Gastric Polyps - Symptoms, Causes, Types, Diagnosis, Treatment
Gastric polyps are abnormal mucosal or submucosal growths in the stomach, often detected incidentally during endoscopy. They can be benign, precancerous, or malignant, with common types including fundic gland polyps (FGPs), hyperplastic polyps (HPs), and adenomatous polyps. Less common types include carcinoid tumors and mesenchymal lesions like GISTs. Risk factors include H. pylori infection, chronic inflammation, PPI use, and genetic disorders. Most are asymptomatic but may cause bleeding or obstruction. Diagnosis requires endoscopic evaluation and histopathology for proper management.
Gastric polyp definition
Luminal lesions that protrude above the mucosal surface are commonly referred to as gastric polyps. These lesions are typically asymptomatic and small, and they are often found incidentally during endoscopic examinations or while diagnosing anaemia, gastrointestinal haemorrhage, or signs of stomach outlet obstruction.
Gastric polyps meaning
The word polyp is derived from the Greek word "polypus", which means "many-footed", and "gastric", which means "stomach". The term gastric polyp does not explain any specific aetiology but is merely descriptive.
It can be used to identify any pedunculated stomach tumor, regardless of its histologic nature, and has been applied to describe neoplasms, hyperplasia, and edematous formations. While a lot of benign stomach tumors can resemble polyps, most of them are adenomas.
Prevalence of gastric polyps
Although the prevalence and distribution of gastric polyps varies greatly throughout sources, which revealed that between 2% to 6% of individuals undergoing endoscopy had gastric polyps.
Gastric hyperplastic polyps account for 17% to 42% of those, fundic gland polyps for 37% to 77%, adenomas for 0.5% to 1%, and malignant neoplasms for roughly 1% to 2%. The fundus is where gastric polyps are most frequently discovered, and the prevalence rises with advancing age.
The prevalence distribution greatly varies between genders as males are more likely to have adenoma, while females are more likely to have fundic polyps.
Incidence of gastric polyps
Gastric polyps are benign lesions that extend into the gastrointestinal cavity and have a broad base or pedicle. Nonetheless, the probability of gastric polyps transforming into malignant tumors varies based on the polyp's pathology, with an overall malignant transformation incidence of 0.4–10%.
Reducing the risk of malignant cancer requires both active intervention and early diagnosis. The incidence of gastric polyps is rising every year due to changes in people's diet and lifestyle, which also substantially raises the risk of cancer.
Fundic gland polyps are slowly replacing hyperplastic polyps as a significant type of gastric polyp such that between 2000 and 2010, the percentage of fundic gland polyps increased from 8.8% to 66.1%, while the rate of hyperplastic polyps decreased from 48.5% to 20.8%.

Gastric polyps types
Based on the characteristics of the polyps, gastric polyps are majorly divided into:
- Epithelial polyps
- Mesenchymal polyps
Epithelial polyps are again sub divided into:
- Fundic gland polyps
- Hyperplastic polyps
- Adenomatous polyps
- Gastric neuroendocrine tumors
Mesenchymal polyps are further classified as:
- Inflammatory fibroid polyps
- Gastrointestinal stromal tumors
Epithelial polyp
Epithelial polyps are the most frequent type of gut polyps. Some prominent epithelial polyps are adenomatous polyps, hyperplastic polyps, and fundic gland polyps, each linked to a specific set of clinical contexts. Other less common epithelial lesions that can manifest as polyps are neuroendocrine tumors (formerly known as carcinoids).
Fundic Gland Polyps
- Gastric fundic gland polyps are among the most frequently discovered stomach polyps (47%), showing up in 0.8% to 23% of endoscopies.
- These polyps occur in three different clinical contexts: syndromic polyps (familial adenomatous polyposis [FAP] syndrome), polyps linked to proton pump inhibitors (PPI) use, and sporadic polyps.
