Adrenocortical carcinoma - Types, Symptoms, Causes, Treatment & Prevention
PACE Hospitals
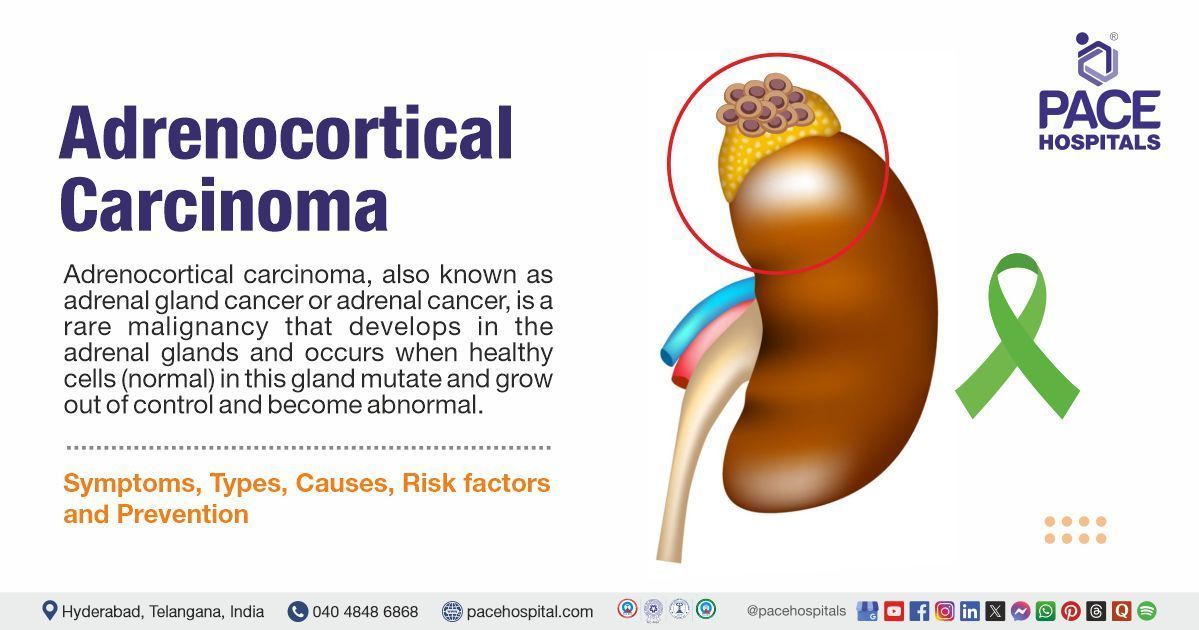
Adrenocortical carcinoma
Adrenocortical carcinoma, also known as adrenal gland cancer or adrenal cancer, is a rare malignancy that develops in the adrenal glands and occurs when healthy cells (normal) in this gland mutate and grow out of control and become abnormal.
Adrenal glands are two tiny, triangular glands that sits on top of each kidney and are responsible for hormone production. Each gland has an inner medulla (adrenal medulla) and an outer cortex (adrenal cortex). Cancerous tumors of the outer part of the adrenal gland are called adrenocortical carcinoma. This cancer can develop in one or both adrenal glands.
Adrenocortical carcinoma meaning
“Adrenal” is derived from Modern Latin from ad- "to, near" + renalis "of the kidneys," from Latin renes "kidneys" meaning "of or near the kidneys,". “Cortex” means an outer layer of tissue.
“Carcinoma” means "a propagating malignant tumour," derived from the Latin "carcinoma", from the Greek "karkinoma", a cancer," from karkinos "a cancer," literally "a crab. “
Adrenocortical carcinoma incidence
Adrenocortical carcinoma (ACC) is an aggressive and uncommon cancer with an incidence of approximately 5 to 20 cases per crore people per year, meaning it affects roughly 5-20 people per crore annually. However, this malignancy accounts for 0.02 to 0.2% of all cancer-related deaths.
Patients with adrenocortical carcinoma are usually either very young (less than 5 years old) or middle-aged (40 to 50s). Women appear to be more likely to develop this cancer than men.
Most patients are diagnosed with advanced-stage disease, leading to a poor prognosis with a 5-year survival rate ranging from 15% to 44%, depending on the stage at diagnosis.
This type of cancer is considered rare in India, with an estimated incidence of about 10 to 20 cases per crore people each year; this incidence aligns with global statistics, which show that it affects a tiny percentage of the population. Most cases are observed in adults aged 30 to 40 years and in children under 6 years old.

Types of adrenal gland cancer
Adrenal cancer is classified based on the location where the cancer originates, including:
- Adrenocortical carcinoma: ACC is the most common form of adrenal cancer, arising in the cortex (outer layer) of the adrenal gland. ACC can be classified into:
- Functioning Tumours: These tumors produce excess hormones, leading to symptoms related to hormone imbalance.
- Non-functioning Tumours: These do not produce hormones and may remain asymptomatic until they grow large.
