Deep Vein Thrombosis (DVT) Treatment in Hyderabad, India
PACE Hospitals is recognized as the best hospital for DVT Treatment in Hyderabad, Telangana, India, provide comprehensive and advanced treatment for Deep Vein Thrombosis with a focus on accurate diagnosis, expert care, and patient safety. Our team of highly experienced vascular specialists ensures early detection and effective management of DVT to prevent serious complications like pulmonary embolism.
We offer state-of-the-art diagnostic facilities, including Doppler ultrasound, CT venography, and blood tests, to accurately assess the severity of the condition. Our treatment options include anticoagulant therapy, thrombolysis, IVC filter placement, and minimally invasive procedures, tailored to each patient’s needs. With 24/7 emergency care, cutting-edge medical technology, and a multidisciplinary approach, we ensure fast recovery, reduced risk of recurrence, and long-term vascular health.
Book an Appointment for DVT Treatment
Deep vein thrombosis treatment (DVT) - appointment
Why Choose PACE Hospitals for Deep Vein Thrombosis (DVT) Treatment in Hyderabad?

State-of-the-art Facilities, Advanced Diagnostics
Team of Best Vascular Specialists in Hyderabad
24/7 Emergency Care & Post-Treatment Support
Affordable & Reliable DVT Treatment
Deep Vein Thrombosis (DVT) Diagnosis
Usually, the diagnosis is done by the physician based on the patient's condition and criteria. Accurate diagnosis is the main key for finding the patient's exact condition or illness, starting with interaction of patient-interventional cardiologist followed by physical examination and diagnostic measures.
The interventional cardiologist considers the following before selecting the appropriate tests to diagnose deep vein thrombosis:
- When patients enter the hospital, the physician/interventional cardiologist typically takes a medical history and asks about their symptoms before recommending a Doppler ultrasound for deep vein thrombosis (DVT) within 24 hours.
- A physical examination by a physician/interventional cardiologist helps identifies the symptoms.
Note: The main veins that are prone to DVT in legs and arms are distal veins, popliteal veins, femoral veins, common femoral veins, and ileac veins.
DVT physical exam
- Limb edema, which may be unilateral or bilateral, develops if the thrombus travels to the pelvic veins.
- Enlarged veins and warmed up red skin.
- Tenderness (pain upon touch)
The physician/interventional cardiologist asks about the following:
- Pain (which is typically present in 50% of patients)
- Redness
- Swelling, which 70% of patients often experience.
After completing the physical examination, the physician/interventional cardiologist may assess the DVT condition using the Wells' Scoring System.
Wells' Criteria (Score)
The probability of DVT influences how to investigate using the Wells Scoring System. It determines the clinical probability of DVT in the initial stage.
- Patients who score 0 to 1 have a low clinical probability, whereas those score 2 or more have a high clinical chance.
- If a patient gets a DVT score of 2, the interventional cardiologist may perform an ultrasound of the proximal leg vein within four hours. In case of negative result, a D-dimer test may follow.
- Upon performing the test, the physician/interventional cardiologist may administer a temporary 24-hour dosage of a parenteral anticoagulant if imaging cannot be performed within 4 hours. Within 24 hours, an ultrasound of the proximal leg vein need be done.
- If the D-dimer test is positive and the proximal leg vein ultrasound is negative, the physician/interventional cardiologist suggests an ultrasound after 6 to 8 days.
- If the D-dimer test is positive, the patient does not have a Wells score DVT of 2. The patient may be recommended to have a proximal leg vein ultrasound scan within 4 hours, or if this is not possible, the patient may be advised to get an interim 24-hour dosage of a parenteral anticoagulant. Within 24 hours of a request by a physician, an ultrasound of the proximal leg vein is performed.
- If the proximal leg vein ultrasonography is positive, the physician/interventional cardiologist treats for DVT.
The diagnostic tests and vascular evaluation for DVT patients include:
- CBC (complete blood count): The complete blood count tells the count of each specific type of blood cell in the body. It is done to identify the signs of infection and identify factors related to blood clotting.
