengue who have either minor or significant bleeding or overt bleeding. There are a number of reasons why dengue can result in thrombocytopenia.
- Bone marrow suppression with reduced megakaryocyte maturation
- Platelet destruction at the peripheral level by phagocytosis, antibody-mediated destruction, and complement cascade activation.
Prophylactic platelet transfusion in dengue
Prophylactic platelet transfusion did not significantly improve supportive treatment alone, nor did it stop bleeding or speed platelet recovery in a number of studies conducted on adult dengue patients. Patients with severe dengue and pediatric dengue patients require more evidence.
Platelet transfusion in patients with minor and major bleeds
- According to research, platelet transfusion boosted the absolute platelet count by 50%–100% in dengue patients with thrombocytopenia-related bleeding; however, it had no discernible effect on clinical bleeding and did not strengthen the clot as measured by thromboelastography (TEG).
- Adult dengue patients with thrombocytopenia and either no bleeding or minimal hemorrhage demonstrate that platelet transfusion is related with significant adverse responses rather than preventing the progression of bleeding to severe bleeding or shortening the time it takes to stop bleeding.
- There is not enough data available at this time to support or refute the advantages of platelet transfusion for dengue patients who are bleeding. If the patient has an acute, severe mucosal bleed that cannot be managed with supportive therapy, the majority of units will transfuse platelets.
Immature platelet fraction in dengue
The reticulated platelets in peripheral blood are measured by the immature platelet fraction. This is the indicator of bone marrow recovery, like the reticulocyte count for red blood cells. As a result, a higher immature platelet fraction suggests a higher marrow thrombopoiesis rate. Compared to mature platelets, newly released platelets are larger and more efficient physiologically. In the next 72 hours, platelet recovery is predicted by an IPF cutoff level of less than 10%.
Platelet micro-particles
- Phospholipid membrane vesicles generated from tiny cells are known as micro-particles (MPs). Activated platelets are the source of platelet micro-particles (PMPs), which have similar properties to platelets.
- Compared to individuals who experienced bleeding symptoms, several investigations revealed noticeably higher PMP levels in dengue patients with thrombocytopenia who did not experience bleeding. This led to the hypothesis that the procoagulant impact of PMPs may have protected these patients; PMPs may also function as a biomarker to determine whether to administer prophylactic platelet transfusion.
✅Anti-dengue drugs
- As of today, no antiviral medication is authorized for the management of dengue. Nonetheless, a number of potentially effective anti-DENV medications are presently undergoing human testing and are in different phases of research.
- Further research is being conducted, but experiments conducted in vitro and in vivo on an Indian group of people have shown that Cocculus hirsutus may have anti-dengue properties. Anti-DENV action has been discovered in compounds obtained from marine microorganisms, such as Microbulbifer variabilis C-03 and Streptomyces gougerotii GT.
✅Anti-dengue vaccines
The lack of a specific anti-viral treatment for dengue makes the development of an anti-dengue vaccination an important goal. As of right now, there are five different kinds of dengue vaccines being developed:
- Live, Attenuated
- Inactivated
- Recombinant subunit
- viral- vector
- DNA vaccines.
The live, attenuated vaccines (CYD-TDV, TAK-003, and TV003/005) are the ones that are most advanced in development. At the moment, only one dengue vaccine is available for sale: the CYD-TDV brand.
Preventing mosquito bites and avoiding endemic areas are the primary ways to avoid getting dengue virus.
Frequently Asked Questions (FAQs) on Dengue fever
What are the symptoms of dengue?
The commonly seen symptoms of dengue fever include high fever, headache, pain behind the eye cavities, joints pain, muscle pain, rashes, mild to moderate bleeding (such as nose, gum bleeding or easy bruising and low count of white blood cells.
When should a dengue patient be hospitalized?
Patients experiencing severe symptoms of dengue, such as intense abdominal pain, continuous vomiting, fast breathing, bleeding gums, exhaustion, restlessness, or blood in the vomit, should be admitted to a hospital.
How long does recovery from dengue take?
Although fatigue and weakness may last for several weeks following the acute phase of the illness, recovery from dengue can take a few weeks.
Can dengue be transmitted from person to person?
Direct person-to-person transmission of dengue is not possible. The bite of an Aedes mosquito carrying the infection transmits it.
What is "dengue shock syndrome"?
A severe case of dengue known as "dengue shock syndrome" is marked by a sharp drop in blood pressure that eventually results in shock. Medical attention must be given right away.
How is dengue diagnosed?
Blood tests that identify the virus, viral RNA, or antibodies made in reaction to the infection are used to diagnose dengue.
What are the main components of dengue treatment?
The mainstay of treatment is supportive care, which includes staying hydrated, using acetaminophen (paracetamol) for pain and fever, and keeping an eye out for symptoms of severe dengue.
What are the recommendations for maintaining hydration?
To stay hydrated, patients should consume a lot of liquids, such as juices, water, and oral rehydration treatments. In severe situations, intravenous (IV) fluid therapy may be necessary.
What is the difference between IgM and IgG antibody tests?
IgM antibodies typically surface within the first week of sickness and are indicative of a recent dengue infection. IgG antibodies develop later, usually beyond the first week, and they signify a prior infection or a subsequent illness.
Why is early diagnosis of dengue important?
Early identification is essential for appropriate treatment and monitoring to avoid repercussions, especially in severe cases that might advance quickly.