- Malignant Pheochromocytoma: This rare cancer originates in the inner part of the adrenal gland (medulla) and can cause overproduction of catecholamines, leading to symptoms like high blood pressure (Hypertension), sweating and headaches.
- Malignant adrenal pheochromocytoma: This is very rare and starts in the middle or medulla.
- Neuroblastoma: This type of cancer also begins in the medulla, usually in children.
Adrenocortical carcinoma symptoms
Adrenal cancer symptoms vary depending on whether the tumor is functioning or non-functioning:
Functioning Tumours: May cause hormonal imbalances leading to:
- Weight gain
- Muscle weakness
- High blood pressure
- Diabetes
- Excessive hair growth
- Deepening of the voice
- Irregular menstrual periods in women
- Breast enlargement in men
Non-functioning Tumours: May not cause symptoms until they become large, potentially leading to:
- Abdominal pain or discomfort
- A palpable mass
- Unexplained weight loss
Adrenal cancer causes
Adrenocortical carcinoma (ACC) typically develops sporadically, without a genetic link. In some cases, this cancer has been associated with the following genetic conditions including:
- Genetic Mutations: Conditions including Li-Fraumeni, Beckwith-Wiedemann syndrome and MEN1 increase adrenal cancer risk by affecting tumor suppressor genes.
- Family History: A hereditary predisposition can raise the likelihood of adrenal cancer.
Adrenal cancer risk factors
The exact cause of adrenal gland cancer is not well understood; however, certain conditions may increase the risk, including:
- Family history: People with a close family member who has diagnosed with adrenal cancer or a related genetic syndrome are at heightened risk.
- Age: While adrenal cancer can occur at any age, it is most likely to affect children younger than 5 and adults in their 40s or 50s.
- Poor lifestyle: Certain environmental factors and lifestyles, including smoking and exposure to carcinogens can also increase the risk of cancer.
- Inherited cancer predisposition syndromes: Specific genetic conditions may increase the risk, including:
- Multiple endocrine neoplasia, type 1 (MEN 1): This is a genetic disorder that causes tumours in multiple endocrine glands, increasing the risk of adrenal cancer due to genetic mutations.
- Lynch syndrome: This condition is associated with a higher risk of various cancers due to inherited defects in DNA mismatch repair genes.
- Li-Fraumeni syndrome: It is an uncommon and inherited disorder caused by certain mutations in the TP53 gene, which predisposes individuals to various cancers, including adrenal cancer, due to defective tumor suppressor function.
- Beckwith-Wiedemann syndrome: A genetic disorder involving overgrowth, this syndrome can cause abnormal growth of adrenal tissue, leading to an increased risk of tumors like adrenal cancer.
- Carney complex (CNC): This condition results from mutations in the PRKAR1A gene, increasing the risk of developing adrenal tumors, including adrenal cancer, due to endocrine dysfunction.
Complications of adrenocortical carcinoma
If adrenal cancer is left untreated, it can lead to serious complications, including:
- Severe hormonal problems: The common complications associated with adrenocortical carcinoma (ACC) are due to over-hormone production. Excess production of hormones occurs in 40% to 60% of patients with ACC, causing:
- Hypercortisolism: It is the most common complication causing classic symptoms including fatigue, hypertension, diabetes mellitus, central obesity, muscle weakness/atrophy, and osteoporosis
- Local or regional recurrences: Adrenal cancer recurs in 19% to 34% of patients with no residual (R0) disease after surgery.
- Metastasis: Cancer can spread to organs such as the lungs or liver, worsening prognosis.
Adrenocortical carcinoma diagnosis
Adrenal gland cancer diagnosis involves a combination of a variety clinical evaluation, laboratory tests, and imaging studies to assess hormone levels and detect tumors, including:
General Examination:
- Physical exam and health history
Blood Tests:
- Low-dose dexamethasone suppression test
- High-dose dexamethasone suppression test
- Blood chemistry study
Urine Tests:
- Twenty-four-hour urine test
Imaging Tests:
- CT scan (CAT scan)
- MRI (magnetic resonance imaging)
- PET scan (positron emission tomography scan)
- MIBG scan
Minimally Invasive Tests:
- Adrenal angiography
- Adrenal venography
Biopsies:
- Fine-needle aspiration biopsy
- Core needle biopsy
Adrenal gland cancer treatment
The adrenal cancer treatment depends on the stage, tumor size, and hormone production. It may involve the following:
Surgical Treatments (Adrenal cancer surgery):
- Adrenalectomy (removal of the adrenal gland)
Medication-Based Treatments:
- Adrenal-suppressing drug
- Chemotherapy
- Hormone therapy (to manage excess hormone production)
Radiation Therapy:
- External beam radiation therapy
Targeted Therapy & Other Advanced Treatments:
- Immunotherapy (experimental or clinical trials)
- Targeted drug therapy (for specific mutations)
Adrenal cancer prevention
There is no known way to prevent adrenal cancer because the exact cause is unknown. However, individuals with a family history of genetic syndromes associated with adrenal cancer should consider the following:
- Genetic Counselling & Monitoring: It can help you understand your risk and how to monitor for early signs of cancer. High-risk individuals should undergo regular check-ups for early detection.