Hyperplastic Polyps
- After fundic gastric polyps, hyperplastic polyps are the second most prevalent type of gastric polyp. The phrase "inflammatory polyp," sometimes used inappropriately to refer to this polyp, should be avoided as it can be mistaken for an inflammatory fibroid polyp (IFP), which requires different management.
- Less than 2 cm in diameter, sessile or pedunculated, hyperplastic polyps commonly form in the antrum, though they can occur anywhere. Inflammatory conditions like reactive or chemical gastritis, H pylori gastritis, chronic gastritis, and pernicious anaemia are closely linked to gastric hyperplastic polyps.
Adenomatous Polyps
- As a precursor to stomach cancer, gastric adenomas, also known as gastric polypoid dysplasia, are real neoplasms. Their histological classification follows that of colon adenomas, with tubular, villous, and tubulovillous variations.
- They are usually solitary and can be found anywhere in the stomach. However, they are most frequently found in the antrum. From an endoscopic perspective, they are typically sessile or fat instead of pedunculated.
Gastric Neuroendocrine Tumors (Formerly Carcinoids)
- By immunohistochemistry, enterochromaffin-like cells (of which 90% are found in the corpus and fundus) stain with either synaptophysin or chromogranin-A are the main component of the majority of gastric neuroendocrine tumors.
- In the stomach, there are four different types of carcinoids, each with a unique prognosis and course of treatment. This specific tumor demonstrates the significance of performing simultaneous biopsies of the background fat mucosa.
Mesenchymal polyps
Mesenchymal lesions broadly represent tumors generated from mesoderm. These polyps are usually found beneath the surface epithelium, giving the appearance of a nodule rather than polypoid. They can be found in the mucosa or submucosa. Some of the common mesenchymal polyps are gastrointestinal stromal tumors and inflammatory fibroid polyps.
Inflammatory fibroid polyps
- Inflammatory fibroid polyps typically manifest as nodules or polypoid lesions. These histologically distinct lesions originate in the submucosa and are characterised by edema, inflammatory cells (primarily eosinophils), and spindle and stellate stromal cells that are CD34 positive.
- These are usually tiny (<1.5 cm) and sessile lesions that appear in the stomach pylorus or distal antrum.
Gastrointestinal Stromal Tumors
- Gastrointestinal stromal tumors represent 1% to 3% of all malignant gastric tumors and are rare connective tissue tumors originating in the muscularis propria.
- During upper endoscopy procedures carried out for non tumor related symptoms, the gastrointestinal stromal tumors are found often. The anatomic location, dimension, and aggressiveness of the cancer can all affect the clinical characteristics of this tumor.
Gastric polyp symptoms
Over 90% of stomach polyps are unintentionally discovered during endoscopy, most of which are asymptomatic. Though most of the gastric polyps are asymptomatic, the prominently observed symptoms are:
- Dyspepsia: Persistent discomfort in the upper abdomen, often accompanied by bloating, nausea, or early satiety.
- Heartburn: A burning sensation in the chest due to acid reflux, commonly seen in polyps associated with chronic gastritis.
- Gastrointestinal Bleeding: Polyps may ulcerate, leading to symptoms like melena (dark stools) or hematemesis (vomiting blood).
- Anemia: Chronic blood loss from ulcerated or inflamed polyps can cause a decrease in hemoglobin levels, leading to fatigue and weakness.
- Gastric Outlet Obstruction: Large polyps, particularly in the pyloric region, may block food passage, causing nausea, vomiting, and weight loss.
- Iron Deficiency: Occurs due to chronic occult blood loss from bleeding polyps, leading to fatigue, pallor, and brittle nails.
Causes of Gastric Polyps
There are wide range of causative factors that contribute to gastric polyps. Mostly the causes are distinguished based on the type of gastric polyp.
Fundic Gland Polyps (FGPs)
- Commonly associated with chronic proton pump inhibitor (PPI) use, leading to increased gastrin secretion and fundic gland hyperplasia.
