Colon Polyps: Types, Causes, Symptoms, Risk factors, Diagnosis, Treatment & Prevention
Colon polyps are abnormal tissue growths that develop on the inner lining of the colon. They vary in size, shape, and potential for malignancy, with some remaining benign while others can progress to colorectal cancer. Most polyps are asymptomatic and are detected incidentally during routine colonoscopy. Risk factors include age, genetic predisposition, diet, and lifestyle habits.
Definition of colon polyp
Colon polyps are abnormal growths on the colon's inner lining, classified as benign, pre-malignant, or malignant. While most are harmless, some may develop into colorectal cancer if left untreated. Polyps are commonly detected during routine screening colonoscopies and can be removed to prevent malignancy.
Colon Polyps Meaning
- The term "colon polyp" has origins in Greek and Latin:
- "Colon" comes from the Latin colon, which itself is derived from the Greek "kolon", meaning "large intestine" or "part of the body." In ancient Greek medicine, kolon referred specifically to the segment of the digestive tract responsible for water absorption and waste processing.
- "Polyp" is derived from the Greek word polys meaning "many" and pous meaning "foot." In ancient times, the term polypous was used to describe organisms like octopuses due to their many appendages. Later, in medical terminology, it came to describe abnormal growths in the body that often have multiple projections or a stalk-like appearance.
- Thus, "colon polyp" etymologically means "a growth with multiple projections in the large intestine."
Colon polyps prevalence
Prevalence Worldwide
Colon polyps are a common condition worldwide, with prevalence rates varying based on age, diet, genetic factors, and screening practices. Studies suggest that approximately 15–40% of adults over the age of 50 develop colon polyps. The risk increases with age, with a higher incidence in Western countries due to dietary and lifestyle factors.
The increasing consumption of processed foods, obesity, and sedentary lifestyles are significant contributors to the prevalence of colon polyps in developed nations.
Prevalence in India
- In India, colon polyps are less common than in Western populations, mostly because of variations in dietary patterns, fiber consumption, and genetic susceptibility. However, the necessity of routine colorectal screening is becoming more widely acknowledged due to factors such as rising colorectal cancer rates, dietary changes, and urbanization.
- Recent hospital-based studies estimate the prevalence of colon polyps in India to be around 7–10% in adults undergoing colonoscopy. The incidence of adenomatous polyps, which have the potential to progress into malignancy, is increasing in urban areas due to shifts toward Western dietary patterns.

Types of Colon Polyps
Colon polyps are classified based on their histological characteristics and potential for malignancy:
Adenomatous Polyps of colon (Adenomas)
- These are the most common type, accounting for approximately 70% of all polyps.
- They are pre-malignant, meaning they have the potential to progress to colorectal cancer.
- The subtypes include tubular adenomas (which are the most common), villous adenomas (which have a higher risk of malignancy), and tubulovillous adenomas (which have characteristics of both).
Hyperplastic colon Polyps
- These are generally small and benign growths.
- They have a low risk of malignancy but may be associated with serrated polyposis syndrome, which increases the risk of colorectal cancer.
Serrated Polyps
- This category includes sessile serrated adenomas (SSA) and traditional serrated adenomas (TSA).
- These polyps have a higher malignant potential than hyperplastic polyps and require careful surveillance.
Inflammatory Polyps
- These polyps are commonly seen in patients with inflammatory bowel disease (IBD).
- They are typically non-neoplastic, arising due to chronic inflammation rather than uncontrolled cell growth.
Hamartomatous Polyps
- These polyps are seen in genetic syndromes such as Peutz-Jeghers syndrome and juvenile polyposis.
- The risk of malignancy varies depending on the underlying syndrome.
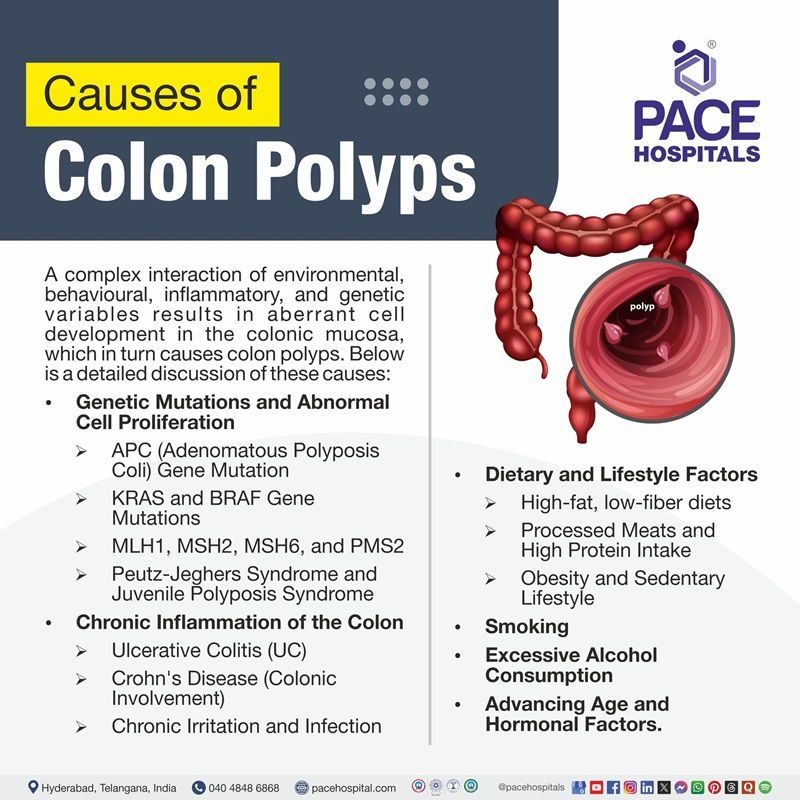
Colon Polyps Causes
A complex interaction of environmental, behavioural, inflammatory, and genetic factors results in aberrant cell growth in the colonic mucosa, which in turn causes colon polyps. Although the exact cause is unknown, a number of important factors play a role in their formation. Below is a detailed discussion of these causes:
Genetic Mutations and Abnormal Cell Proliferation
Colon polyps, especially adenomatous polyps, which can evolve into colorectal cancer, are largely caused by genetic changes. Uncontrolled cell division, abnormal growth patterns, and the breakdown of regulatory systems that prevent excessive tissue proliferation are all consequences of these mutations.
Key Genetic Factors
APC (Adenomatous Polyposis Coli) Gene Mutation
- The Adenomatous Polyposis coli (APC) gene works as a tumor suppressor, regulating cell growth.
- Mutations in the APC gene lead to dysregulated cell division, increasing the likelihood of adenoma formation.
- Found in patients with Familial Adenomatous Polyposis, a condition characterized by hundreds to thousands of polyps, eventually leading to colorectal cancer if untreated.
KRAS and BRAF Gene Mutations
- These oncogenes, when mutated, drive uncontrolled cell proliferation and increase polyp formation.
- They are frequently associated with serrated polyps, which have a higher risk of malignant transformation.
MLH1, MSH2, MSH6, and PMS2
- Mutations in these genes lead to Lynch Syndrome (Hereditary Non-Polyposis Colorectal Cancer.
- Individuals with Lynch Syndrome have a greater risk of developing colorectal cancer with fewer polyps compared to FAP.
Peutz-Jeghers Syndrome and Juvenile Polyposis Syndrome
- Both syndromes involve mutations in genes controlling cell growth and differentiation.
- They are associated with hamartomatous polyps and an increased lifetime risk of colorectal cancer.
- Genetic testing is essential for people with a strong family history of colorectal cancer since genetic factors contribute to both hereditary polyposis syndromes and random polyps.
Chronic Inflammation of the Colon
Inflammatory conditions affecting the colon can lead to polyp formation due to continuous epithelial damage, repair, and abnormal tissue remodeling.
Ulcerative Colitis (UC)
- A chronic inflammatory disease that affects the mucosal lining of the colon.
- Leads to inflammatory (pseudopolyps), which are benign but indicate chronic mucosal damage.
- Long-standing UC increases the risk of dysplastic changes and colorectal cancer.
Crohn's Disease (Colonic Involvement):
- Chronic inflammation in Crohn's disease leads to irregular mucosal repair and potential polyp formation.
- It increases the risk of dysplasia and malignant transformation in long-standing cases.