- Lifestyle changes: One can reduce their overall risk of cancer by making healthy lifestyle choices, including:
- Avoiding smoking and alcohol consumption
- Maintaining a healthy weight
- Managing risk factors like obesity and hypertension
- Eating a balanced diet with lots of fruits and vegetables
- Being physically active
- Avoiding exposure to cancer-causing chemicals
Difference between Adrenocortical adenoma and Carcinoma
Adrenocortical adenoma vs carcinoma
Though both affect the adrenal glands, the most significant difference lies in their malignant potential and clinical behaviour, including:
| Elements | Adrenocortical adenoma | Adrenocortical carcinoma |
|---|---|---|
| What is it | It is a more common non-cancerous (benign) tumour that grows in the adrenal cortex | It is rare and aggressive cancerous (malignant) tumour that originates in the adrenal glands. |
| Size | Typically, smaller (< 5 cm) | Larger, usually > 5 cm |
| Causes | Typically, idiopathic (unknown cause) | Genetic mutations |
| Symptoms | Often asymptomatic (found incidentally) | Symptoms often related to hormone secretion |
| Metastasis | No metastasis (No spreading) | Metastasis to liver, lungs, or lymph nodes |
| Treatment | Laparoscopic surgery, surgery (adrenalectomy), observation if non-functional | Surgical resection (adrenalectomy), adjuvant therapy, chemotherapy, radiotherapy, targeted therapy and targeted therapy |
Frequently Asked Questions (FAQs) on Adrenal cancer
Is adrenal cancer hereditary?
Most adrenal cortex cancers are not inherited (they are sporadic); certain genetic factors are more likely to be involved in up to 15% of adrenal cancers in children. It is linked to genetic syndromes such as Li-Fraumeni syndrome, Lynch syndrome, or Beckwith-Wiedemann syndrome. If there is a family history of adrenal cancer or related conditions, genetic testing may be recommended.
Is adrenal gland cancer fatal?
Adrenal cancer can be aggressive and may be fatal, especially if diagnosed at a late stage. However, survival rates may vary from person to person depending on the stage at diagnosis and response to treatment.
Is adrenal cancer curable?
There’s always a chance for a cure when the tumour is only in early stages, detected early and hasn’t spread to other regions of body (metastasis). Adrenalectomy (surgical removal) is the main curative treatment for adrenal cancer. If cancer has spread beyond the adrenal gland, a cure is less likely. However, treatment can slow tumour growth and enhance quality of life.
Can stress cause adrenal cancer?
No, stress doesn't cause adrenal cancer. However, chronic stress raises the risk of several diseases, such as depression, cardiovascular disease, endocrine disorder, inflammation and cancer. Chronic stress can cause changes in the neuroendocrine-immune system. Stress hormones can promote tumorigenesis, support cancer growth and progression, and regulate the tumor microenvironment.
Who treats adrenal cancer?
Adrenal cancer is treated by a multidisciplinary team of specialists, including endocrinologists,
oncologists, surgeons, and radiation oncologists. Endocrine surgeons or surgical oncologists usually perform adrenal gland removal, while medical oncologists manage chemotherapy and targeted therapies.
What age do people get adrenal cancer?
Adrenal cancer can occur at any age; however, it is most common in children under five and middle-aged adults, with the average age of diagnosis being 46, affecting adults between 40 and 60 years old.
What is the life expectancy of someone with adrenal cancer?
The life expectancy for someone with adrenal cancer depends mainly on the stage at which the cancer is diagnosed. The 5-year survival rate generally ranges from 50% for early-stage localized tumors to as low as 10-20% when cancer has spread to other organs. This means that early detection can greatly improve the prognosis.
Can you live with adrenal cancer?
Yes, it is possible to live with adrenal cancer, particularly if diagnosed early and treated effectively. Survival depends on factors like the cancer stage, response to treatment, and overall health. Advanced cases may require ongoing treatment to manage symptoms and slow disease progression.
A healthcare professional may suspect cancer in adrenal glands based on patient-specific symptoms, such as excessive hair growth or unexplained weight changes. However, sometimes, healthcare professionals find adrenal tumours after taking a computed tomography (CT) scan or MRI (magnetic resonance imaging) for other reasons.
Adrenal cancer is diagnosed through a combination of imaging tests (CT scan, MRI, or PET scan), urine and blood tests to check hormone levels, and a biopsy if needed. Surgical oncologists may also use adrenal vein sampling to confirm the tumor's origin.
Treatment of adrenal cancer depends on the size and location of the tumor, and whether it has spread outside of the adrenal gland. Adrenal cancer is primarily treated with surgery to remove the tumor, often through adrenalectomy. If the cancer has spread to other areas of the body, radiation therapy, chemotherapy, and targeted drugs therapy will be used to slow its growth and manage symptoms.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles