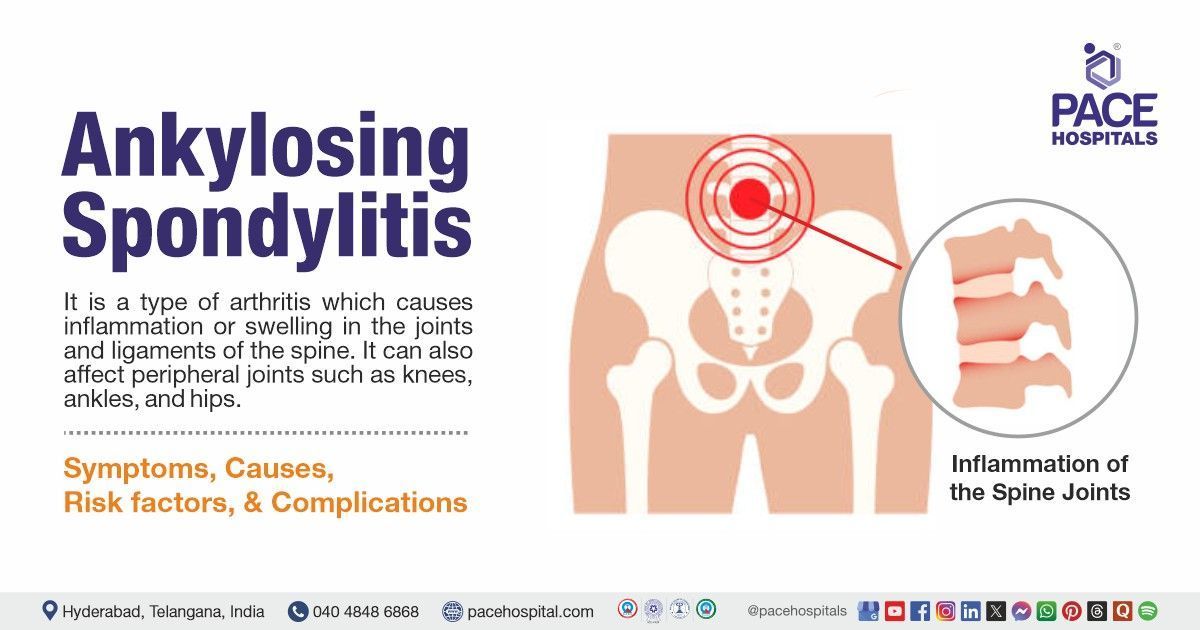
Ankylosing Spondylitis - Symptoms, Causes, Complications, Diagnosis & Treatment
Ankylosing spondylitis definition
It is a type of arthritis which causes inflammation or swelling in the joints and ligaments of the spine. It can also affect peripheral joints such as knees, ankles, and hips. There is no known cause of ankylosing spondylitis (AS), but it is thought to be linked to a particular gene variant known as HLA-B27. Symptoms include back pain, a straight and stiff spine, extreme tiredness, loss of appetite, and weight loss. A rheumatologist can treat ankylosing spondylitis.
Ankylosing spondylitis meaning
The term ankylosing spondylitis is a combination of two words: "ankylosis" and "spondylitis"
The term “ankylosis” means stiffening of joints, which is caused by the fusion of two or more bones into one.
The term “spondylitis” is derived from the Latin language “spondylo” which means “of the vertebrae”, and “itis” meaning "inflammation". Together, it means inflammation of the vertebrae.
Ankylosing Spondylitis Prevalence
Prevalence of ankylosing spondylitis worldwide
The prevalence of ankylosing spondylitis is thought to vary across different regions. The mean prevalence of ankylosing spondylitis per 10,000 (from 36 eligible studies) was 23.8 in Europe, 16.7 in Asia, 31.9 in North America, 10.2 in Latin America, and 7.4 in Africa.
Prevalence of ankylosing spondylitis in India
According to epidemiological studies, the prevalence of ankylosing spondylitis (AS) in India is estimated to be between 7 to 9 cases per 10,000 people. Males are more likely to have AS than females (male-to-female ratios can reach 16:1), and the condition usually manifests in the early 20s and 30s. Although this prevalence may differ by region due to genetic and environmental factors, it is consistent with global estimates that range from 0.1% to 1.4%.