Chronic Irritation and Infection:
- Recurrent bacterial infections, colonic ulcers, and diverticulitis may contribute to mucosal damage and polyp development.
- Regular colonoscopic surveillance is essential for individuals with inflammatory bowel disease (IBD) to detect pre-cancerous changes early.
Dietary and Lifestyle Factors
Diet and lifestyle choices play crucial role in the formation of colon polyps by affecting intestinal health, inflammation, and oxidative stress levels.
High-fat, low-fiber diets:
- Diets rich in saturated fats, red meat, and processed foods promote chronic inflammation and increase colorectal cancer risk.
- Low fiber intake leads to slower bowel movements, prolonging exposure to carcinogens and increasing polyp risk.
- Fiber promotes gut motility, dilutes potential carcinogens, and supports the growth of beneficial gut bacteria.
Processed Meats and High Protein Intake:
- Nitrates and preservatives in processed meats can generate carcinogenic compounds.
- Cooking meat at high temperatures (e.g., grilling, frying) can produce heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs), which contribute to DNA damage.
Obesity and Sedentary Lifestyle:
- Obesity is associated with increased insulin resistance, chronic inflammation, and changes in gut microbiota, all of which contribute to polyp formation.
- Physical inactivity results in slower gut motility and prolonged exposure of colonic cells to harmful substances.
Smoking and Excessive Alcohol Consumption
Both smoking and excessive alcohol intake significantly increase the risk of polyp formation and colorectal cancer.
Smoking
- Tobacco contains multiple carcinogens that damage colonic DNA and promote polyp formation.
- Long-term smokers have a higher prevalence of adenomatous and serrated polyps with increased malignant potential.
- Smoking leads to chronic inflammation and oxidative stress, further accelerating the risk of dysplasia.
Excessive Alcohol Consumption
- Alcohol metabolism creates acetaldehyde, a toxic compound that damages DNA and increases cancer risk.
- Chronic alcohol use increases inflammatory cytokines and oxidative stress, promoting abnormal tissue growth.
- Excessive alcohol intake is associated with larger and more aggressive polyps.
- Reducing or eliminating smoking and alcohol consumption is a critical step in reducing colorectal polyp risk.
Advancing Age and Hormonal Factors
- The risk of colon polyps increases with age, particularly after the age of 50.
- Age-related genetic mutations accumulate over time, leading to abnormal cell growth and polyp formation.
- Age-related immune system decline reduces the body's ability to detect and eliminate abnormal cells.
- Hormonal changes, particularly in postmenopausal women, may also influence polyp formation.
- Longer exposure to dietary carcinogens and environmental toxins increases the cumulative risk of polyp development.
- Regular colorectal cancer screening (e.g., colonoscopy every 5–10 years after the age of 50) is crucial for early detection and prevention.
Colon Polyps Symptoms
Colon polyps are often asymptomatic, making them difficult to detect without routine screening. In many cases, individuals with polyps remain unaware of their presence until a colonoscopy or other diagnostic test identifies them. However, when polyps grow larger or become ulcerated, they can produce noticeable symptoms. Below is a detailed discussion of the key symptoms associated with colon polyps.
Rectal Bleeding or Visible Blood in the Stool
- One of the most common and alarming symptoms of colon polyps is rectal bleeding. Blood may appear as bright red streaks on the surface of the stool, which typically indicates bleeding from the lower colon or rectum.
- In some cases, the blood may be dark and tarry (melena), which suggests bleeding from a higher location in the gastrointestinal tract. Since some polyps bleed intermittently, the detection of blood in the stool may be inconsistent. Chronic blood loss from polyp-related bleeding can lead to iron deficiency anemia over time
- It is important to note that rectal bleeding can also be caused by other conditions such as haemorrhoids, anal fissures, diverticulosis, or colorectal cancer, making proper diagnostic testing like colonoscopy essential.
Changes in Bowel Habits
- Colon polyps can cause persistent alterations in stool frequency, consistency, or shape, which may indicate their presence.
- If the polyps produce excessive mucous secretions, they may lead to persistent diarrhea. This symptom is more common in polyps located in the proximal (right-sided) colon, where excessive fluid is secreted into the stool.