- Frequently found in patients with familial adenomatous polyposis (FAP) due to APC gene mutations, which drive abnormal cell proliferation.
Hyperplastic Polyps
- Hyperplastic polyps develop as a result of chronic gastric inflammation, often triggered by Helicobacter pylori (H. pylori) infection or chronic gastritis.
- Persistent mucosal irritation stimulates epithelial regeneration, increasing the risk of polyp formation and potential malignant transformation.
Adenomatous Polyps (Gastric Adenomas)
- These are precancerous lesions caused by dysplastic changes in the gastric epithelium, often found in patients with atrophic gastritis and intestinal metaplasia.
- Strongly associated with APC gene mutations and familial adenomatous polyposis (FAP), leading to uncontrolled cell proliferation and an increased malignancy risk.
Inflammatory Fibroid Polyps (Vanek’s Tumor)
- The inflammatory fibroid polyps are rare, benign lesions of unknown exact cause, though often linked to chronic irritation and reactive hyperplasia of connective tissue.
- Many cases show mutations in the PDGFRA gene, leading to excessive fibrous tissue growth and inflammatory infiltration.
Gastric Carcinoid Tumors (Neuroendocrine Tumor Type I)
- These develop due to chronic hypergastrinemia, which stimulates enterochromaffin-like (ECL) cell proliferation and small neuroendocrine tumor formation.
- Commonly associated with autoimmune atrophic gastritis and pernicious anemia, where chronic inflammation leads to gastric mucosal atrophy.
Juvenile Polyps (Hamartomatous Polyps)
- The juvenile polyps frequently occur in hereditary syndromes such as Peutz-Jeghers syndrome and Juvenile Polyposis Syndrome, which affect cell growth regulation.
- Caused by mutations in SMAD4 or BMPR1A genes, leading to abnormal tissue differentiation and excessive polyp formation.
Other Rare Causes
- Gastric Xanthomas – Benign accumulations of lipid-laden macrophages in areas of chronic gastritis, often mistaken for polyps.
- Lymphoid Polyps – Reactive hyperplasia of lymphoid tissue, typically found in association with chronic infections or immune responses.
- Gastrointestinal Stromal Tumors (GISTs) – Rare tumors arising from interstitial cells of Cajal, often driven by KIT or PDGFRA gene mutations.
Risk Factors for Gastric Polyps
- Chronic Gastric Inflammation – Persistent inflammation from H. pylori infection or autoimmune gastritis promotes epithelial changes, increasing polyp risk.
- Prolonged PPI Use – Chronic suppression of gastric acid secretion leads to hypergastrinemia, stimulating fundic gland hyperplasia and polyp formation.
- Genetic Syndromes – Conditions like FAP, Peutz-Jeghers syndrome, and Juvenile Polyposis Syndrome significantly increase the likelihood of polyp formation.
- Smoking & Alcohol – Long-term exposure to tobacco and alcohol damages the gastric mucosa, leading to dysplastic changes and an increased polyp risk.
- Dietary Factors – High consumption of salt, nitrosamines, and processed foods can contribute to chronic gastric irritation and polyp development.
Gastric Polyps Complications
- Bleeding: Polyps may ulcerate, leading to gastrointestinal bleeding, hematemesis, or melena.
- Perforation: Large or ulcerated polyps can weaken the stomach wall, causing perforation and peritonitis.
- Infection: Infected polyps may result in localized gastric inflammation, abscess formation, or sepsis in severe cases.
- Cancer: Adenomatous and hyperplastic polyps carry a risk of malignant transformation into gastric cancer.
- Ileus: Large polyps may impair gastric motility, leading to delayed gastric emptying and paralytic ileus.
- Obstruction: Polyps near the pylorus or duodenum can block food passage, causing nausea, vomiting, and weight loss.
- Tumors:
Some polyps, particularly adenomas and neuroendocrine tumors, can progress to malignant neoplasms over time.