Ankylosing Spondylitis Causes
There is no known cause of ankylosing spondylitis, but a few studies show that both genes and the environment may lead to the development of the disease. The HLA-B27 gene can increase the risk of developing ankylosing spondylitis, but that does not mean that everyone with this gene will develop the disease.
Ankylosing Spondylitis Symptoms
The symptoms of ankylosing spondylitis may come and go over time. These symptoms may be different in different among individuals. The following are some of the ankylosing spondylitis signs and symptoms:
- Back pain, which is usually severe at night, especially during rest
- Early morning stiffness
- Straight and stiff spine
- Inability to take a deep breath, if the joints between the ribs and spine are affected
- Loss of appetite
- Weight loss
- Tiredness or fatigue
- Fever
- Anemia
- Joint pain
- Inflammation of the eye
- Organ damage, such as to the heart, lungs, and eyes
- Rashes on the skin
- Digestive illness
Ankylosing Spondylitis Risk Factors
Ankylosing spondylitis is chronic arthritis which causes inflammation, pain, and stiffness mostly in the spine and the sacroiliac joints, which are located just above the tailbone. There are several factors which can increase the risk of developing ankylosing spondylitis. The following are some of the risk factors of ankylosing spondylitis:
- Age: Ankylosing spondylitis occurs more commonly in young adults. Though degenerative arthritis is associated with aging, inflammatory back pain usually occurs at a younger age. Almost 80 percent of patients will experience early symptoms before the age of 30, and merely about 5 percent of ankylosing spondylitis patients will experience the symptoms at the age of 45 or older.
- Gender: Because of the overwhelming diagnosis of ankylosing spondylitis in men compared to women, it used to be considered a man’s disease. Men are more likely to get radiographic damage (damage to the spinal joints, which is visible on X-rays). Non-radiographic axial spondylarthritis, having the same symptoms as ankylosing spondylitis but without causing radiographic damage, is more commonly seen in women. Ankylosing spondylitis may be misdiagnosed in women, and women tend to be diagnosed later compared to men, and they experience more misdiagnoses.
- Genes: Certain types of genes play a key role in the developing ankylosing spondylitis; one of the genes is the HLA-B gene, which is part of a gene family called the human leukocyte (HLA) complex. This gene has hundreds of variations, each one of them differentiated by a number. One of these gene variations, HLA-B27, has a strong connection to the development of ankylosing spondylitis. But it is important to note that ankylosing spondylitis can develop without being positive for HLA-B27 and also being positive for HLA–B27 does not guarantee that one may develop ankylosing spondylitis.
- Environmental causes: Environmental factors can increase the risk of developing ankylosing spondylitis, but they are not clearly understood. Factors such as exposure to certain infections, toxins, and pollutants; injury to affected joints; changes in the colon bacteria; and bowel inflammation increase the risk of ankylosing spondylitis, but how these factors influence the onset and severity of ankylosing spondylitis is not understood.
- Race: Caucasians are affected more by ankylosing spondylitis compared to African Americans, which may be due to the prevalence of the HLA-B27 gene. This gene is present in 90 to 95 percent of Caucasian patients with ankylosing spondylitis. The prevalence of this gene is low in African Americans with ankylosing spondylitis.
- Family history: Ankylosing spondylitis runs in families; that is, if a parent or sibling is diagnosed with ankylosing spondylitis, it is estimated that the patient is 10 to 20 times more likely to have ankylosing spondylitis than someone with no family history of the disease.
- Inflammatory bowel disease (IBD): Having one disease can increase the risk of developing the other. Inflammation or swelling of the gastrointestinal tract is common in ankylosing spondylitis. Many recent studies have indicated that about 3 percent to 4 percent of patients with ankylosing spondylitis have inflammatory bowel disease.
- Uveitis: It is a type of inflammation of the eye, and with one episode of uveitis, there is a greater risk of developing ankylosing spondylitis. According to a study of Arthritis Research and Therapy, uveitis occurs in about a quarter of patients with ankylosing spondylitis and is the most common manifestation of the disease outside the joints.