- If the polyp causes partial obstruction, the patient may experience chronic constipation and difficulty passing stool. This is more common when the polyp is in the distal colon or rectum.
- Some individuals with colon polyps experience alternating episodes of diarrhea and constipation, which may indicate the presence of multiple polyps with varying effects on bowel motility.
- If bowel habit changes persist for more than a few weeks, it is important to seek medical evaluation to rule out serious conditions such as colorectal cancer.
Abdominal Pain or Cramping
- While most tiny polyps are painless, bigger polyps can cause intestinal blockage, which can be uncomfortable.
- Patients may experience cramping or colicky abdominal pain, particularly after meals, as the polyp interferes with normal intestinal function.
- The presence of a large polyp may cause bloating and discomfort, as stool passage becomes restricted.
- In severe cases, where a polyp causes complete obstruction, symptoms may include severe pain, nausea, and vomiting, requiring emergency medical attention.
- Lower abdominal pain is more likely to be caused by polyps in the rectum or sigmoid colon.
- A polyp that has necrosis or torsion may cause abrupt, excruciating pain that calls for immediate medical attention.
Mucous Discharge from the Rectum
- Some types of polyps, particularly inflammatory polyps and villous adenomas, produce excess mucous, which can lead to additional symptoms.
- Patients may notice watery or slimy stools with noticeable mucous.
- In some cases, individuals may experience rectal discharge of mucous, especially in the morning or after defecation.
- Excess mucus can irritate the area around the anus, resulting in discomfort or itching.
- Excessive mucus release in extreme situations can change the electrolyte balance, resulting in muscle weakness and dehydration.
Iron Deficiency Anemia Due to Chronic Blood Loss
- Many polyps bleed gradually over time, which causes iron levels to gradually be depleted without any visible bleeding.
- Chronic blood loss from polyps can result in significant iron deficiency anemia, which may be the first sign of an undetected polyp.
- Anaemia’s symptoms include weakness, brittle nails, pale skin, and exhaustion because the blood's ability to carry oxygen is diminished.
- Some individuals may experience shortness of breath, dizziness, or light-headedness, especially with physical exertion.
- A complete blood count (CBC) test frequently shows low ferritin and hemoglobin levels, which leads to a colonoscopy for more testing.
- Early detection of the cause of chronic blood loss is essential since chronic anemia can affect general health and wellbeing.
Other Possible Symptoms of Colon Polyps
- In some cases, colon polyps may be associated with additional symptoms, though they are less common.
- Unexplained weight loss may occur if polyps interfere with nutrient absorption, and in some cases, it can be a warning sign of early malignancy.
- Excessive gas or bloating may be present if a polyp alters normal colonic motility, leading to increased gas production.
- A feeling of incomplete evacuation, also known as tenesmus, may occur if a large rectal polyp obstructs stool passage, causing the sensation of needing to defecate even after a bowel movement.
Colon polyps risk factors
- Age greater than 50 years, as the incidence of polyps increases with aging.
- The risk of colon polyp formation is increased by a family history of colon polyps or colorectal cancer.
- Recurrence risk is increased by a personal history of polyps or inflammatory bowel disease.
- Obesity and a sedentary lifestyle, both of which contribute to metabolic and inflammatory changes.
- A high-fat, low-fiber diet, particularly one rich in processed meats and red meat.
- Smoking and heavy alcohol use, both of which are known carcinogenic factors.
- An elevated risk of colorectal cancer is linked to type 2 diabetes.
Complications of Colon Polyps
Some of the complications associated with colon polyps are as mentioned below:
- Malignant Transformation: Some polyps can progress to colorectal cancer over time if left untreated.
- Intestinal Obstruction: Large polyps may cause partial or complete blockage of the intestinal track.
- Bleeding and Anemia: Iron deficiency anemia brought on by persistent blood loss from polyps can cause weakness and exhaustion.
- Recurrence: Polyps can recur even after removal, requiring regular follow-up screenings to prevent malignant progression.
Diagnosis of Colon Polyps
Diagnosis of colon polyps is primarily based on imaging and endoscopic evaluation:
- Colon polyp removal or Colonoscopy (Gold Standard): This procedure detects and allows for the removal of polyps during the examination.