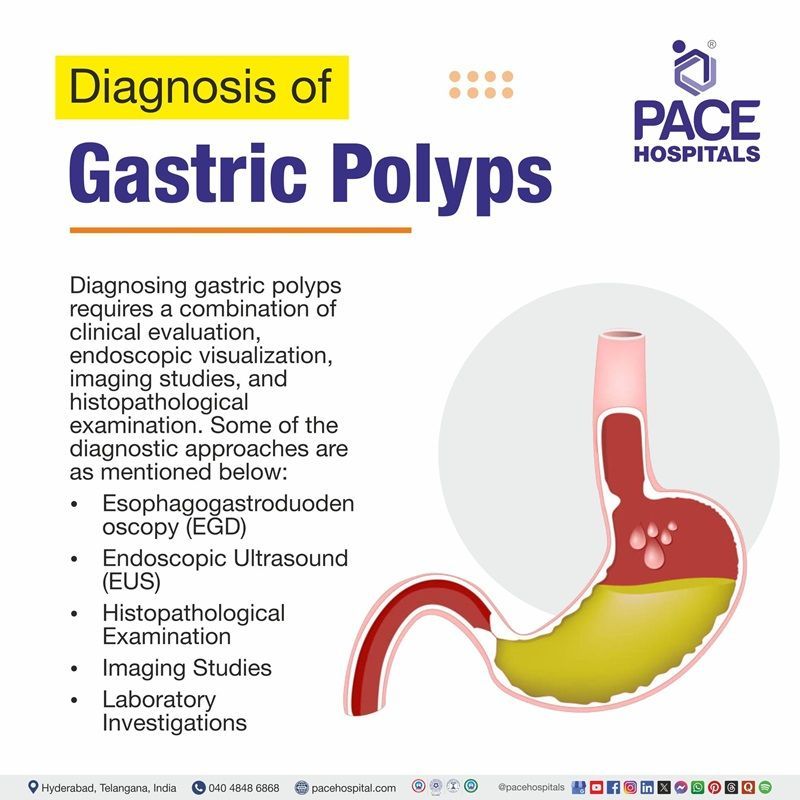
Gastric Polyps Diagnosis
Since most gastric polyps are asymptomatic or incidentally discovered, the evaluation begins with first signs of examination like dyspepsia or anaemia, observed on a regular complete blood count.
Diagnostic Techniques for Gastric Polyps
- Complete Blood Count (CBC): Helps detect anemia, which may indicate chronic blood loss from bleeding polyps.
- Computed Tomography (CT) Scans: Useful for detecting large polyps, assessing their size, and identifying potential malignancy or metastasis.
- Magnetic Resonance Imaging (MRI): Provides detailed imaging for evaluating soft tissue characteristics and differentiating benign lesions from malignant ones.
- Esophagogastroduodenoscopy (EGD): The gold standard for direct visualization, biopsy, and histopathological examination of gastric polyps.
Gastric polyp treatment
Endoscopic visualisation of a stomach polyp is not always sufficient to determine its underlying histology, so biopsy and en-bloc resection are necessary to choose a treatment type. Because of the well-established correlation between lesion size and malignant potential, endoscopic mucosal resection (EMR) is recommended for lesions that are larger than 10 mm.
Some of the treatment options available for gastric polyps are as mentioned below:
- Observation & Monitoring – Small, asymptomatic polyps, especially fundic gland polyps (FGPs), may only require regular endoscopic surveillance.
- H. pylori Eradication – Hyperplastic polyps associated with H. pylori infection may regress after antibiotic therapy.
- Proton Pump Inhibitor (PPI) Discontinuation – Fundic gland polyps linked to long-term PPI use may shrink after stopping medication.
- Endoscopic Polypectomy – Symptomatic, large (>10 mm), or adenomatous polyps are removed via endoscopic mucosal resection (EMR) or biopsy.
- Surgical Resection – Rarely required but indicated for large, obstructive, or malignant polyps cannot be removed endoscopically.
- Genetic Screening & Surveillance – In familial syndromes like FAP or Peutz-Jeghers syndrome, regular endoscopic screening is essential.
Prevention of gastric polyp
While gastric polyps may be associated with symptoms such as weakness, fatigue, and dyspepsia, they are mainly detected unintentionally during endoscopic evaluations carried out to rule out other stomach pathologies like peptic ulcer disease, Barrett oesophagus, and delayed gastric emptying, etc.
Some of the preventive measures for gastric polyps are mentioned below:
- H. pylori Eradication – Timely treatment of Helicobacter pylori infection reduces the risk of hyperplastic polyps and gastric cancer.
- Limiting PPI Use – Avoid prolonged, unnecessary proton pump inhibitor (PPI) therapy, which is linked to fundic gland polyps.
- Healthy Diet – A balanced diet rich in fruits, vegetables, and fiber, while avoiding processed foods and nitrosamines, helps maintain gastric health.
- Regular Endoscopic Screening – Individuals with risk factors, such as familial adenomatous polyposis (FAP) or previous gastric polyps, should undergo periodic endoscopic surveillance.
- Avoiding Smoking & Alcohol – Reducing tobacco and alcohol consumption minimizes gastric mucosal damage and polyp formation.
- Managing Chronic Gastritis – Treating underlying chronic inflammation or autoimmune gastritis can lower polyp risk.
- Routine Health Check-ups – Regular medical consultations help in early detection and management of gastric conditions before complications arise.
Frequently Asked Questions (FAQs) on Gastric polyps
How long does stomach polyps take to recover?
It usually takes around two weeks to recover after removing the stomach polyps. If required and prescribed by a physician, the patient should take painkillers to manage the pain right after the procedure.
Can gastric polyps regrow?
According to clinical records and most physicians' opinions, recurrence of gastric polyps in the same old site is not possible after removing them completely. However, the reappearance of polyps in new locations might occur.
Do gastric polyps bleed?
As most polyps are asymptomatic, bleeding is uncommon in patients with gastric polyps. However, if the polyp is too big, chances of being anaemic, bleeding, or gastric outlet obstruction can occur.
How can you reduce the risk of developing stomach polyps?
One strategy to lower your chance of getting stomach polyps is to manage the factors that may cause them. Maintaining a healthy body weight and choosing healthy diet is key to avoid risk of acquiring gastrointestinal issues such as indigestion, reflux etc. Moreover, this will help in minimising the use of proton pump inhibitors.
What is the commonest gastric polyp?
Epithelial polyps are the most prevalent kind of stomach polyps, and they originate from the outermost layer of your stomach lining. Other, less common varieties may begin in the deeper layers of stomach lining and protrude through to the outer layers.
What foods should you avoid with gastric polyps?
Consume liquids or soft foods that aren't too hot, such as oatmeal, lukewarm vegetable soup, and fruit and vegetable juices, as they are gentle on the digestive tract and do not cause constipation. Provide the body with the protein and minerals to heal quickly. Complex meals that are challenging to swallow and chew should be avoided. Acidic foods like fermented and sour foods like fish sauces and pickles can lead to stomach ulcers that can worsen the wound from surgery.
Can stomach polyps cause acid reflux?
Most of the gastric polyps are asymptomatic. However, when the polyps show any symptoms, it includes indigestion, acid reflux etc.
What are gastric polyps?
Gastric polyps are abnormal tissue growths that protrude from the stomach’s mucosal or submucosal layers. They are usually detected incidentally during an endoscopy and can be benign, precancerous, or malignant. The most common types include fundic gland polyps (FGPs), hyperplastic polyps (HPs), and adenomatous polyps.
What causes gastric polyps?
Gastric polyps develop due to various factors, including chronic gastric inflammation, H. pylori infection, prolonged proton pump inhibitor (PPI) use, genetic syndromes like familial adenomatous polyposis (FAP), and dietary influences. Some polyps arise as a response to tissue irritation, while others result from genetic mutations.
