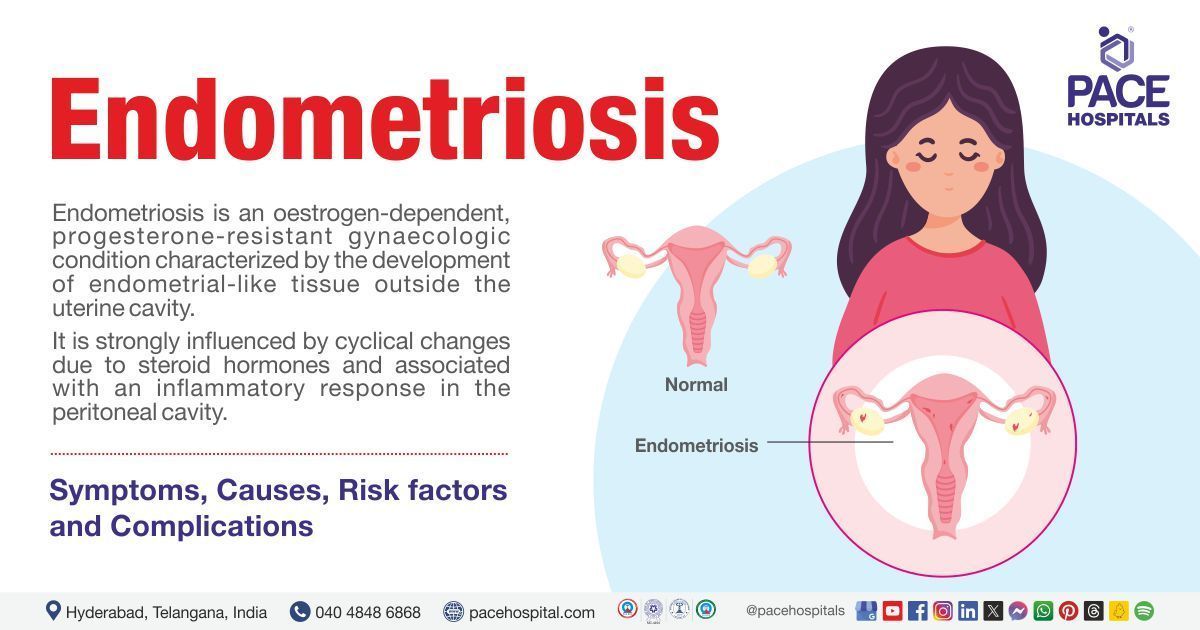
Endometriosis - Types, Symptoms, Risk factors, Causes and treatment
Endometriosis definition
Endometriosis is a chronic inflammatory gynaecologic condition characterized by the presence of endometrial (tissue similar to the lining of the uterus-like) tissue grows outside of the uterus and on other regions of the body where it doesn’t belong, which is associated with painful symptoms.
This condition may have a significant effect on the fertility of the female, and many patients with undiagnosed endometriosis may be first presented to the gynaecologist with the symptoms of difficulty in conceiving.
Endometriosis growths are not cancerous (benign). However, they may continue to expand and cause specific issues, such as inflammation, blocking the fallopian tubes when these growths cover the ovaries, forming scar tissue and adhesions leading to pelvic pain, and making it hard for the patient to get pregnant and problems in the intestines and bladder.
Endometriosis meaning
Endometriosis is a word derived from the Greek word “endo,” which means “inside or within,” “metra,” which means “uterus,” and osis means “state of disease.” Commonly, most of the endometriosis is found on the:
- Ovaries
- Fallopian tubes
- Tissues that hold the uterus in place
- The outer surface of the uterus
Other sites for endometrial growths may include:
- Vagina
- Vulva
- Cervix
- Bowel
- Bladder or rectum
Rarely, endometriosis may appear in
- Lungs
- Brain
- skin
Endometriosis prevalence in worldwide
Approximately 10 in every 100 women of reproductive age are affected by endometriosis. It is caused due to a combination of several genetic and environmental factors, which infers 24.7 crore girls and women globally.
It is estimated that endometriosis affects approximately 10-15% of women of reproductive age, as many as half of all women with decreased fertility, and 70-90% of women who are suffering from chronic pelvic pain. Surprisingly, endometriosis may be possible in males taking high doses of oestrogen, which is extremely rare.
Endometriosis prevalence in India
In the Indian population, various studies have shown the incidence of endometriosis to range from 34% to 48% as diagnosed by laparoscopy. A recent study found out that there are about 4.2 crore females in India. The significant incidence of endometriosis is thought to be in women aged 25-35 years. However, this condition is less common in younger females and post-menopausal women.
Types of endometriosis
Endometriosis is characterised by the presence of endometrium (the inner lining of your uterus) such as tissue and lesions (stroma) outside the endometrium and myometrium (the muscular outer layer of the uterus) and is usually with an associated inflammatory process.
Most endometriosis is found inside the abdominal cavity and exists in three subtypes. The following are the three types of endometriosis:
- Superficial peritoneal endometriosis (pelvic endometriosis): Endometrial-like tissue develops along the lining of the abdominal cavity, which accounts for around 80% of endometriosis.
- Ovarian endometriosis: These are cystic masses (abnormal growths or fluid-filled sacs) caused by the development of the endometrial tissue inside the ovary containing dark bloodstained fluid (chocolate cysts). These are also called endometriosis ovarian cysts or “endometriomas.”
- Deep infiltrating endometriosis: A severe form of endometriosis where the lesions penetrate deeper than 5mm below the peritoneal surface (membrane lining the abdominal cavity) found in the recto-vaginal septum, bladder and bowel).
Some of the other types of endometriosis include:
- Extra-abdominal endometriosis: Endometrium-like tissue outside the abdominal cavity (for example, thoracic, umbilical, brain endometriosis)
- Iatrogenic endometriosis: Direct or indirect dissemination (spreading) of endometrium tissue following surgery (for example, caesarean scar endometriosis).
Endometriosis symptoms
Signs and symptoms of endometriosis may not be the same for all women and usually be cyclic and worsen at the time of menstruation because these endometriotic lesions are hormonally responsive. During anovulation periods, such as menopause, pregnancy, lactation, and hormone-induced amenorrhoea (not having regular periods), symptoms are usually reduced or eliminated.
- Endometriosis pain: It is the most common symptom in most women. The kind and intensity of endometriosis pain depends on endometriosis pain location. These include:
- Endometriosis ovulation pain: Very painful menstrual cramps: This type of pain may get worse over time.
- Endometriosis pelvic pain: Chronic pain in the pelvis area and lower back.
- Endometriosis pain during intercourse: It may describe as “deep” pain, which is not the same as the pain that a woman feels at the entrance of the vagina when penetration starts. It can also be seen after intercourse in some cases.
- Endometriosis abdominal pain: it is also called endometriosis intestinal pain.
- Endometriosis and bowel pain: Pain or painful bowel movements when the patient is urinating during menstrual periods.
- Endometriosis vaginal bleeding or spotting: It may see in between the menstruation cycle that is caused by something other than endometriosis. In rare cases, patients may also find blood in urine or stool.
- Endometriosis heavy periods: The patient may have to use lots of pads or tampons, or the patient may bleed through the clothes.
- Endometriosis infertility: The main clinical symptoms of the disease are chronic pelvic pain and impaired fertility. It is significantly more common in patients with endometriosis, with a doubling of risk compared with women without endometriosis.
- Endometriosis and stomach problems: Endometriosis women may experience more abdominal pain, constipation, bloating, and flatulence, especially during menstrual periods.
- Silent endometriosis: Some women with endometriosis may not have any symptoms (asymptomatic endometriosis). They are usually surfaced upon examining any unexplained infertility.
Endometriosis causes
The cause of endometriosis is not known and not well understood. However, it is estimated that retrograde menstruation is the common pathogenesis of endometriosis which accounts for about 90% of women.
- Retrograde menstruation: During each menstrual period, most of the blood and uterine lining are shed through the woman's cervix and into the vagina. However, for some women, some of this tissue enters the pelvis through the fallopian tubes instead of the vagina. One common theory is that women develop endometriosis simply due to the inability to clear these cells from the pelvis.
When retrograde menstruation occurs, internal bleeding and inflammation can lead to fibrosis (scar formation) and adhesion development, which in turn contributes to the development of symptoms and physical distortion of pelvic anatomy (changes in normal shape, structure, and positioning of organs) that is seen in patients with more severe endometriosis.
The following factors may influence whether lesions and implants that persist in the pelvic cavity.
- Genetic factors: Endometriosis runs in families. Hence, some people may have a high chance of developing endometriosis if they have a family history of this condition.
- Immune system issues: In some people, a (faulty) immune system may fail to detect and destroy endometrial tissue growing outside of the uterus, leading to endometriosis. Certain cancers and immune system disorders are more common in women with endometriosis.
- Hormones: The high level of oestrogen appears to promote endometriosis and the treatment mainly deals in the reduction of the same.
- Surgery: For instance, endometrial tissue has been found in abdominal scars. It is possible during surgery on the abdominal area, such as a hysterectomy or caesarean (C-section), the endometrial tissue of the patient could be picked up and moved by mistake.
Risk factors for developing endometriosis
Although the cause of endometriosis remains unclear, some environmental and genetic factors are considered endometriosis risk factors for its manifestation and progression. Several factors have been associated with the risk of developing endometriosis, including as follows:
- Early age at menarche (age below 11 years old): If the woman starts menstruation at a young age, usually before age 11, this may increase the risk of developing endometriosis due to more years of menstrual cycles in the woman's reproductive life.
- Shorter duration of menstrual periods (less than 27 days): The menstrual cycle length is not the same for all women and varies greatly from woman to woman (ranging from 21 to 35 days). The length of the menstrual cycle shorter than or equal to 27 days (SEQ27) raises the risk of endometriosis, and the length LEQ29 decreases the risk.
- Nulliparity (state of never being pregnant yet): As per the researchers, it was found that there is a twofold increased risk of endometriosis among nulliparous women, which might be linked with the early use of oral contraceptive pills (OCPs) (nulligravida endometriosis).