- Sigmoidoscopy: Sigmoidoscopy examines the lower part of the colon and is useful for detecting polyps in the rectal and sigmoid regions.
- CT Colonography (Virtual Colonoscopy): A non-invasive imaging test that provides a detailed view of the colon using CT scans.
- Fecal Occult Blood Test (FOBT) & Fecal Immunochemical Test: These are indirect tests to detect hidden blood in the stool, which may indicate the presence of polyps or malignancy.
- Genetic Testing: It is advised for people with polyposis syndromes or a strong family history of colorectal cancer.
Colon Polyps Treatment
The mainstay of treatment is the removal of polyps to prevent complications:
Polypectomy (Endoscopic Removal)
- Performed during a colonoscopy using snares or biopsy forceps to excise the polyp.
- Electrocautery may be used to prevent bleeding from the excised site.
Surgical Resection
- Required for large or cancerous polyps that cannot be safely removed endoscopically.
- Segmental colectomy may be necessary in cases of hereditary polyposis syndromes.
Pharmacological Management
- NSAIDs and aspirin have been studied for their potential role in reducing adenoma recurrence.
- Chemoprevention strategies continue to be explored through ongoing clinical trials.
Prevention of Colon Polyps
- Regular colorectal cancer screening, particularly for individuals over the age of 50 years of age or those with risk factors.
- The diet rich in fruits, vegetables, and whole grains that is high in fiber helps encourage regular bowel movements and lower inflammation.
- Reducing red meat and processed food intake to lower the risk of polyp formation.
- Weight management and regular physical activity to reduce metabolic risk factors.
- Avoiding smoking and excessive alcohol consumption to minimize carcinogenic effects.
- Genetic counseling for individuals with a hereditary predisposition to colorectal cancer.
Frequently Asked Questions (FAQs) on Colon polyps
Are all colon polyps cancerous?
No, most colon polyps are benign and do not cause harm. However, some polyps, particularly adenomatous and serrated types, have the potential to turn into colorectal cancer over time. The likelihood of malignancy depends on factors such as the size, number, and histology of the polyps. Regular screening and removal of polyps help prevent cancer development.
Can colon polyps go away on their own?
No, colon polyps do not typically disappear on their own. Once formed, they remain in the colon until they are removed. If left untreated, some polyps may continue to grow and potentially develop into cancer. This is why routine screening and removal during colonoscopy are important preventive measures.
What foods causes polyps in the colon?
- A higher risk of colon polyps has been associated with foods high in fat, red meat, and processed meats. Pork, beef, and other red meats can raise the risk of colon polyps.
- Processed meats
- Sausage, hot dogs, bacon, and deli meats are examples of processed meats that may increase the risk of colon polyps
- Fried and high-fat foods are associated with a higher incidence of colon polyps.
Do colon polyps cause symptoms?
The majority of colon polyps are found by chance during a standard colonoscopy and are asymptomatic. Larger polyps, on the other hand, may result in iron deficiency anemia from continuous blood loss, abdominal pain, excessive mucous discharge, rectal bleeding, or changes in bowel habits including persistent diarrhea or constipation. A colonoscopy is required to find and remove polyps if these symptoms appear.
Are colon polyps hereditary?
Yes, genetics can influence the likelihood of developing colon polyps. Hereditary conditions like FAP and Lynch syndrome increase the risk of multiple polyps and colorectal cancer. If there is a family history of polyps or colorectal cancer, early and more frequent screening is recommended to detect abnormalities at an early stage.
What are polyps in the colon?
Abnormal tissue growths known as colon polyps form on the rectum's or colon's inner lining. They vary in size, shape, and potential to become cancerous. While most polyps remain benign, certain types, like adenomatous and serrated polyps, can eventually develop into colorectal cancer. They are often detected during routine colonoscopy and can be removed to prevent future complications.
How common are colon polyps?
Colon polyps are quite common, especially in older adults. Studies indicate that about 15–40% of people over the age of 50 will develop polyps in the colon or rectum. The risk increases with age, genetic predisposition, and certain lifestyle factors, such as a diet high in processed foods and red meat.
What causes colon polyps?