- D-Dimer blood test: This blood test is used to identify the presence of a clot (thrombus) in the body.
- Doppler ultrasound examination: Based on the sound waves, this test provides images of blood flow in the area with blood clots.
- Pelvic MRI (magnetic resonance imaging): Pelvic MRI is a non-invasive procedure that provides images of soft tissues, bones, and blood flow to identify the blood clots in the pelvis.
- Anti-thrombin-III: Anti-thrombin-III is responsible for preventing excess coagulation in the body. The levels of Anti thrombin-III confirm the presence of clots in the body.
- Lupus-related problems (autoimmune disease-related problems): Anti-phospholipid antibodies and lupus anticoagulants attack the body's cells.
- Genetic testing: Genetic tests are used to check for mutations that make people more susceptible to developing blood clots, such as the prothrombin G20210A mutation or the Factor V Leiden mutation.
- Protein-C and Protein-S: Levels of protein C and protein S, help the body control clotting.
- Computed tomography venography (CVT): This test can thoroughly assess venous issues in the pelvis and abdomen and find additional potential causes of leg swelling.
Therefore, CTV can be a helpful test for patients undergoing rehabilitation, not only for quickly detecting DVT but also for evaluating the various diagnoses of leg edema.
✅Stages of Deep Vein Thrombosis (DVT)
Understanding the stages of DVT is crucial to implementing effective management strategies and reducing the risks associated with this condition. The following categories describe the disease's severity:
- Provoked DVT: It occurs because of acquired conditions such as malignancy (cancer), recent trauma, oral contraceptive use, lengthy immobilization, or obesity. These factors enhance the likelihood of clot formation by causing venous stasis or modifying blood coagulation.
- Unprovoked DVT: It occurs without clear external causes and is frequently associated with endogenous or idiopathic (unknown) parameters. This kind has a higher chance of recurrence if anticoagulant therapy is discontinued, emphasising the need for close monitoring as well as additional treatment.
- Proximal DVT: It involves clots that form above the knee, particularly in the iliofemoral or femoral veins, and it is more prone to cause serious outcomes like pulmonary embolism.
- Distal DVT: It refers to clots that form below the knee and are often considered less dangerous; nevertheless, they still require attention because they can lead to proximal DVT if not treated.
✅Differential diagnosis of DVT
A differential diagnosis is a list of possible medical conditions or diseases that may share the same symptoms in a person. This list provides a theory about what might be causing the symptoms, rather than final confirmation. The physician will arrange tests to rule out any possible diseases on the differential diagnosis list after providing patients with a list of potential illnesses. The diagnosis of the patient will be confirmed through these tests.
DVT differential diagnoses are as follows:
- Budd-Chiari syndrome: The rare condition known as Budd-Chiari syndrome (BCS) is characterised by hepatic venous outflow blockage. It may be located along the venous route, from the hepatic venules to the inferior vena cava (IVC) junction and right atrium. The obstruction may be thrombotic or non-thrombotic.
- Cellulitis: A typical bacterial skin infection called cellulitis makes the skin around the infected area red, swollen, and painful. It can spread and lead to major health issues if left untreated.
- Baker’s cyst: Popliteal cysts, often called Baker's cysts, are one of the most common knee conditions. The condition is characterised by a lump formed by fluid-filled cysts at the back of the knee, frequently resulting in stiffness and discomfort. The illness uses the name of Dr William Morrant Baker, a surgeon who originally identified it in the 19th century.
- Dependent edema: Venous insufficiency, which typically gets worse with elevation and dependency, is more likely to cause dependent edema.
- Pulmonary embolism (PE): PE is a condition where the portion of a blood clot in DVT passes through the bloodstream to the lungs. People can recover from this condition if the clot is minor, and the proper treatment is received. If a bigger clot dislodges and obstructs the blood from reaching the lungs, it may lead to death finally.
- Hepatic disease: A combination of regional and general prothrombotic variables is required for thrombosis, which is a complex process. Liver cells produce protein C, protein S, and antithrombin. Therefore, liver failure causes these inhibitors' levels to drop. This occurs even in people with liver damage that is not easy to recognize due to portal vein thrombosis (PVT).
