Radiculopathy Treatment in Hyderabad, India
PACE Hospitals is regarded as a leading hospital for radiculopathy treatment in Hyderabad, Telangana, India. Our expert team of neurologists, neurosurgeons, orthopaedic specialists, and physiotherapists offers a multidisciplinary approach to diagnose and manage radiculopathy—a condition caused by compression or inflammation of spinal nerve roots, often leading to pain, tingling, numbness, or weakness.
Using advanced diagnostic tools such as MRI, CT scan, nerve conduction studies, and electromyography (EMG), we accurately identify the affected nerves and the underlying causes, such as herniated discs, spinal stenosis, or degenerative spine diseases.
Treatment options are personalized for each patient and may include medications, physiotherapy, spinal injections, or surgery, depending on the severity. Our goal is to relieve nerve pain, restore function, and enhance the quality of life through expert care and ongoing support.
Book an appointment for
Radiculopathy Treatment
Radiculopathy Treatment Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Quick Navigation
Why Choose PACE Hospitals for Radiculopathy Treatment?
State-of-the-art diagnostic - MRI, CT, nerve conduction studies, and EMG
Expert Spine Specialists and Neurosurgeons in Hyderabad for Radiculopathy
Comprehensive Non-Surgical & Minimally Invasive Surgical Options
Affordable & Transparent Radiculopathy Treatment with Insurance & Cashless Options
Radiculopathy Diagnosis
Diagnosis of radiculopathy involves several steps to identify the disease and its underlying causes. The following are the steps involved in diagnosing radiculopathy:
Initial evaluation
- Medical history: This is an important step in the diagnosis of radiculopathy as it helps in identifying the symptoms such as pain, weakness which are the characteristic symptoms of radiculopathy. It also helps in identifying risk factors such as age, trauma or degenerative conditions which may compress the nerve roots.
- Physical examination
- Muscle strength and reflexes: This helps in identifying the specific patterns of weakness which correspond to the affected nerve root. For example, weakness in the quadriceps can indicate L4 nerve root involvement and weakness in foot dorsiflexion indicates L5 involvement. Diminished or absent reflexes can indicate nerve root dysfunction.
- Sensory testing: In this test, simple bedside tests such as assessing touch sensitivity with a monofilament, pain perception with a pinprick, and temperature sensitivity are performed. They help in identifying nerve root involvement by detecting sensory disturbances, such as increased or decreased sensitivity.
- Lasegue’s sign: In this test the patient is made to lie in the supine position, the knee is extended, the ankle dorsiflexed, and the cervical spine is flexed. The examiner then lifts the patient’s lower extremity off the table towards 90 degrees, which brings out radicular pain as the nerve root is stretched.
Diagnostic tests
Based on the above information, neurosurgeons and orthopedic specialists advise some diagnostic tests for radiculopathy. The following are the tests that might be recommended to diagnose radiculopathy:
- Imaging studies
- Magnetic resonance imaging (MRI): These are the primary imaging tests used for the diagnosis of radiculopathy, particularly cervical and lumbar radiculopathy. It provides excellent visualization of soft tissues including the spinal cord, nerve roots and intervertebral discs and helps in identifying the level of nerve compression.
- Computed tomography (CT) scan: This imaging studies provide detailed visualization and clear images of bony structures, making them able to identify conditions such as osteophytes or fractures which contribute to the development of radiculopathy.
- X-ray: These imaging studies are useful in the identification of bony abnormalities such as fractures, osteoarthritis, and scoliosis. It also helps in visualizing the narrowing of neural foramina which indicates nerve compression.
- Electrodiagnostic tests
- Electromyography: This test plays an important role in the diagnosis of radiculopathy. It can evaluate the electrical activity of the skeletal muscle and nerves which control them, and also helps in the identification of abnormalities which may indicate nerve root involvement.
- Nerve conduction studies: Despite lower utility, these tests are an important part of electrodiagnostic tests in radiculopathy diagnosis. These tests can evaluate the strength of electrical signals and can detect abnormalities, which can be useful in ruling out other conditions that might mimic radiculopathy, such as peripheral neuropathy.
