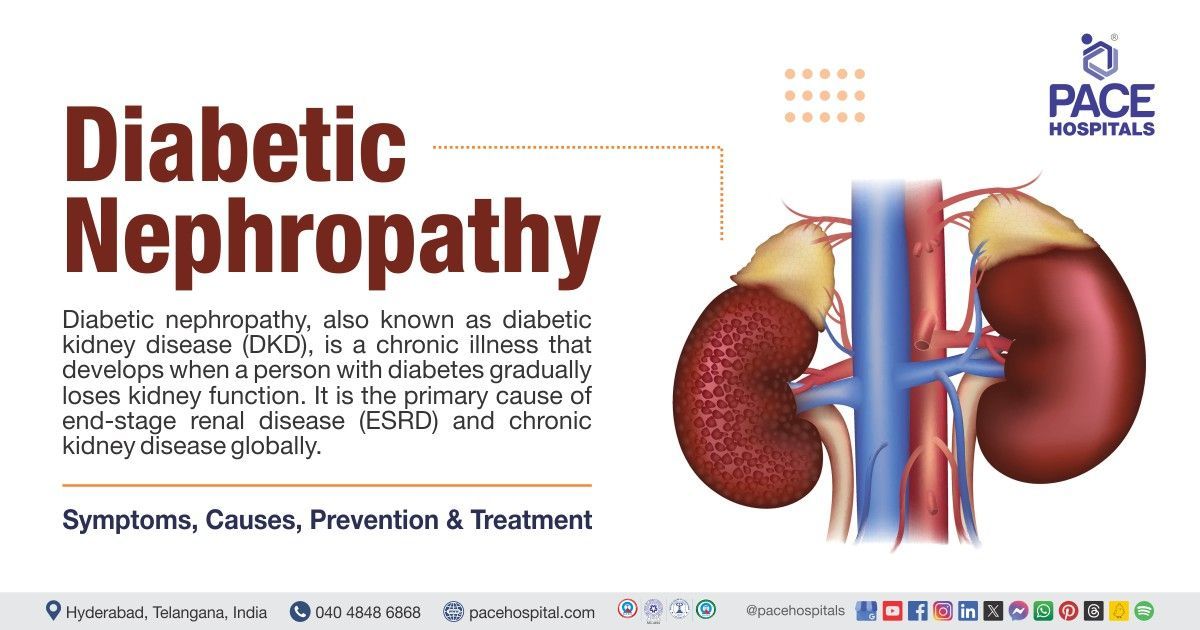
Diabetic Nephropathy - Symptoms, Causes, Complications, Treatment & Prevention
Diabetic nephropathy (DN), also known as diabetic kidney disease (DKD) is one of the most hazardous diabetic chronic microvascular (involving tiny blood vessels) complications, as well as the leading cause of end-stage renal disease (ESRD). The conventional manifestation of diabetic nephropathy is characterized by hyperfiltration (increased glomerular filtration rate) and albuminuria (presence of albumin in urine) in the early stages, followed by gradual kidney function deterioration.
The appearance of diabetic kidney disease (DKD) might vary, particularly in patients with type 2 diabetes, where the presence of additional glomerular/tubular pathologies and severe peripheral vascular disease (a cardiovascular disorder where blood flow to the limbs is decreased due to constricted blood vessels) can be significant factors.
Individuals with diabetic kidney disease have a death rate nearly 30 times greater than diabetic patients without nephropathy, and the vast majority of patients with diabetic kidney disease (DKD) will die from cardiovascular disease before reaching end-stage renal disease (ESRD). Management of metabolic and hemodynamic disturbances is critical for preventing and delaying the progression of diabetic nephropathy. Diabetic kidney disease is a global concern that imposes a large social and economic burden.
Diabetic nephropathy definition
Diabetic nephropathy, commonly known as diabetic kidney disease, is a degenerative kidney disorder that affects people with diabetes. It is distinguished by damage to the small blood vessels of the kidneys, which, if left untreated, can result in diminished kidney function and, finally, renal failure.
Diabetic nephropathy meaning
Diabetic nephropathy is the combination of three words in which
- ‘Diabetic’ is used to describe ‘of or pertaining to diabetes’
- ‘Nephro’ is derived from Greek word ‘nephros’ which means ‘kidney, kidneys’
- ‘Pathy’ is derived from Greek word ‘patheia’ which is used to describe ‘act of suffering, feeling’
Prevalence of diabetic nephropathy
It is demonstrated that about half of individuals with type 2 diabetes and one-third of those with type 1 diabetes will eventually develop diabetic kidney damage. Specifically, due to the drastic increase in cases of type 2 diabetes mellitus, the incidence and prevalence of diabetes mellitus have sharply increased worldwide.
Diabetes affected 53.7 crore people globally in 2021 (eleven percent of the world's population), and by 2045, that figure is predicted to rise to 78.3 crore people (which is 12% of global population). Increased consumption of processed foods decreased physical activity, and a rise in sedentary behaviour have been linked to the obesity pandemic, which has resulted in an increasing burden of type 2 diabetes mellitus. The so-called western way of life is associated with increased urbanisation and technological advancement on a worldwide scale. Diabetic kidney disease (DKD), which is characterised as chronic kidney disease in a diabetic individual, is one of the most common and serious long-term complications of diabetes.
Patients with type 2 diabetes mellitus eventually develop diabetic kidney disease in about 20–50% of cases. Diabetic kidney disease is the primary cause of end-stage kidney disease and chronic renal disease in almost 50% of cases of diabetic kidney disease worldwide. Moreover, diabetic kidney disease lowers the quality of life that patients have in relation to their health and is associated with increased cardiovascular morbidity and death.
Prevalence of diabetic nephropathy in India
A research study found that 34.4% of Indians have diabetic kidney disease (DKD). A composite prevalence of diabetic-chronic kidney disease of about 62.3% was discovered in another multicentre investigation. According to a 2011 research study, 31% of cases of chronic kidney disease (CKD) in India were caused by diabetic nephropathy.
Diabetic nephropathy symptoms
Early diabetic nephropathy frequently occurs without symptoms. As kidney function declines, symptoms may include:
- Swollen hands, feet, and face
- Unable to sleep or concentrate
- Loss of appetite
- Nausea
- Weakness
- Itching at end stage kidney disease
- Extremely dry skin
- Drowsiness (Strong desire to sleep and feelings of sleepiness)
- Abnormalities in the regular heartbeat
- Muscle twitching (unintentional contraction and relaxation of muscles)
As kidney disease worsens, the kidneys find it difficult to eliminate waste from the circulation. The waste accumulates in the body and can reach toxic amounts - a condition known as uraemia. People with uraemia are frequently disoriented and even fall unconscious.
Causes of diabetic nephropathy
Diabetic nephropathy is a complication caused due to diabetes mellitus (type1 and type 2). Long term diabetes can cause damage to the body's tiny blood vessels. Sustained damage to the blood vessels that are present in the kidneys can lead to inadequate blood filtration that can be characterized by ankle swelling and weight gain due to bodily retention of more salt and water. Proteins may also leak into the urine in patients with diabetic nephropathy.
Diabetes has the potential to harm body's nerves which may make it difficult to urinate. A full bladder can cause pressure that builds up and damages the kidneys. High blood pressure is a common side effect of diabetes that can harm the kidneys.
Risk factors for diabetic nephropathy
Various risk factors may influence the onset and progression of diabetic nephropathy, which can be classified into two categories, modifiable and non-modifiable risk factors. Understanding these risk factors is essential for effective prevention and management strategies aimed to preserve kidney health in individuals with diabetes.
Non-modifiable risk factors for diabetic nephropathy
- Duration of diabetes: The longer a person has diabetes, the higher the risk of developing diabetic nephropathy. Patients with diabetes for over 10 years are at significantly increased risk.
- Age: Advanced age is associated with a higher likelihood of diabetic nephropathy, independent of diabetes duration.
- Genetic predisposition: Family history and certain genetic markers have been linked to an increased risk of diabetic nephropathy. Ethnic background also plays a role, with higher incidences observed in African American population.
- Gender: Some studies suggest that female sex may be associated with a reduced risk of progression to severe diabetic nephropathy compared to males.
Modifiable risk factors for diabetic nephropathy
- Poor glycemic control: Elevated blood glucose levels are a primary risk factor. Maintaining optimal glycemic control is crucial to prevent kidney damage.
- Hypertension : High blood pressure significantly increases the risk of diabetic nephropathy. Effective management of blood pressure can help reduce the risk of progression from mild to severe kidney disease.
- Dyslipidemia: Abnormal lipid levels, particularly high levels of low-density lipoprotein (LDL) cholesterol and triglycerides, are associated with an increased risk of nephropathy. Lowering these lipid levels through lifestyle changes or medication can mitigate this risk.
- Obesity: Excess body weight, especially abdominal obesity, is linked to a higher incidence of diabetic nephropathy. Weight loss can improve kidney function and reduce urinary albumin excretion.
- Smoking: Tobacco use has been shown to worsen kidney function and increase albuminuria in individuals with diabetes.
- Physical inactivity: A sedentary lifestyle contributes to obesity and poor metabolic control, thereby increasing the risk of kidney disease.
Understanding these risk factors is essential for early detection and management strategies aimed to prevent or delay the onset of diabetic nephropathy in individuals with diabetes. Regular monitoring and lifestyle modifications can significantly impact outcomes for those at risk.
Diabetic nephropathy complications
Complications from diabetic kidney disease are more likely as the condition gets worse. Some of the examples include:
- Cardiovascular disease (heart disease and/or stroke)
- Hypertension (high blood pressure)
- Anaemia (reduced haemoglobin or red blood cells level in the body)
- Metabolic acidosis (accumulation of acid in the blood)
- Mineral and bone disorder (when an imbalance between the blood levels of calcium and phosphorus causes heart disease or fractures)
- Hyperkalaemia (elevated levels of potassium in the blood)
- Kidney failure
- Diabetes-related kidney disease can be exacerbated or caused by a number of diseases, including high blood pressure and cardiovascular illness.
Diabetic nephropathy diagnosis
Diagnosis of diabetic nephropathy is initially established by:
- Chronic albuminuria (>300 mg/d or >200 μg/min)
- A continuous decrease in the rate of glomerular filtration (GFR)
- Increased blood pressure in the arteries
Besides the above-mentioned diagnostic indicators, diagnostic tests may include:
- Urinalysis
- Blood tests
- Serum and Urinary Electrophoresis
- Renal Ultrasonography
- Renal Biopsy
Diabetic nephropathy treatment
Management of diabetic nephropathy
In the medical treatment of patients with diabetic nephropathy, several factors are crucial. These include lowering salt intake in the diet, controlling hypertension, and, in more severe cases, limiting potassium and phosphorus in the diet.
The following medications are used to regulate blood sugar levels in diabetic patients with renal disease:
- Dipeptidyl peptidase inhibitors
- Alpha-glucosidase inhibitors
- Sodium-glucose cotransporter 2 (SGLT2) inhibitors
- Glucagonlike peptide-1 (GLP-1) receptor agonists or incretin mimetics
- Amylin analogues
- Non-steroidal selective mineralocorticoid receptor (MR) antagonist
In case of a complication such as high blood pressure due to diabetes is treated by using medications such as:
- ACE inhibitors
- Angiotensin receptor blockers (ARBs)
These medications are effective especially in tackling the progression of diabetic kidney disease.
Treatment for end stage renal disease (ESRD) may require:
- Dialysis-at initial stage
Kidney transplantation
Renal replacement therapy may be necessary if end-stage renal disease is diagnosed with a GFR of 10–15 ml/min or lower.
Diabetic nephropathy prevention
Diabetic kidney disease (DKD) can be prevented or slowed down by addressing recognised risk factors along with the preventive strategies such as:
- Glycaemic control (maintaining optimum blood sugar levels): Preventing diabetic nephropathy requires maintaining an acceptable levels of glucose in the blood. According to several studies’ microalbuminuria, which is an early indicator of kidney damage can be prevented by maintaining strict glycaemic control. In addition to delaying the development of diabetic nephropathy strict glycaemic management can also lower the risk of end-stage renal disease.
- Blood pressure control: One more crucial step in preventing diabetic nephropathy is blood pressure control. Lowering blood pressure can inhibit the onset of microalbuminuria and delay the development of diabetic nephropathy. A blood pressure goal of less than 130/80 mm Hg is advised for those with diabetes by the American Diabetes Association.
- Lipid management: To avoid diabetic nephropathy, lipid control is also essential. Diabetes-related kidney damage can be more likely in those with elevated cholesterol and triglyceride levels. It has been demonstrated that people with type 2 diabetes who use statins, a class of lipid-lowering drugs, have a decreased risk of albuminuria.
- Smoking cessation: Smoking is one established risk factor for diabetic nephropathy. Giving up smoking can delay the onset of diabetic nephropathy and lower the incidence of microalbuminuria.
- Regular monitoring: To avoid diabetic nephropathy, kidney function must be regularly monitored. Diabetic nephropathy can be stopped or slowed down in its progression with early kidney damage detection and therapy. The American Diabetes Association advises individuals with type 1 diabetes and those with type 2 diabetes who have had the disease for longer than five years to undergo annual screening for microalbuminuria.
- Lifestyle modifications: Diabetes-related nephropathy can also be avoided by adopting lifestyle changes like consistent exercise, a balanced diet, and weight control. Research has demonstrated that physical activity can enhance kidney function and lower the likelihood of renal damage in individuals with diabetes. Blood pressure and cholesterol levels can be managed with a nutritious diet reduced in salt and saturated fat.
- Medications: Diabetes-related nephropathy is said to be managed with medications such as angiotensin receptor blockers and angiotensin-converting enzyme inhibitors. These drugs can reduce the risk of end-stage renal disease, lessen proteinuria, and decrease the development of diabetic nephropathy.
- Education and awareness: The prevention of diabetic nephropathy is mostly depends on education and awareness. Diabetes patients need to be made aware of the significance of blood pressure, cholesterol, and glucose control. They should also understand the significance of routinely assessing kidney function and the risk factors associated with diabetic nephropathy.
Differences between diabetic nephropathy and hypertensive nephrosclerosis
Diabetic nephropathy vs hypertensive nephrosclerosis
| Aspect | Diabetic Nephropathy (DN) | Hypertensive Nephrosclerosis (HN) |
|---|---|---|
| Meaning | Kidney damage due to longterm diabetes mellitus | A degenerative kidney disease due to poorly managed high blood pressure (hypertension). |
| Pathogenesis and Risk Factors | Associated with diabetes (type 1 or 2) | Linked to chronic hypertension |
| Histological Features | Diabetic glomerulosclerosis (Kimmelstiel-Wilson lesions) and tubulointerstitial involvement | Vascular, glomerular, and tubulointerstitial changes, vascular disease in renal arteries and arterioles |
| Clinical Presentation | Proteinuria, hypertension, progressive renal decline | Hypertension (less prominent proteinuria) |
| Prognosis | Poor prognosis, especially in advanced stages | Variable outcomes based on eGFR, proteinuria, and other factors |
Frequently Asked Questions (FAQs) on Diabetic nephropathy
What are the biomarkers of diabetic nephropathy?
At the moment, the gold standard markers for identifying and tracking diabetic kidney disease are albuminuria and eGFR. These two indicators, however, are not very good at identifying diabetic kidney disease in its early stages.
Can diabetic nephropathy be cured?
End-stage renal illness results in irreversible kidney damage, making dialysis or a kidney transplant necessary for survival. The usual therapies for diabetic patients include lowering cholesterol, preventing the renin-angiotensin system, and monitoring blood sugar and vital signs.
Can diabetic nephropathy cause death?
Yes. Indeed, diabetic nephropathy can be fatal. Diabetic nephropathy is a progressive disease that can lead to end-stage renal disease and eventually kidney failure, the two conditions that kills people most frequently. Diabetic nephropathy may potentially result in the need for dialysis or a kidney transplant, as well as an increased risk of cardiovascular disorders.
What is the life expectancy of a diabetic with kidney disease?
For individuals with type 1 diabetes mellitus with nephropathy, end stage renal disease (ESRD) is the leading cause of death, accounting for 59–66% of deaths. Less than 10% of the older type 2 diabetes mellitus population and no more than 40% of the younger type 1 diabetes mellitus group survived for five years in prospective research study.
What is the first sign of diabetic nephropathy?
Patients are frequently asymptomatic when the disease initially starts off, and screening results show creatinine levels ranging from 30 to 300 mg/g. Once nephropathy sets in patients may have tiredness, frothy urine (urine protein more than 3.5 g per day), and pedal oedema (swollen feet).
What is diabetic nephropathy?
Diabetic nephropathy is a significant consequence of both type 1 and 2 diabetes. It's also known as diabetic kidney disease.Diabetic nephropathy impairs the kidneys' normal function of eliminating waste materials and excess fluid from the body. The best strategy to prevent or delay diabetic nephropathy is to maintain a healthy lifestyle and control diabetes and high blood pressure levels.
What is kimmelstiel wilson disease?
Diabetic nephropathy, commonly referred to as Kimmelstiel-Wilson disease. It is so called because, Paul Kimmelstein- a pathologist and Clifford Wilson- a
nephrologist originally reported regarding the lesions in diabetic kidney disease which are then named as Kimmelstiel-Wilson lesions in the year 1936.
What is kimmelstiel wilson lesion?
Mutations in polycystin 1 and polycystin 2 proteins can affect the function of renal cilia, which allow tubular cells to perceive flow rates. A prominent concept suggests that flow rate influences tubular cell proliferation and differentiation, and thus ciliary failure may result in cyst transformation.
What is the pathophysiology of diabetic kidney disease?
A number of pathophysiological mechanisms, including microvascular and macrovascular alterations, are involved in this complicated condition- diabetic kidney disease (DKD). Increased glomerular filtration, decreased albuminuria, or both may result from these modifications.
Do all diabetics get kidney damage?
Diabetes can damage the kidneys over time. This may result in renal failure. Even though many patients with diabetes do not have renal issues in the end.
What is the new treatment for diabetic kidney disease?
A 2024 study has demonstrated that other novel medications, such as GLP1 receptor agonists, incretin mimetics, and nonsteroidal MRAs, are advantageous for diabetic patients. These novel medications can slow the advancement of diabetic kidney disease and enhance blood sugar regulation.
What are diabetic nephropathy stages?
Studies conducted over the years divide the diabetic kidney disease into five stages
- Stage 1: Marked by hypertrophy (increased organ volume) and early hyperfunction (excessive function)
- Stage 2: Stage 2 is marked by morphologic abnormalities that do not exhibit any clinical symptoms and develops silently over several years.
- Stage 3: Stage 3, or incipient diabetic nephropathy, is characterised by excessively high urine albumin excretion as determined by radioimmunoassay.
- Stage 4: Overt diabetic nephropathy, or stage 4, is a well-known condition marked by ongoing proteinuria (more than 0.5 g/24 hours).
- Stage 5: Stage 5 of diabetic nephropathy is end-stage renal failure accompanied by uraemia (a disorder characterised by excessively elevated waste product levels in the blood, primarily urea and creatinine).
How long does diabetes take to damage kidneys?
Diabetes-related kidney damage can start 5–15 years after diagnosis, although more severe kidney disease can take 10–30 years to develop.
What diet one should eat having diabetic kidney disease?
A healthy diet for diabetes appears to be like any other healthy diet. People with diabetic kidney disease are recommended to Consume a diet rich in fruits, vegetables, lean protein, and healthy fats and reduce the intake of processed carbohydrates, sugar, and salt.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Hafeezpet, Madeenaguda, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc).

CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
FOLLOW US
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital near me.