- Trauma: Any injury to the veins may lead to the obstruction of blood flow or blockage and resembles DVT in clinical conditions.
- Heart failure: The medical condition known as congestive heart failure (CHF) carries a significant venous thromboembolism (VTE) risk. Thrombosis by venography is seen in 10% to 22% of hospitalised CHF patients without thromboprophylaxis (DVT prophylaxis).
- Septic thrombophlebitis: Suppurative (septic) thrombophlebitis is used to characterise vein thrombosis in an inflammatory and infectious condition. A thrombus that is connected to swelling and the production of pus (suppuration), both in the venous wall and around the vessel, is the characteristic that distinguishes this illness.
- Nephritic syndrome: Haematuria, high blood pressure, reduced urine production, and edema are the clinical symptoms of nephritic syndrome, which is caused by glomerulus inflammation, which is the main underlying pathology. It results in a quick onset of proteinuria, white blood cells in the urine, and the emergence of red blood cells (RBCs) and blood cells. The fundamental pathology may originate in the kidney or be a systemic disease complication.
- Post-thrombotic syndrome (PTS): PTS can lead to edema, discomfort, skin discolouration or redness, and various other problems. It makes the skin more vulnerable to cellulitis, an infection that can enter the circulation, resulting in sepsis and death.
- Congenital vascular abnormalities: About 1% of all births result in congenital vascular malformations (CVM). Congenital vascular abnormalities are a condition of bleeding or lymph fluid leakage, pooling under the skin, and forming painful lumps, which can range from flat, basic birthmarks to complicated, three-dimensional abnormalities deep within the body. They may comprise lymph vessels, arteries, veins, or a combination. Although they are typically present at birth, it is rare that they will be passed on from parent to child or that anyone will have more than one.
✅Considerations of an interventional cardiologist in treating DVT
When treating deep vein thrombosis (DVT), interventional cardiologists examine some aspects to ensure appropriate management and reduce the likelihood of complications. Here are some important considerations:
- Assessment of risk: Interventional cardiologists will assess the risk of pulmonary embolism (PE) using clinical prediction approaches, such as the Wells score, to guide diagnostic tests and treatment options.
- Patient comorbidities: Interventional cardiologists will evaluate the patient's overall health, including any existing illnesses (e.g., renal dysfunction or cancer) that may impact treatment options.
- Anticoagulant therapy: Interventional cardiologists will consider contraindications to anticoagulant therapy, such as active bleeding or prior surgery, which may need alternate treatment options.
- IVC filters: Interventional cardiologists will consider mechanical procedures such as inferior vena cava (IVC) filters for patients who are incapable of taking anticoagulants or have recurrent DVT despite management.
✅ DVT treatment Goals
- The major goal in treating DVT is to prevent the clot from growing larger and breaking off to form a pulmonary embolus (PE).
- Other goals of treatment include
- Preventing the clot from becoming bigger
- Preventing new blood clots from forming
- Preventing long-term complications.
Deep Vein Thrombosis (DVT) Treatment
DVT treatment aims to prevent pulmonary embolism, lessen morbidity, and lower the risk of post-thrombotic syndrome.
Anticoagulation is the mainstay of therapy. Only proximal DVT (not distal) and patients with pulmonary emboli should be treated, according to The National Institute For Health and Care Excellence (NICE) DVT treatment guidelines. The benefits and hazards of DVT anticoagulation must be compared for each patient.
Deep vein thrombosis treatment is as follows:
- Anticoagulants: Anticoagulants are most frequently prescribed to treat DVT or PE, also known as "blood thinners." Despite being referred to as blood thinners, these drugs do not thin the blood. They reduce the blood's ability to clot, lowering the chance of creating more clots and preventing the clot from growing as the body gradually reabsorbs it.
Contraindication: Usage of anticoagulants causes bleeding. Before usage, clear monitoring is needed for unusual bleeding in the patients.
- Thrombolytics: Thrombolytics (also known as "clot busters") function by dissolving the clot.
Contraindication: Careful patient selection is essential since administering thrombolytic treatment can cause an intracranial bleed.
- Xa inhibitors: These recent drugs can be easy to administer and work like anticoagulants.
Contraindication: They may not be suitable for everyone because it might be challenging to prevent excessive bleeding.
- Compression stockings: If there are no contraindications, below-knee graded compression stockings for DVT with an ankle pressure greater than 23 mm Hg need to be recommended for two years.
The surgical and minimally invasive procedures for DVT are as follows:
- Endovascular procedures: A large blood clot can be removed (thrombectomy) by surgeons, interventional cardiologists, or interventional radiologists using small tools. These methods can be applied to inject clot-busting medications or to clean a vein.
- Stenting: Stents, which are tiny metal tubes that can hold open the vein, can be inserted by surgeons, interventional cardiologists, and interventional radiologists. With the help of these tubes, surgeons can place stents in the iliac veins in the leg or pelvis to treat DVT in various parts of the body.
- Vena cava filter placement: Placing a filter in the vena cava, the body's largest vein, is done by a physician/interventional cardiologist. Blood clots are stopped in their tracks by this filter before they can reach the lungs.
Contraindication: In cases of acute DVT, inferior vena cava filters are not advised. Both permanent and transient inferior vena cava filters are accessible. These devices have little effect on survival; however, they may lower the rate of recurrent DVT. These filters should only be inserted in individuals with a greater risk of bleeding and contraindications to anticoagulation.
- Thrombectomy/Embolectomy: It may occasionally be necessary to do DVT surgery (deep vein thrombosis surgery) to remove the clot. The goal of thrombectomy is to remove the clot from a DVT patient. In a pulmonary embolic patient, embolectomy may be performed to remove the blockage in the lungs caused due to the clot.
Frequently Asked Questions (FAQs) on Deep Vein Thrombosis (DVT)
How do you get deep vein thrombosis?
DVT results from reduced or blocked blood flow in the veins because of blood vessel damage from surgery or trauma, blood vessel inflammation due to various risk factors such as injury, obesity, age greater than 60, being immobile (motionless) for a long time, pregnancy, dehydration, hormone replacement therapies, inserting venous catheters etc.
What are 3 signs of DVT?
The three signs of DVT are:
- Throbbing pain (to beat or pulsate with increased force) in the leg,
- Occurrence of swelling in one leg (rarely in both legs), and
- Warm skin surrounding the painful area (tenderness in the swollen veins).
Which leg is more common for DVT?
A study was done on the DVT associated with an elevated risk of left-side compression and finally concluded that greater than 70% compression may be associated with an increased risk of left-sided DVT when compared to the right side.
What is the most serious complication of deep vein thrombosis?
The most serious complication of deep vein thrombosis is pulmonary embolism (PE). If the blood clot from a deep vein thrombosis (DVT) travels to the lungs through the bloodstream, it is known as a pulmonary embolism (PE). People can recover from this illness if the clot is minimal, and the appropriate treatment is given.
Finally, death may occur if a larger clot becomes dislodged, preventing blood from reaching the lungs.