Are gastric polyps cancerous?
Most gastric polyps are benign, but some, especially adenomatous polyps, have the potential to become cancerous. Hyperplastic polyps can also undergo malignant transformation, particularly when associated with chronic H. pylori infection or atrophic gastritis. Regular monitoring is essential for identifying high-risk polyps.
What are the symptoms of gastric polyps?
Most gastric polyps are asymptomatic, but larger or ulcerated ones may cause symptoms like dyspepsia, heartburn, gastrointestinal bleeding, anemia, obstruction, nausea, or vomiting. In rare cases, they can grow large enough to block food passage, leading to gastric outlet obstruction.
How are gastric polyps diagnosed?
Diagnosis involves esophagogastroduodenoscopy (EGD) for direct visualization and biopsy, along with complete blood count (CBC) to check for anemia. Imaging techniques like CT scans or MRI may be used for larger polyps to assess their extent, structure, and potential malignancy.
Can gastric polyps be prevented?
Prevention includes treating H. pylori infection, minimizing long-term PPI use, maintaining a healthy diet, avoiding smoking and alcohol, and managing chronic gastritis. People with genetic syndromes like FAP should undergo regular endoscopic screening to monitor polyp formation and progression.
Do all gastric polyps require removal?
Not all gastric polyps require removal. Small, benign fundic gland polyps (FGPs) and some hyperplastic polyps may only need regular monitoring. However, adenomatous polyps, large polyps (>10 mm), and symptomatic polyps should be removed due to their malignant potential.
What is the best treatment for gastric polyps?
Treatment depends on the type, size, and symptoms of the polyps. Small, asymptomatic polyps are often monitored, while endoscopic polypectomy is used for larger or precancerous polyps. In rare cases, surgical resection is required for extensive or malignant polyps.
Can gastric polyps grow back after removal?
Yes, some types of gastric polyps, especially hyperplastic and adenomatous polyps, may recur after removal, particularly if the underlying cause (e.g., chronic gastritis or H. pylori infection) is not treated. Regular follow-up endoscopy is recommended to monitor recurrence.
Is there a connection between gastric polyps and acid reflux?
Gastric polyps themselves do not cause acid reflux, but chronic acid suppression with PPIs can lead to the development of fundic gland polyps. Additionally, acid reflux can cause gastritis, which may contribute to the formation of hyperplastic polyps over time.
Can a diet influence the risk of gastric polyps?
Yes, a diet high in processed foods, nitrites, and excessive salt can increase the risk of gastric mucosal irritation and polyp formation. A diet rich in fruits, vegetables, fiber, and antioxidants helps maintain gastric health and may reduce polyp risk.
Are gastric polyps common?
Gastric polyps are relatively common and are detected in about 1-6% of endoscopies. Most are benign and asymptomatic, with fundic gland polyps (FGPs) and hyperplastic polyps being the most frequently encountered types. Their prevalence increases with age.
How often should gastric polyps be monitored?
The frequency of monitoring depends on the type of polyp. Small, benign polyps may require surveillance every 1-3 years, while adenomatous or high-risk polyps need more frequent follow-ups. Patients with FAP or Peutz-Jeghers syndrome require closer monitoring.
What happens if gastric polyps are left untreated?
Many gastric polyps remain harmless, but untreated high-risk polyps (e.g., adenomatous polyps) may progress to gastric cancer. Large polyps can cause bleeding, anemia, gastric obstruction, or perforation, leading to serious complications requiring urgent medical intervention.
Can gastric polyps cause weight loss?
While most gastric polyps do not cause weight loss, large polyps that obstruct food passage can lead to reduced appetite, early satiety, nausea, and vomiting, resulting in unintentional weight loss. If weight loss is accompanied by other symptoms, medical evaluation is necessary.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868