Radiculopathy Differential Diagnosis
Differential diagnosis of radiculopathy generally includes considering various conditions which can mimic or cause similar symptoms, such as radiating pain, numbness, or weakness. The following are some of the conditions which mimic lumbosacral radiculopathy:
- Herniated disc: It is also known as slipped disc or ruptured disc. This condition occurs when the soft, jelly-like inner part of a spinal disc pushes through a crack in the tough outer layer, potentially compressing nearby nerves. Pain in the back, buttocks or legs; numbness, tingling sensation in the affected area and loss of bowel or bladder function are some of the symptoms of herniated disc.
- Lumbosacral plexopathy: It is a condition which involves injury to the nerves in the lumbosacral plexus area, which is a network of nerves formed by the anterior rami of the lumbar and sacral spinal cord. Pain in the lower back, buttocks, or legs, weakness and tingling sensations in the legs and feet are the symptoms of lumbosacral plexopathy.
- Lumbar spinal stenosis: It is defined as the narrowing of the spinal canal in the lower back, which compresses nerves and blood vessels. Back pain while standing or walking, Pain which radiates down the buttocks, numbness, tingling and weakness in legs are the symptoms of lumbar spinal stenosis.
- Mononeuropathies: It is defined as the damage or dysfunction of a single nerve outside the brain and spinal cord, which can cause loss of function in the area that nerve innervates. The symptoms of mononeuropathies include pain, numbness or tingling sensations, weakness and difficulty in moving the affected area.
- Diabetic amyotrophy: It is also called as diabetic lumbosacral radiculoplexus neuropathy (DLRPN). This is a rare complication of diabetes, which is characterized by asymmetrical pain and weakness in the proximal lower limbs, affecting the hips and thighs. Severe pain in the hips, thighs, and buttocks; weakness in the affected muscles which makes it difficult to walk or stand are some of the symptoms of diabetic amyotrophy.
- Cauda equina syndrome: This is a rare and serious neurological condition which is caused by compression or damage to the bundle of nerve roots at the lower end of the spinal cord. Severe low back pain, pain which radiates down the legs, numbness or weakness in one or both legs are some of the symptoms of cauda equina syndrome.
Radiculopathy Treatment Goals
The primary treatment goal of radiculopathy focuses on treating symptoms and restoring the normal nerve function. The following are some of the treatment goals of radiculopathy:
- To decrease pain and inflammation using medications such as non-steroidal anti-inflammatory drugs and opioids.
- To improve function, mobility and strength of the muscles by engaging in various physical activities and exercises.
- To reduce strain and pressure on the spine which is caused by excessive body weight or by lifting heavy objects.
Book online appointment
Treatment of radiculopathy usually depends on the location, the cause of the condition and on various other factors. Non-surgical treatment is recommended first before opting for surgery. The following are the steps involved in treating radiculopathy:
Non-surgical treatment
- Medications
- Non-steroidal anti-inflammatory drugs (NSAIDs): These drugs are commonly used to manage pain and inflammation, and they act by inhibiting the cyclooxygenase (COX) enzymes that are involved in the production of prostaglandins which cause pain and inflammation
- Opioids: These drugs are sometimes considered for treating pain when other treatments fail to provide adequate pain relief. They provide short-term pain relief for various types of chronic pain, including neuropathic pain conditions.
- Muscle relaxants: These are used to alleviate muscle spasms which are associated with radiculopathy. They can provide temporary relief and improve patient comfort, and can help in managing symptoms by reducing muscle tension.
- Physical therapy: Engaging in exercises that are designed to strengthen the muscles around the spine and improve flexibility, which can help in stabilizing the spine and reducing the pressure on nerves. Following proper posture helps in reducing pressure on the spinal discs and nerves, promoting healing and preventing further injury.
- Lifestyle modifications
- Weight loss: Excess body weight puts extra pressure on the spine and joints, thereby causing nerve compression and leading to radiculopathy symptoms. Losing weight and maintaining body weight can help in reducing this pressure, potentially reducing pain and discomfort. Weight loss can also increase the mobility and physical activity of the patient, which helps in reducing the strain on the affected nerves.