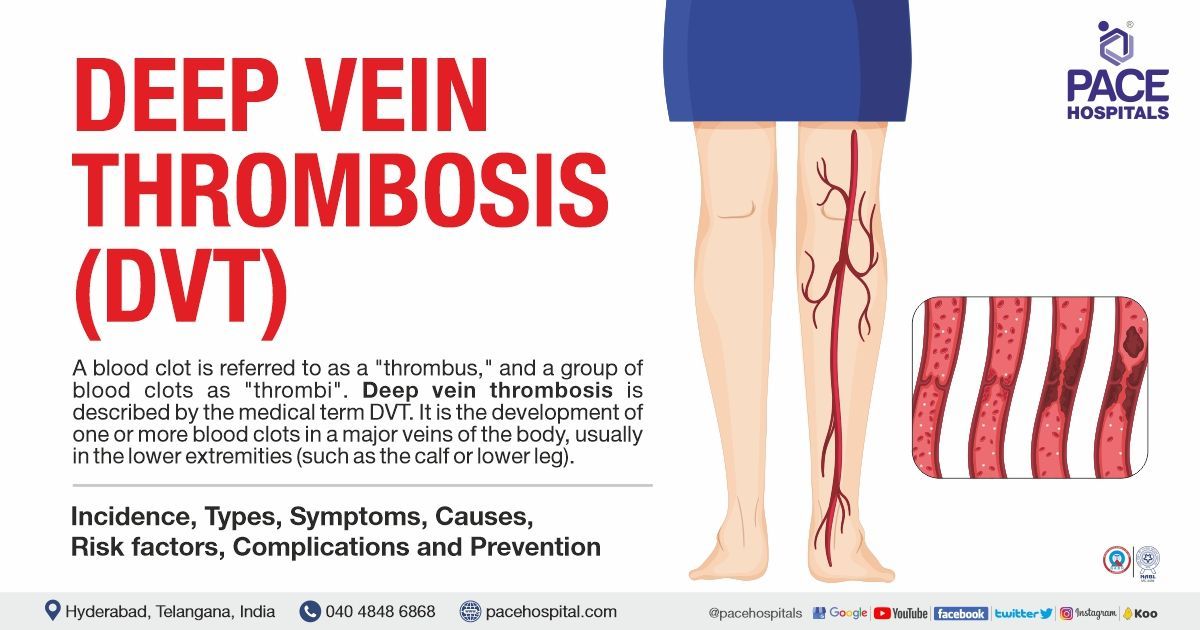
What is deep vein thrombosis DVT?
Deep vein thrombosis is also termed as DVT. DVT is the development of one or more blood clots in a body's major vein, typically in the lower extremities (such as the calf or lower leg). Accordingly, some patients may have pain, swelling, discomfort, discolouration, redness in the affected area, and maybe warm-to-the-touch skin. The clots may entirely or partially limit blood flow in the vein.
What are the 5 warning signs of a blood clot?
“STOP the CLOT” is a fantastic method to remember the 5 warning symptoms of a blood clot.
STOP stands for:
S- Swelling in the arm or leg
T- Tenderness,
O- Out of breath
P- Passing out or lightheaded
CLOT stands for:
C-Chest pain
L- Leg discolouration
O- Overdrive on heart racing
T- Time to call for an emergency
What age is at risk for DVT?
According to the studies, individuals older than 60 are more prone to venous thrombosis. The incidence of a first symptomatic venous thrombosis (VT) in the general population is 1-2 per 1,000 people yearly. Nearly 8 per 1,000 people aged 85 and older had VT, compared to about 1 per 10,000 people aged 25 to 30.
90% of the population's thrombosis incidence can be attributed to ageing, according to the population-attributable risk, which is greater than 90%. Up to 15% of people can develop VT during their lifetime (cumulative incidence) until they are 90 years old, while people over 70 account for about 60% of all VT incidents.
Is walking good for a DVT?
Studies have shown that in patients with acute DVT, early walking exercise is safe and may assist in lowering the initial symptoms. DVT treatment and exercise training may reduce or prevent post-thrombotic syndrome in patients with a history of DVT by not worsening leg symptoms.
Can deep vein thrombosis cause a stroke?
No, heart attacks and strokes are not caused by DVT. The nature and location of the clot determine how it affects the body.
There are two primary categories of blood clots:
- Deep vein thrombosis (DVT) clots: Here, the blood clot occurs in a deep vein of the leg, pelvis, or occasionally in the arm. This kind of blood clot does not cause heart attacks and strokes.
- Arterial thrombosis clots Blood clots in an artery, typically in the heart or brain. Heart attack or stroke can result from this form of blood clot.
Although both forms of clots can result in major health issues, there are differences in their causes and preventative measures.
Can varicose veins cause deep vein thrombosis?
Yes, there is a slight risk of blood clots in the deep veins if the patient has significant varicose veins. Blood clots require immediate medical attention as it causes swelling and redness. Blood clots can also develop in the arms or other body parts.