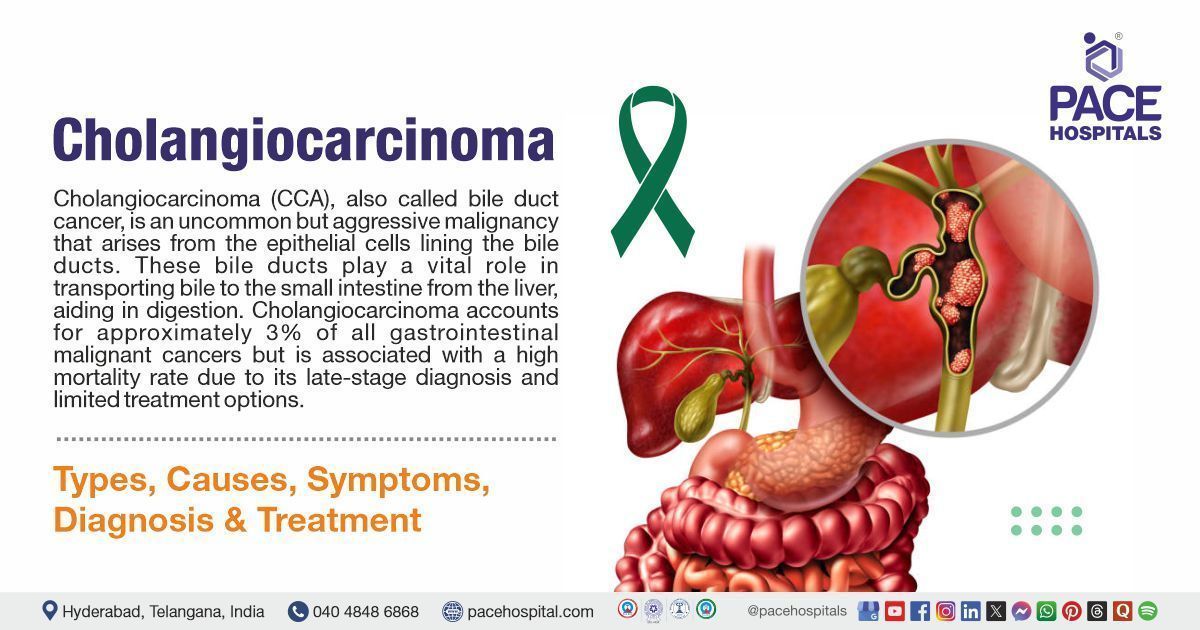
Cholangiocarcinoma (Bile Duct Cancer): Symptoms, Causes, Types, Staging, Treatment & Prevention
Cholangiocarcinoma (CCA), also called bile duct cancer, is an uncommon but aggressive malignancy that arises from the epithelial cells lining the bile ducts. These bile ducts play a vital role in transporting bile to the small intestine from the liver, aiding in digestion. Cholangiocarcinoma accounts for approximately 3% of all gastrointestinal malignant cancers but is associated with a high mortality rate due to its late-stage diagnosis and limited treatment options.
Cholangiocarcinoma meaning
The term cholangiocarcinoma is derived from Greek roots:
- "Cholangio-" (Greek: chole = bile + angeion = vessel) → Refers to the bile ducts.
- "Carcinoma" (Greek: karkinōma = cancerous tumor) → Refers to a malignant tumor of epithelial origin.
Thus, cholangiocarcinoma literally means "a malignant tumor of the bile ducts."
The disease is often asymptomatic in its early stages, leading to delayed detection and poor prognosis. Some of the commonly seen symptoms are jaundice, pruritus, abdominal pain, and weight loss. The pathogenesis of cholangiocarcinoma is complex and multifactorial, involving chronic inflammation, genetic predisposition, and environmental factors. Though there are advancements in the diagnosis and treatment of cholangiocarcinoma, curative options remain restricted, making early detection and targeted therapies a crucial focus of ongoing research.
Cholangiocarcinoma Types
Cholangiocarcinoma is classified based on its anatomical location within the biliary tree. This classification helps determine clinical presentation, treatment options, and prognosis.
Intrahepatic Cholangiocarcinoma (iCCA)
- Intrahepatic Cholangiocarcinoma (iCCA) originates from the small bile ducts within the liver, accounting for 10–20% of all cholangiocarcinoma cases. It is often mistaken for hepatocellular carcinoma (HCC) due to its intrahepatic location.
- iCCA typically presents at an advanced stage due to the absence of early symptoms and can develop as single or multiple nodules, sometimes infiltrating the surrounding liver parenchyma.
Hilar Cholangiocarcinoma (hCCA) or Klatskin Tumor
- Hilar Cholangiocarcinoma (hCCA) or Klatskin Tumor is the most common subtype, accounting for 50–60% of cases, and arises at the confluence of the right and left hepatic ducts, often leading to bile duct obstruction and early-onset jaundice. It is also called perihilar cholangiocarcinoma (pHCC).
- hCCA typically presents as a locally advanced disease, making surgical resection challenging, and frequently invades adjacent vascular structures, further complicating curative treatment.
Distal Cholangiocarcinoma (dCCA)
- Distal Cholangiocarcinoma (dCCA) arises in the common bile duct near the pancreas, accounting for 20–30% of cholangiocarcinoma cases, and often presents early due to biliary obstruction.
- dCCA is sometimes misdiagnosed as pancreatic cancer due to its anatomical proximity, and surgical resection (the Whipple procedure) remains the preferred treatment for resectable tumors.
In addition to anatomical classification, CCA can also be categorized histologically, with adenocarcinoma being the predominant subtype. Other rare histological forms include mucinous carcinoma and squamous cell differentiation.
Cholangiocarcinoma staging
Cholangiocarcinoma staging is typically based on the TNM (Tumor, Node, Metastasis) system and varies depending on the location of the tumor (intrahepatic, perihilar, or distal). The AJCC (American Joint Committee on Cancer) staging system is commonly used.
General Staging
- Stage 0 (Carcinoma in situ) – Abnormal cells are present but have not spread to deeper tissues.
- Stage I – A localized tumor confined to the bile ducts.
- Stage II – Tumor invades nearby structures but no lymph node involvement.
- Stage III – Tumor has spread to regional lymph nodes or major blood vessels.
- Stage IV – There is distant metastasis to organs like the liver, lungs, or peritoneum.
Cholangiocarcinoma Symptoms
Cholangiocarcinoma is often asymptomatic in its early stages, leading to a delayed diagnosis. Symptoms may differ based on the tumor location.
Intrahepatic Cholangiocarcinoma (iCCA)
The symptoms of intrahepatic cholangiocarcinoma are usually asymptomatic in early stages.
Symptoms of advanced disease include:
- Right upper quadrant pain
- Unintentional weight loss and fatigue
- Hepatomegaly (enlarged liver)
- Mild jaundice (in later stages)
- Ascites due to peritoneal carcinomatosis in advanced cases.
Hilar and Distal Cholangiocarcinoma
Symptoms of hilar and distal cholangiocarcinoma are more likely to present with bile duct obstruction.
Some of the symptoms include:
- Painless Jaundice: Jaundice is one of the most common presenting feature.
- Pruritus: Pruritus occurs due to bile salts accumulation in the skin.
- Dark Urine and Pale Stools: Disrupted in bilirubin metabolism may result in dark urine and pale stools
- Abdominal Pain: Pain in the abdomen is more common in distal cholangiocarcinoma
- Cholangitis: In case of any infection, cholangitis is observed which is characterized by fever, chills, and sepsis.
- Anorexia and Nutritional Deficiencies: Cholestasis and malabsorption lead to nutritional deficiency and anorexia in patients with cholangiocarcinoma.
Paraneoplastic and Systemic Symptoms
- Fatigue
- Night sweats
- Unexplained blood clotting (Trousseau syndrome).
- Metastatic disease may cause ascites, bone pain, or respiratory complications.
- Hypercalcemia and cachexia in advanced-stage disease.
Cholangiocarcinoma Causes and risk factors
Cholangiocarcinoma results from chronic inflammation, bile duct injury, and genetic mutations. Below are some of the risk factors that might increase the likelihood of developing this malignancy.
Chronic Biliary Inflammation
Cholangiocarcinoma (CCA) risk factors related to chronic biliary inflammation include primary sclerosing cholangitis, chronic hepatitis B and C infections, recurrent biliary infections, gallstones and chronic cholecystitis:
- Primary Sclerosing Cholangitis (PSC): Primary sclerosing cholangitis is a major risk factor for cholangiocarcinoma. Between 2% to 8% of cases of CCA are found in patients with PSC, and it is the leading cause of death in these patients. The lifetime incidence of CCA among PSC patients ranges from 6 to 36%.
- Chronic Hepatitis B and C Infection: Chronic viral hepatitis is a known risk factor for CCA. Hepatitis B and C contribute to hepatobiliary carcinogenesis, increasing the risk of CCA.
- Recurrent Biliary Infections: Recurrent biliary infections are a risk factor, especially in individuals infected with liver flukes like *Clonorchis sinensis* and *Opisthorchis viverrini*, which are common in Southeast Asia
- Gallstones and Chronic Cholecystitis: Gallstones and chronic cholecystitis can cause persistent irritation of the bile duct epithelium, potentially leading to malignant transformation. Studies have revealed a link between CCA and choledocholithiasis and cholangitis, with risk estimates ranging from 4–64. Primary biliary stones can cause chronic biliary tract inflammation, which raises the risk of cancer.
Congenital Biliary Abnormalities
- Choledochal Cysts: Choledochal cysts can lead to bile stasis, increasing the risk of malignant transformation. Cholangiocarcinoma is a common malignancy associated with choledochal cysts. Patients with choledochal cysts have an increased chance of developing malignancy, a risk that increases with age.
- Caroli Disease: Caroli disease is characterized by bile duct dilatation, predisposing individuals to chronic cholangitis and the development of cholangiocarcinoma (CCA). Choledochal malformations are generally considered premalignant conditions, which increases the risk of developing malignancy.
- Biliary Atresia: It is a congenital condition that disrupts bile flow, increasing the long-term risk of cancer. Malignancies develop at a higher rate in patients with biliary cysts compared to the general population.
Environmental and Lifestyle Factors
Some of the environmental and lifestyle factors that can increase the risk of cholangiocarcinoma (CCA) include exposure to industrial carcinogens, smoking, alcohol consumption, obesity and diabetes mellitus, and high consumption of processed foods.
- Exposure to Industrial Carcinogens: Exposure to dioxins and nitrosamines are directly linked to an increased risk of CCA. Some industrial chemicals, when used as cleaning agents, have been reclassified as carcinogens after an outbreak of cholangiocarcinoma in workers exposed to high levels of these chemical.
- Smoking and Alcohol Consumption: Tobacco smoking and alcohol consumption can lead to bile duct epithelial damage, increasing the likelihood of malignancy. People who drink alcohol are more likely to get intrahepatic bile duct cancer.
- Obesity and Diabetes Mellitus: Obesity and diabetes mellitus can cause metabolic and inflammatory changes that may contribute to the CCA development.
- High Consumption of Processed Foods: Diets rich in nitrosamines and preservatives may play a role in oncogenesis.
Genetic and Epigenetic Factors
- Genetic Mutations: Mutations in genes like BAP1, IDH1/IDH2, and TP53 are commonly found in cholangiocarcinoma.
- Epigenetic Changes: DNA methylation, histone modifications, and non-coding RNA dysregulation contribute to tumorigenesis.
- Familial Cholangiocarcinoma: Although rare, familial predisposition suggests genetic susceptibility in some cases.
Despite these risk factors, many cases of cholangiocarcinoma occur sporadically without a known predisposing condition.
Diagnosis of Cholangiocarcinoma
Since cholangiocarcinoma often presents with non-specific symptoms, early and accurate diagnosis requires a combination of imaging, laboratory tests, and histopathological confirmation.
- Laboratory Tests
- Liver Function Tests (LFTs): Elevated bilirubin, alkaline phosphatase (ALP), and gamma-glutamyl transferase (GGT) suggest bile duct obstruction.
- Tumor Markers:
- CA 19-9 (Carbohydrate Antigen 19-9): Elevated in 50–75% of patients with CCA but also increased in benign biliary diseases.
- CEA (Carcinoembryonic Antigen): May be elevated in some cases but lacks specificity.
- AFP (Alpha-Fetoprotein): Helps differentiate CCA from hepatocellular carcinoma (HCC).
- Imaging Studies
- Ultrasound: First-line imaging to detect bile duct dilation or mass.
- CT Scan (Multiphasic): Provides detailed information about tumor size, vascular involvement, and metastases.
- MRI/MRCP (Magnetic Resonance Cholangiopancreatography): The best imaging modality for visualizing bile ducts and identifying strictures or masses.
- PET-CT (Positron Emission Tomography-CT): Useful for detecting distant metastases and lymph node involvement.
- Endoscopic and Histopathological Evaluation
- ERCP (Endoscopic Retrograde Cholangiopancreatography): Used for bile duct visualization, biopsy, and stent placement in cases of obstructive jaundice.
- EUS (Endoscopic Ultrasound): Helps in assessing tumor depth and lymph node involvement.
- Percutaneous Biopsy: For histological confirmation, especially in unresectable cases.
- Molecular and Genetic Testing
- IDH1/IDH2, FGFR2, and BRAF mutations: Guide targeted therapies in advanced cases.
- MSI (Microsatellite Instability) and NTRK fusion: Help determine eligibility for immunotherapy.
Cholangiocarcinoma Treatment
Treatment varies based on tumor location, stage, and patient fitness. It includes surgery, chemotherapy, targeted therapy, radiation, and palliative care.
Cholangiocarcinoma Surgery
Surgical resection remains the only curative treatment for cholangiocarcinoma, but eligibility depends on tumor size, vascular invasion, and lymph node involvement.
- Intrahepatic Cholangiocarcinoma (iCCA): Requires partial hepatectomy or liver lobectomy.
- Hilar Cholangiocarcinoma (hCCA): Extended hepatectomy with bile duct resection and lymphadenectomy is performed for eligible patients.
- Distal Cholangiocarcinoma (dCCA): Treated with a Whipple procedure (pancreaticoduodenectomy).
Liver Transplantation
Selected patients with early-stage hilar CCA (under strict protocols) may benefit from liver transplantation combined with neoadjuvant therapy. This approach offers long-term survival for well-selected cases.
Chemotherapy
For unresectable, recurrent, or metastatic cholangiocarcinoma, chemotherapy is the mainstay of treatment.
- First-line Chemotherapy: Anti metabolites along with alkalizing agents are the standard regimen for advanced disease.
- Second-line Chemotherapy: The FOLFOX class of drugs are given for patients who do not respond to first line chemotherapy.
- Adjuvant Chemotherapy: Immunosuppressive agents are often used post-surgery to reduce recurrence risk.
Radiation Therapy
Radiation is useful for locally advanced, unresectable, or post-operative cases.
- External Beam Radiation Therapy (EBRT): Helps control tumor growth and relieve symptoms.
- Stereotactic Body Radiation Therapy (SBRT): Delivers precise high-dose radiation, minimizing damage to healthy tissues.
- Brachytherapy (Internal Radiation): Sometimes used in combination with palliative biliary stenting.
Palliative and Supportive Care
For patients with unresectable or metastatic disease, symptom control is essential.
- Biliary Drainage (Stenting): Relieves jaundice and improves quality of life.
- Pain Management: Includes opioids and nerve blocks for pain relief.
- Nutritional Support: Aims to manage cachexia and improve overall well-being.
Cholangiocarcinoma Prognosis and survival
Cholangiocarcinoma has a poor prognosis, with a 5-year survival rate varying by stage and treatment.
- Localized Disease (Resectable Tumors): 5-year survival rate ~25–40%.
- Locally Advanced Disease (Unresectable): Median survival ranges from 6–12 months with palliative chemotherapy.
- Metastatic Disease: 5-year survival rate <5%, with median survival of less than 1 year.
Prognostic factors
- Early detection and complete surgical resection (R0 resection) significantly improve survival.
- Lymph node involvement and vascular invasion worsen prognosis.
- Patients with targetable mutations (e.g., IDH1, FGFR2) may benefit from newer therapies.
Prevention of cholangiocarcinoma
While many risk factors like age and genetics can't be controlled, you can lower your risk of bile duct cancer. Key steps include maintaining a healthy weight, staying physically active, eating a healthy diet, limiting alcohol, and not smoking. Taking precautions to avoid hepatitis and other infections are also important.
Frequently Asked Questions (FAQs) on Cholangiocarcinoma (Bile duct cancer)
What causes cholangiocarcinoma?
The exact cause is unknown, but risk factors include chronic inflammation of the bile ducts, primary sclerosing cholangitis (PSC), liver fluke infection, chronic viral hepatitis (B and C), cirrhosis, bile duct cysts, and exposure to certain chemicals like Thorotrast. Genetic mutations also contribute to tumor development.
What are the symptoms of cholangiocarcinoma?
Symptoms often appear late and include jaundice (yellowing of skin and eyes), dark urine, pale stools, pruritus (itching), unexplained weight loss, abdominal pain (especially in the right upper quadrant), nausea, vomiting, and fever. Some patients may develop hepatomegaly or a palpable mass.
Is cholangiocarcinoma hereditary?
Most cases are sporadic, but genetic predisposition may play a role. Mutations in genes like IDH1/2, FGFR2 fusions, and BAP1 have been implicated. A family history of biliary cancer or Lynch syndrome slightly increases the risk, but routine genetic screening is not standard.
What are the complications of cholangiocarcinoma?
Complications include biliary obstruction, leading to jaundice, cholangitis (bile duct infection), liver failure, ascites, and metastasis to the lymph nodes, lungs, peritoneum, and bones. Severe pruritus and malnutrition are common in advanced cases, significantly affecting the quality of life.
Can cholangiocarcinoma recur after treatment?
Yes, recurrence is common even after surgery. Local recurrence or distant metastasis often occurs within two years. Regular follow-ups with imaging and CA 19-9 monitoring are essential. Adjuvant chemotherapy and targeted therapies may be considered to delay recurrence.
What is cholangiocarcinoma?
Cholangiocarcinoma is a rare but aggressive cancer that originates in the bile ducts, which carry bile from the liver to the small intestine. It can develop anywhere along the biliary tract and is classified into intrahepatic, perihilar, and distal types. It often presents at an advanced stage due to its silent progression, making early detection challenging.
What are the types of cholangiocarcinoma?
Cholangiocarcinoma is classified based on its location:
- Intrahepatic: Arises within the liver.
- Hilar (Klatskin tumor): Occurs at the junction of right and left hepatic ducts.
- Distal: Develops in the bile ducts near the small intestine.
Each type has different treatment approaches and prognosis.
How is cholangiocarcinoma diagnosed?
Diagnosis involves a combination of imaging tests like ultrasound, CT scans, MRI/MRCP, and PET scans. Blood tests, including liver function tests (LFTs) and tumor markers like CA 19-9 and CEA, may indicate cholangiocarcinoma. Biopsy through ERCP or percutaneous techniques confirms the diagnosis.
What are the risk factors for cholangiocarcinoma?
Major risk factors include primary sclerosing cholangitis (PSC), bile duct stones, liver fluke infections (Opisthorchis viverrini, Clonorchis sinensis), chronic hepatitis B and C, cirrhosis, diabetes, obesity, smoking, alcohol use, and exposure to industrial toxins like dioxins and nitrosamines.
What is the role of CA 19-9 in cholangiocarcinoma?
CA 19-9 is a tumor marker used in the diagnosis and monitoring of cholangiocarcinoma. Elevated levels suggest malignancy but are not specific, as they can also be seen in benign biliary diseases like cholangitis or
pancreatitis. Serial measurements help assess treatment response and disease progression.
Can cholangiocarcinoma be detected early?
Early detection is challenging because symptoms appear late. High-risk individuals, such as those with PSC, should undergo regular imaging and CA 19-9 monitoring. Advanced imaging like MRI/MRCP and endoscopic ultrasound (EUS) can help with early detection in at-risk populations.
How is cholangiocarcinoma treated?
Treatment depends on the stage and location. Surgical resection is the best option for localized disease. Unresectable or metastatic cases are managed with chemotherapy (gemcitabine, cisplatin), targeted therapy (FGFR and IDH1 inhibitors), immunotherapy, and palliative procedures like biliary stenting to relieve obstruction.
What is the prognosis for cholangiocarcinoma?
Prognosis depends on the stage at diagnosis. Patients with resectable tumors have a 5-year survival rate of 20–40%. Advanced or metastatic cases have poor outcomes, with median survival of less than a year. Early detection and aggressive treatment improve survival chances.
What role does liver transplantation play in cholangiocarcinoma?
Liver transplantation is an option for unresectable hilar cholangiocarcinoma in highly selected cases. The Mayo Clinic protocol, involving neoadjuvant chemoradiation followed by transplantation, has shown promising outcomes, with 5-year survival rates exceeding 50% in well-selected patients.
Can cholangiocarcinoma be prevented?
Prevention strategies include avoiding known risk factors: treating chronic hepatitis B/C, managing bile duct diseases, preventing liver fluke infections (through proper cooking of fish), quitting smoking, limiting alcohol intake, and controlling obesity and diabetes. Regular monitoring in high-risk patients can aid early detection.
What is the role of targeted therapy in cholangiocarcinoma?
Targeted therapies like FGFR inhibitors and IDH1 inhibitors are effective in patients with specific mutations. They offer personalized treatment options for advanced cases that do not respond to chemotherapy, improving survival rates and quality of life.
How does cholangiocarcinoma spread?
Cholangiocarcinoma spreads through the direct invasion of the liver, lymphatic system, peritoneum, and bloodstream. Metastasis often occurs in regional lymph nodes, lungs, bones, and the peritoneal cavity, complicating treatment. The late-stage disease is often diagnosed due to distant spread.
What is the role of palliative care in cholangiocarcinoma?
Palliative care focuses on symptom management in advanced cholangiocarcinoma. Biliary stents relieve jaundice, pain management improves comfort, and nutritional support helps maintain strength. Palliative chemotherapy or radiation may slow disease progression and improve the quality of life.
How does cholangiocarcinoma affect liver function?
Biliary obstruction leads to cholestasis, causing jaundice, pruritus, and liver dysfunction. Progressive disease can cause hepatic failure, ascites, and coagulopathy. Liver function tests often show elevated bilirubin, alkaline phosphatase, and gamma-glutamyl transferase (GGT), indicating bile duct involvement.
What are the latest advancements in cholangiocarcinoma treatment?
Recent advancements include immunotherapy (checkpoint inhibitors like pembrolizumab), precision medicine using next-generation sequencing for targeted therapy, and novel drug combinations. Ongoing clinical trials are exploring new agents like NTRK inhibitors and radioembolization for improved outcomes.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868