Ankylosing Spondylitis Complications
Ankylosing spondylitis is a complex disease which can affect different parts of the body. It can cause some serious complications, affecting day-to-day life and leading to additional health problems. Ankylosing spondylitis patients are at greater risk of thinning of the bones (osteoporosis), which can result in spinal fractures. The following are some of the complications of ankylosing spondylitis:
- Joint damage: In patients with ankylosing spondylitis, the hips and knees get inflamed, which over time can damage the affected joints, making them painful and difficult to move. Surgery may be required if the joint is damaged to replace the damaged joint with an artificial one.
- Iritis: It is also known as acute anterior uveitis, a condition commonly associated with ankylosing spondylitis. In this condition, the front part of the eye becomes red and swollen, which usually affects only one eye, rather than both.
- Osteoporosis: It is a condition where the bones become weak and brittle, and it is a common and frequent complication of ankylosing spondylitis. In patients with ankylosing spondylitis, the inflammation of joints is associated with trabecular bone loss, which leads to osteoporosis.
- Spinal fractures: In this condition, the progressive fusion of vertebrae causes the spine to stiffen, and as a result, the bones become prone to breaking even under minor traumas. Due to a weak spine, there is always a risk of spinal fractures.
- Cardiovascular disease: Ankylosing spondylitis increases the risk of developing cardiovascular diseases, and this risk is multifactorial, including inflammation accelerating atherosclerosis and cardiac inflammation itself, such as in aortitis.
- Cauda equina syndrome: This is a rare complication of ankylosing spondylitis, which occurs when the nerves at the bottom of the spine become compressed (compacted). Severe weaknesses or numbness in both legs and numbness around the genitals are some of the symptoms of cauda equina syndrome.
- Psoriasis: It is a commonly seen complication in patients with ankylosing spondylitis and is triggered by a skin break injury from vaccinations, sunburns, scratches, or other skin breaks.
- Inflammatory bowel disease (IBD): In patients with ankylosing spondylitis, there is always a risk of developing inflammatory bowel disease. This risk is because of the similar underlying mechanisms, which include an overactive immune system attacking healthy tissues in both the joints and the digestive tract.
Ankylosing Spondylitis Diagnosis
For diagnosing ankylosing spondylitis, a comprehensive evaluation of the entire body is suggested because of the disease systemic nature and its potential involvement with multiple organ systems. The following are the steps involved in diagnosing ankylosing spondylitis:
- Initial evaluation
- Medical history
- Physical examination
- Diagnostic evaluation
- Laboratory testing
- Complete blood count (CBC)
- C–reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Human leukocyte antigen B27 (HLA)
- Imaging studies
- X-rays
- Magnetic resonance imaging (MRI)
- Ultrasound
- Genetic testing
Ankylosing Spondylitis Treatment
There is no cure for ankylosing spondylitis, and the treatment usually involves managing the symptoms and preventing further disease progression. The following are the steps involved in the treatment of ankylosing spondylitis:
- Physiotherapy and exercise
- Drug therapy
- Painkillers or Nonsteroidal Anti-Inflammatory Drugs (NSAIDS)
- Biologic therapy
- Tumor necrosis factor (TNF) inhibitors
- Monoclonal antibody treatment
- Janus kinase Inhibitors (JAK inhibitors)
- Disease modifying antirheumatic drugs (DMARDs)
- Corticosteroids
- Bisphosphonates
- Surgery
Ankylosing Spondylitis Prevention
There is no proven way of preventing ankylosing spondylitis. However, prevention of disease morbidity can be achieved with exercise, physical therapy, and tailored pharmacologic intervention.
Difference Between Dish and Ankylosing Spondylitis
Dish v/s ankylosing spondylitis
Both dishes (Diffuse Idiopathic Skeletal Hyperostosis) and ankylosing spondylitis (AS) are types of arthritis which affect the spine but differ significantly in their characteristics and causes. Dish is usually characterized by bone spurs and hardening of ligaments, while ankylosing spondylitis is an inflammatory condition that affects the sacroiliac joints and spine.
| Parameter | Dish (Diffuse Idiopathic Skeletal Hyperostosis) | Ankylosing spondylitis |
|---|---|---|
| Definition | It is a systemic condition which is characterized by distinct ossification patterns affecting the spine and peripheral entheses. | It is a type of arthritis which causes inflammation or swelling in the joints and ligaments of the spine. It can also affect peripheral joints such as knees, ankles, and hips. |
| Causes | The cause remains is not clearly understood, but several risk factors have been identified, such as gout, hyperlipidemia, and diabetes, linked with development of dish. | There is no known cause of ankylosing spondylitis, but few studies show that both genes and environment may lead to the development of the disease. HLA-B27 gene can increase the risk of developing ankylosing spondylitis |
| Symptoms | Pain in the back, neck, shoulders, elbows, knees, or heels; tingling, numbness, or weakness in the legs are some of the symptoms of dish. | Back pain, early morning stiffness, straight and stiff spine, loss of appetite, weight loss, tiredness or fatigue, fever, anemia and joint pain. |
| Treatment | The primary treatment for dish includes activity modification, physical therapy, bracing, nonsteroidal anti-inflammatory drugs (NSAIDs), and bisphosphonates. Surgical decompression and stabilization may be indicated in cases of fractures, cervical myelopathy, lumbar stenosis, neurologic deficits, and infections. | There is no cure for ankylosing spondylitis, and the treatment usually involves managing the symptoms and preventing further disease progression. Treatment usually involves pain killers, corticosteroids, biologic agents, and disease-modifying antirheumatic drugs. |
Difference Between Ankylosing Spondylitis and Rheumatoid Arthritis
Ankylosing spondylitis v/s Rheumatoid arthritis
Both Rheumatoid arthritis (RA) and ankylosing spondylitis (AS) are the most common rheumatic diseases. These chronic progressive inflammatory diseases can lead to a reduction in physical fitness and an increase in joint degeneration. Though they are closely related, their symptomatology and etiology are different. The following are some of the key parameters that differentiate between rheumatoid arthritis and ankylosing spondylitis:
| Parameters | Rheumatoid arthritis | Ankylosing spondylitis |
|---|---|---|
| Definition | It is a condition which causes inflammation of the joint and joint pain. It usually occurs when the immune system doesn’t function properly and attacks the lining of the joints, called the synovium. | It is a type of arthritis which causes inflammation or swelling in the joints and ligaments of the spine. It can also affect peripheral joints such as knees, ankles, and hips. |
| Causes | The cause of rheumatoid arthritis is thought to occur from the interaction between patients' genotypes and environmental factors. | There is no known cause of ankylosing spondylitis, but few studies show that both genes and the environment may lead to the development of the disease. The HLA-B27 gene can increase the risk of developing ankylosing spondylitis |
| Symptoms | Pain, stiffness, tenderness and swelling or redness in one or more joints are some of the symptoms of rheumatoid arthritis. | Back pain, early morning stiffness, straight and stiff spine, loss of appetite, weight loss, tiredness or fatigue, fever, anemia, and joint pain. |
| Treatment | It is not curable; treatment usually helps in improving and maintaining joint mobility and muscle strength. Treatment usually involves non-steroidal anti-inflammatory drugs (NSAIDs), glucocorticoids, disease-modifying antirheumatic drugs (DMARDs), and biological agents. | There is no cure for ankylosing spondylitis, and the treatment usually involves managing the symptoms and preventing further disease progression. Treatment usually involves pain killers, corticosteroids, biologic agents, and disease-modifying antirheumatic drugs. |
Frequently Asked Questions (FAQs) on Ankylosing Spondylitis (AS)
Can ankylosing spondylitis be cured?
There is no cure for ankylosing spondylitis, and the treatment usually involves symptom management. The primary aim of ankylosing spondylitis treatment is to reduce pain and stiffness, preserve axial spine mobility and functional ability, and prevent spinal complications.
How is ankylosing spondylitis diagnosed?
Diagnosis of ankylosing spondylitis involves findings from medical history and physical examination. Laboratory tests such as complete blood count (CBC), erythrocyte sedimentation rate (ESR), C reactive protein help in detecting signs of inflammation, and imaging studies such as X-rays, magnetic resonance imaging (MRI), and ultrasound help in confirming the diagnosis.
What are the treatment options available for ankylosing spondylitis?
Ankylosing spondylitis treatment aims to reduce pain and stiffness, preserve spine mobility and functional ability, and prevent spinal complications. In most cases, treatment usually includes physical exercise and drug therapy, and in severe cases, surgery may be advised. Drug therapy usually includes the use of analgesics; biological treatments such as anti-tumor necrosis factor medicines, monoclonal antibodies, and steroids. Surgical treatment includes joint replacement and hip replacement surgery.
When is surgery required for treating ankylosing spondylitis?
When ankylosing spondylitis results in severe joint damage and the patient is unable to perform daily activities, surgery such as hip replacement surgery and total knee replacement surgery is recommended.
Which blood test shows ankylosing spondylitis?
Several blood tests, such as complete blood count (CBC), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and human leukocyte antigen B27 (HLA-B27), help in diagnosing ankylosing spondylitis, but these tests alone cannot detect ankylosing spondylitis. These blood tests are generally ordered to look for signs of inflammation.
How does MRI help in diagnosing ankylosing spondylitis?
Magnetic resonance imaging techniques are required to detect more subtle abnormalities, such as fatty or inflammatory changes. This imaging technique can reveal active inflammatory lesions in the sacroiliac joints, and these lesions appear as bone marrow edema (BME) on short tau inversion recovery (STIR) and T2-weighted images with fat suppression. It is important to note that the presence of BME on magnetic resonance imaging can be seen in up to 23 percent of the patients with mechanical back pain and 7 percent of healthy individuals.
Can ESR be elevated in chronic ankylosing spondylitis?
Yes, the levels of erythrocyte sedimentation are elevated in patients with ankylosing spondylitis. About 50 to 70 percent of patients with ankylosing spondylitis show elevated levels of erythrocyte sedimentation rate (ESR) and elevated C-reactive protein (CRP). A normal ESR and CRP do not exclude the possibility of ankylosing spondylitis.
What is long term treatment for ankylosing spondylitis?
Non-steroidal anti-inflammatory drugs (NSAIDS), which are considered as the first-line drug therapy, are prescribed for long-term use. When these non-steroidal anti-inflammatory drugs do not provide adequate relief these drugs are used in combination with tumor necrosis factor inhibitors (TNF – Is). Response to treatment with NSAIDS is assessed after 4 to 6 weeks of initiation, and the response of tumor necrosis factor inhibitors is evaluated after 12 weeks.
Does positive HLA B27 indicate that the individual has ankylosing spondylitis?
Human leukocyte antigen (HLA B27) is a part of a family of genes called the human leukocyte (HLA) complex, which helps the immune system to differentiate between the body’s own proteins and those produced by invaders such as bacteria or viruses. This gene increases the likelihood of developing ankylosing spondylitis, but being positive for HLA B27 does not guarantee that one will develop ankylosing spondylitis.
Can the HLA B27 test be negative in ankylosing spondylitis?
Yes, the HLA B27 test can sometimes be negative in patients with ankylosing spondylitis. It is important to note that ankylosing spondylitis can develop without being positive for HLA-B27. African American patients with ankylosing spondylitis are less likely to have HLA-B27 than Caucasians, but they can still develop the disease.
What is the role of physiotherapy in treating ankylosing spondylitis?
Physiotherapy plays a key role in treating ankylosing spondylitis. By being physically active, the patient can improve posture and range of spinal movement, along with preventing the spine from becoming stiff and painful.
What is the prognosis of ankylosing spondylitis patients?
The prognosis of ankylosing spondylitis differs in every patient. Patients with an earlier onset of ankylosing spondylitis (AS) are associated with poorer functional outcomes. But it is important to note that severe physical disability is uncommon in ankylosing spondylitis. In patients with severe and long-standing disease, there is an increased risk of mortality primarily attributed to increased cardiovascular complications.
What is the difference between ankylosing spondylitis and arthritis?
Arthritis is a broad term which refers to inflammation, pain, stiffness, swelling, and reduced range of motion in one or more joints. It includes over 100 different conditions, including osteoarthritis, rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. Ankylosing spondylitis, on the other hand, is a type of arthritis that affects the spine and sacroiliac joints, causing chronic inflammation.
What is the difference between ankylosing spondylitis and spondylosis?
Spondylosis refers to age-related degenerative changes in the spine, such as wear and tear of the spinal discs, cartilage, and vertebrae. It can lead to bone spurs, which can compress nerves or the spinal cord, resulting in symptoms such as numbness, weakness, or tingling. Ankylosing spondylitis, on the other hand, is a type of arthritis which affects the spine and sacroiliac joints, causing inflammation.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868