Multidisciplinary Management of Tuberculous Peritonitis in a Patient with Portal Venous Thrombosis and Type 2 Diabetes Mellitus
A 65-year-old male from West Bengal presented to the PACE Hospitals, Hyderabad, with complaints of abdominal distension and pedal edema persisting for two months. The patient had a complex medical history, including diabetes mellitus and peripheral arterial disease (PAD). Current investigations revealed granulomatous inflammation, suggestive of tuberculosis (Koch’s etiology), Which were managed with a multidisciplinary approach.
Chief complaints
A 65-year-old male patient from West Bengal presented to the
PACE Hospitals, Hyderabad, with chief complaints of abdominal distension and pedal edema persisting for 2 months. The patient also reported a weight loss of approximately 3–4 kg over the same period, which he attributed to a persistent loss of appetite.
Medical history
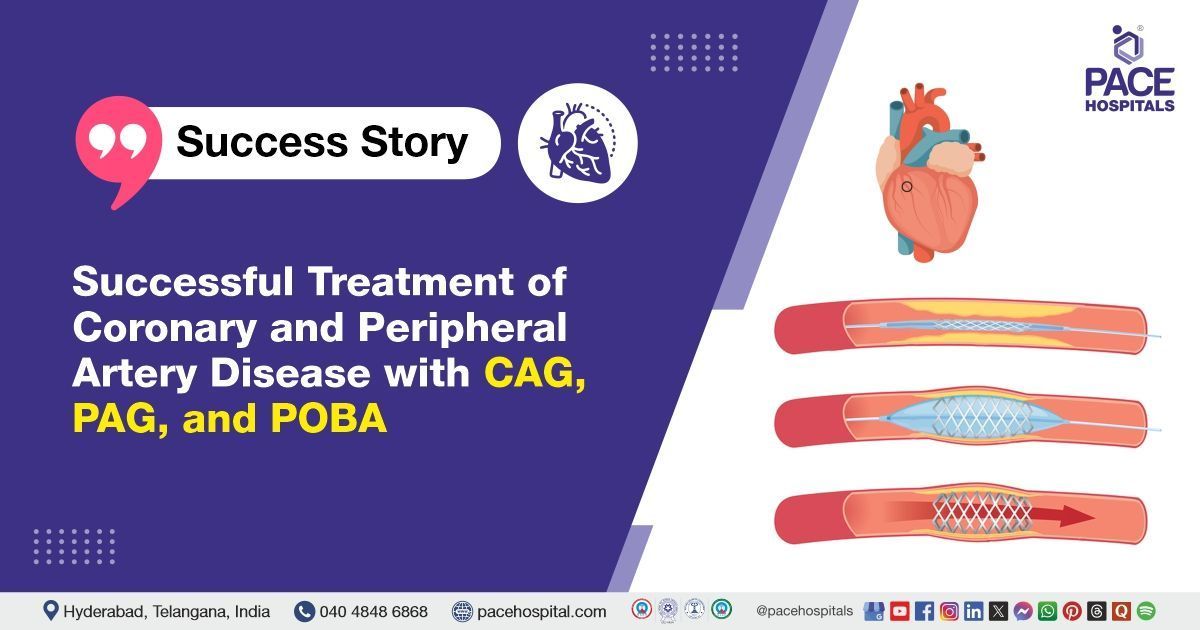
The patient had a complex medical history, including long-standing type 2 diabetes mellitus for over 25+ years and peripheral arterial disease (PAD), for which he underwent iliac arterial stenting twice.
In 2018, portal vein thrombosis (PVT) was incidentally detected during imaging tests, for which esophageal variceal ligations (EVL) procedure was done thrice in 2018, 2019, and 2023 to manage portal hypertension. He also underwent a transurethral resection of the prostate (TURP) in 2023 for urinary obstruction due to benign prostatic hyperplasia (BPH).
A positive Mantoux test result one year ago indicated
tuberculosis exposure, though treatment was not initiated until the time of admission at PACE Hospitals. Therapeutic paracentesis was performed recently, with 1 litre of ascitic fluid drained to relieve symptoms.
General examination
The patient appeared cachexic, with marked muscle wasting and a notably thin appearance, suggesting chronic illness and malnutrition. His skin showed signs of pallor and a petechial rash over the left lateral malleolus, indicative of possible clotting abnormalities or thrombocytopenia.
The oral and nasal mucosa also exhibited dryness, which pointed to dehydration or a metabolic imbalance, further reflecting the patient's compromised overall health. These clinical signs were consistent with advanced systemic inflammation and chronic disease.
Diagnostic investigations
The upper gastrointestinal endoscopy showed scarring from post-esophageal variceal ligations, with the esophageal varices successfully obliterated. Additionally, erosive antral gastritis and mild portal hypertensive gastropathy (PHG) were observed, indicating the ongoing effects of chronic portal hypertension.
Diagnostic laparoscopy and peritoneal biopsy revealed granulomatous inflammation, consistent with Koch’s etiology, confirming the diagnosis of tuberculous peritonitis.
Treatment
The Interventional Gastroenterologist, Transplant Hepatologist, Pancreatologist, and Endosonologist,
Dr. Govind Verma, along with the cross-consulting team of
Dr. Phani Krishna Ravula,
Dr. Pradeep Kiran Panchadi, and
Dr. Abhik Debnath, adopted a multidisciplinary approach, considering the complexity of the patient's condition.
Medical management
Medical management included initiating Anti-Tuberculosis Therapy (ATT) to target tuberculous peritonitis, while intravenous antibiotics were administered to address secondary bacterial infections. Proton Pump Inhibitors (PPI) were prescribed to manage erosive gastritis and portal hypertensive gastropathy (PHG).
Albumin infusion was used to correct hypoalbuminemia and support plasma oncotic pressure, and iron sucrose infusion was administered for anaemia correction. Hepatoprotective drugs were prescribed to improve liver function and manage portal hypertension. Lastly, oral hypoglycemic agents (OHA) were given to maintain optimal blood glucose levels.
The patient had a consultation with the General Medicine department for diabetes management and weight loss evaluation, an appointment with the department of Pulmonology to assess COPD and optimize respiratory care, and a consultation with the department of Dermatology for skin dryness and petechial rash management.
Discharge notes
The patient showed symptomatic improvement during the hospital stay and was discharged in a stable condition. He was advised to adhere to the prescribed medications and dietary recommendations.
Follow-up plan
The patient is scheduled for a follow-up review with Dr. Govind Verma, in the Surgical Gastroenterology Outpatient Department (OPD) after 1 week to assess the response to Anti-Tuberculosis Therapy (ATT) and evaluate overall progress. The patient has been advised to report immediately if symptoms such as severe abdominal pain, fever, or altered sensorium occur.
Impact of portal hypertension and Diabetes mellitus in causing granulomatous peritonitis
Granulomatous peritonitis, portal hypertension, and Type 2 Diabetes Mellitus (DM II) are interconnected, as liver dysfunction caused by portal hypertension can worsen glucose metabolism, complicating the DM II management. Type-2 diabetes mellitus also increases infection risk, making peritonitis treatment challenging. Management involves controlling the underlying peritonitis, using beta-blockers for portal hypertension, and tightly managing blood glucose. Close monitoring of liver function, renal status, and glucose levels, along with lifestyle changes, is essential for optimal care. Regular imaging is needed to track disease progression.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868