- Injections
- Steroid injections: These injections play a significant role in treating radiculopathy, especially for treating radicular pain which is associated with spinal conditions such as herniated discs and spinal stenosis. They provide moderate short-term relief from radicular pain, particularly in the lumbar area.
- Nerve root injections: These injections are composed of corticosteroids and local anesthetics. While corticosteroids reduce inflammation around the nerve root, local anesthetics provide immediate pain relief. These are generally recommended after conservative treatments or non-surgical treatment such as medications and physical therapy have failed to manage pain effectively.
Surgical treatment
Patients with severe or progressive neurological deficits (like severe weakness), cauda equina syndrome, or those who do not improve following an appropriate trial of conservative management (usually 6–12 weeks) may be candidates for surgery.
Common Surgical Procedures:
- Discectomy/Microdiscectomy: The most common procedure for lumbar radiculopathy is the removal of the herniated disc material that is compressing the nerve root.
- Laminectomy: In cases of spinal stenosis, the lamina, or portion of the vertebral bone, is removed in order to decompress the nerve root.
- Foraminotomy: More frequently seen in cervical radiculopathy, neural foramen widening relieves nerve compression.
- Fusion procedures: Considered in cases involving recurrent symptoms or instability.
Radiculopathy Prognosis
In lumbosacral radiculopathy, the majority of the patients tend to resolve with conservative management. However, for those patients requiring surgical intervention, a study indicated that among 100 patients undergoing discectomy, 73 percent of the patients achieved complete relief of leg pain and 63 percent of the patients had complete relief of back pain at the 1-year follow-up. These numbers have remained stable at the 5- to 10-year follow-up, with 62 percent of patients reporting complete relief in both categories. Only 5 percent of the patients were qualified as having failed back syndrome at the 5- to 10-year follow-up.
Around 85 percent of acute cervical radiculopathy resolves without any specific treatments within 8 to 12 weeks. A number of surgical procedures are available for treating radiculopathy, and they all have the potential to cause serious complications. Patients who do not show improvement are considered for surgery as a last resort.
Frequently Asked Questions (FAQs) on Radiculopathy
What are the symptoms of radiculopathy?
Sharp pain in the back, arms, legs, or shoulders, weakness or loss of reflexes in the arms or legs, numbness of the skin, a pins-and-needles sensation, or other abnormal sensations in the arms or legs are some of the symptoms of radiculopathy.
Who is more at risk for developing radiculopathy?
Individuals with a family history of radiculopathy, who have a history of other spine disorders, and individuals involved in strenuous activities such as heavy lifting and repetitive motions are at higher risk of developing radiculopathy.
Can bad posture cause radiculopathy?
Yes, bad or poor posture, especially forward head posture (FHP) can cause radiculopathy. Forward head posture can increase stress on the spine including cervical and lumbar regions. This stress can cause nerve root compression, which is one of the main causes of radiculopathy.
What are the complications of radiculopathy?
When left untreated radiculopathy can progress to chronic pain and can lead to various other complications. Disability, muscle atrophy, difficulty in walking or moving, cauda equina syndrome, severe lumbar radiculopathy, weight gain, muscle loss, depression, and chronic pain are some of the complications of radiculopathy.
How can radiculopathy be prevented?
Radiculopathy cannot always be prevented, but there are a few measures which helps in reducing the risk of development. By following certain measures such as staying physically active, maintaining body weight, maintaining good posture and proper heavy lifting techniques, managing stress and smoking cessation can help in preventing radiculopathy.
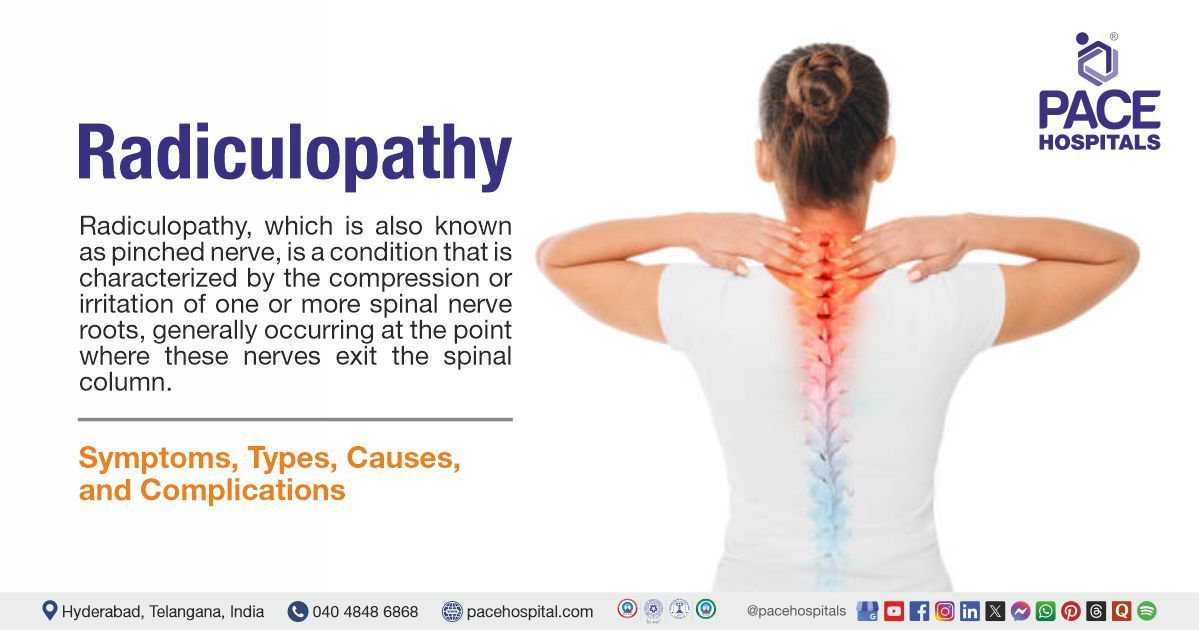
What is radiculopathy?
It is a condition which is characterized by the compression or irritation of one or more spinal nerve roots, generally occurring at the point where these nerves exit the spinal column. It is described as radicular pain that radiates along the path of the affected nerve.
What are the causes of radiculopathy?
There are various causes of radiculopathy; some involve spinal injury, and others are caused by the development of spinal conditions. Bone spurs (bony overgrowths which develop in the vertebrae), osteoarthritis, spinal stenosis (a narrowing of the spinal column), scoliosis (a condition where the spine curves abnormally), and spinal tumors are some of the causes of radiculopathy.
What are the symptoms of cervical radiculopathy?
The symptoms of cervical radiculopathy vary based on the severity of the condition. Neck pain, shoulder and back pain, weakness or numbness, and reduced range of motion are some of the symptoms of cervical radiculopathy.
What are the symptoms of thoracic radiculopathy?
The symptoms of thoracic radiculopathy may vary from patient to patient. Chest pain, torso pain, burning nerve pain felt, which is felt in the rib cage, down the sides of the body, in the abdomen, and numbness or tingling sensation in the areas affected are some of the symptoms of thoracic radiculopathy.
What are different types of radiculopathy?
Based on the location of the affected spine, radiculopathy is primarily of three main types: lumbar radiculopathy, cervical radiculopathy, and thoracic radiculopathy. Lumbar radiculopathy occurs in the lower back, and it is also known as sciatica, as the nerve roots which make up the sciatic nerve are often involved.
Cervical radiculopathy occurs when a nerve in the neck is compressed or irritated at the point where it leaves the spinal cord. Thoracic radiculopathy refers to the compressed nerve root in the thoracic area of the spine, which is the upper back.
What is lumbosacral radiculopathy?
It is a condition characterized by pain and/or neurologic symptoms which radiate in one or more lumbar or sacral dermal segments. It results from compression of lumbar nerve roots in the lumbosacral spine area.
Can cervical radiculopathy cause paralysis?
Yes, cervical radiculopathy can cause paralysis. When a nerve root in the cervical spine is compressed, it can lead to symptoms such as pain, muscle weakness, numbness, and tingling in the arm or hand. Prolonged or severe compression of the nerve root can ultimately lead to paralysis.