The development of colon polyps is caused by aberrant cell proliferation in the colon lining, albeit the precise mechanism is yet unknown. Their development is influenced by a number of factors, including genetic alterations, chronic inflammation, poor eating habits, smoking, excessive alcohol consumption, obesity, and a sedentary lifestyle. Another important risk factor is age, which is more common in those over 50.
How are colon polyps diagnosed?
Colon polyps are usually diagnosed during a colonoscopy, which allows direct visualization of the colon lining. Other diagnostic methods include sigmoidoscopy (for examining the lower colon), CT colonography (a non-invasive imaging test), and stool tests like FIT or FOBT, which detect hidden blood in the stool. If polyps are found, a biopsy is performed to determine their type and potential malignancy.
Can blood tests detect colon polyps?
Blood tests alone cannot directly detect colon polyps, but they may indicate an underlying problem. A complete blood count (CBC) test can reveal anemia, which may result from chronic blood loss due to bleeding polyps. Additionally, stool tests such as FIT and FOBT can help detect hidden blood, prompting further investigation through colonoscopy.
Blood in the stool may be a sign of various gastrointestinal conditions, including colon polyps,
hemorrhoids, diverticulosis, inflammatory bowel disease, or colorectal cancer. Bright red blood suggests bleeding from the lower digestive tract, while dark or tarry stools indicate bleeding higher in the digestive track. A colonoscopy is the best method to determine the exact cause of rectal bleeding.
Yes, a CT colonography, also known as virtual colonoscopy, can detect colon polyps. However, it is not as precise as a traditional colonoscopy, as it cannot remove polyps during the procedure. If a CT scan identifies suspicious polyps, a follow-up colonoscopy is required to confirm the diagnosis and remove them.
Who is at risk for colon polyps?
Colon polyps are likely to develop in people over 50 years of age, those with inflammatory bowel disease, and those with a family history of polyps or colorectal cancer. Additionally, obesity, smoking, high alcohol consumption, a high-fat, low-fiber diet, and a sedentary lifestyle contribute to an increased risk. Regular screening is important for early detection.
Can diet affect the risk of colon polyps?
Yes, the diet has a big impact on the development of colon polyps. A diet consisting in processed foods, red meat, and saturated fats raises the risk of polyps, whereas a diet rich in vegetables, whole grains, and fiber is typically linked to a decreased risk. Fiber promotes bowel regularity and helps remove potential carcinogens from the digestive tract.
How can I prevent colon polyps?
Colon polyps can be prevented by maintaining a healthy lifestyle, including a high-fiber diet, regular physical activity, maintaining an optimum weight, avoiding smoking and excessive alcohol consumption, and undergoing routine colorectal screening. People with a family history of polyps should seek genetic counseling and adhere to more frequent screening recommendations.
Does smoking increase the risk of colon polyps?
Yes, smoking tobacco has been linked to an increased risk of colon polyps, particularly adenomatous polyps, which have a higher likelihood of becoming cancerous. Tobacco exposure leads to chronic inflammation and cellular changes in the intestinal lining, making it a vital risk factor for colorectal cancer as well.
How are colon polyps treated?
Colon polyps are usually resected during a colonoscopy using a technique called polypectomy. This procedure involves the use of biopsy forceps or a snare loop to excise the polyp. In cases where polyps are too large or cannot be removed endoscopically, surgical intervention may be necessary.
Do I need surgery for colon polyps?
Surgery is not typically required for most colon polyps. However, if polyps are very large, recurrent, or suspected to be cancerous, partial colectomy (surgical removal of a section of the colon) may be necessary. Patients with genetic syndromes like FAP may require colectomy to prevent the development of colorectal cancer.
Can colon polyps come back after removal?
Yes, polyps can recur even after removal, which is why follow-up screenings are essential. People with a history of polyps are advised to undergo repeat colonoscopy at intervals recommended by their doctor, usually within 3 to 5 years, depending on the type, size, and number of previous polyps.
How often should I get screened for colon polyps?
For individuals at average risk, colonoscopy is recommended every 10 years starting at age 50. Those with a family history of polyps, previous history of adenomas, or conditions like inflammatory bowel disease may require earlier and more frequent screenings, as often as every 3–5 years.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868