- Family history of endometriosis: If a woman's family has endometriosis, there is an increased risk of developing endometriosis.
- Hormonal status of the woman: When the hormones become unbalanced in women (high oestrogen levels and low progesterone), the body may increase the risk of developing oestrogen-dominant conditions such as endometriosis.
- Müllerian anomalies: Mullerian anomalies refer to abnormal anatomy that arises during the formation of female reproductive organs.
- Outflow obstructions: Outflow obstructions, such as a transverse vaginal septum, cervical stenosis, or an imperforate hymen, may cause this condition.
Factors decreasing the risk of endometriosis
Research revealed that there are protective factors that act by decreasing the levels of oestrogen in the body or lowering the inflammatory process. The following are the protective factors that reduce the risk of endometriosis:
- Parity, protracted breastfeeding: Prolonged breastfeeding seems to suppress the development of endometriosis by causing postpartum amenorrhea (delay of menstruation after childbirth) but also with other mechanisms.
- Tubal ligation: Tubal ligation (a permanent form of contraceptive in which a fallopian tube of a woman is tied or blocked) is thought to be one of the protective factors because it decreases the chance of endometriosis by blocking the menstrual blood flow to reach the pelvic cavity.
- Current oral contraceptive use: Contraceptive use and parity (number of times a woman has given birth) may interfere with the occurrence of ovulation. Whenever ovulation occurs, it triggers inflammation and the release of specific cytokines in the body. These cytokines enhance cell growth and oxidative stress, increasing the production of substances that cause further discomfort and inflammation.
- Other factors: Additionally, primary amenorrhea (not having regular periods), being physically active, and other dietary and lifestyle habits such as increased intake of omega-3 fatty acids and smoking are linked with decreased risk of endometriosis. Surprisingly, smoking is associated with a reduced risk of endometriosis, where commonly, it has harmful effects on other health issues.
- Early adult body mass index (BMI): Early adult BMI is inversely proportional to endometriosis.
Endometriosis complications
Studies demonstrated a risk of obstetrical complications (increased risk of placental complications) among women suffering from endometriosis. This could lead to an increased risk of obstetrical haemorrhage during labour as well as in pregnancy. A detailed list of complications which may be experienced by women with endometriosis include:
Fertility problems (endometriosis and pregnancy)
- The main problem with endometriosis could arguably be the difficulty in the patient to get pregnant (subfertility) or not being able to get pregnant at all (infertility).
- While endometriosis medication may not improve the fertility, there are cases of fertility promotion with surgery. Surgery may improve fertility by removing the endometriosis tissue.
- However, surgery is not guaranteed to allow the patient to get pregnant.
- All women with endometriosis may not face this problem, and some women will eventually be able to conceive without any treatment.
- If the patient is having difficulty getting pregnant, infertility treatments such as in vitro fertilization could be an option.
Adhesions and ovarian cysts
- Some women with endometriosis may develop adhesions (sticky areas of endometriosis tissue that can fuse organs together), and endometriomas (fluid-filled cysts in the ovaries) can sometimes become very large and painful.
- They may occur if the endometriosis tissue is on or near the ovaries (endometriosis ovarian cyst).
- These adhesions and ovarian cysts can be treated with surgery, but they may revert in the future if the patient gets endometriosis again.
Endometriosis diagnosis
Diagnosis of endometriosis might be challenging, as some studies show a delay in diagnosis by 4–10 years, resulting in disease progression and reduced quality of life. Therefore, timely diagnosis and initiation of management of endometriosis is vital in reducing painful symptoms, improving quality of life, and managing fertility. The common diagnostic tests include:
- Pelvic exam: Endometriosis pelvic examination may be used to feel the large cysts or scars behind the uterus.
- Endometriosis ultrasound: Gynaecologists may recommend ultrasound (endometriosis usg) to picture the reproductive organs and check for ovarian cysts from endometriosis.
- Magnetic resonance imaging (MRI): Pelvic MRI endometriosis is another common imaging test that can make an imaging of the inside of the body.
- Endometriosis medication: If the gynaecologist does not find signs of an ovarian cyst during an ultrasound, some hormonal medications may be recommended to check whether the pain is getting better or not to diagnose endometriosis.
- Laparoscopy endometriosis: It is a minimally invasive surgery (uses small incisions) used to look inside the pelvic area to see endometriosis tissue.
- Endometriosis biopsy test: In the endometrial biopsy test, a small tissue sample is extracted from the lining of the uterus (endometrium) which will be sent to the pathologist department for study. The pathologist then observes the endometrial tissue under a microscope to see if any abnormal cells are developed.
Endometriosis treatment
Endometriosis can be treated symptomatically with contemporary medicines and devices as the cure for endometriosis is yet to be discovered. The treatment of endometriosis depends on the patient’s decision to get or not get pregnancy.
- If the patient opts to be pregnant, then endometriosis drugs such as hormonal contraceptive are usually the first step of treatment. This may include:
- Extended-cycle or continuous contraceptives: These are available in the form of pills and help to reduce pain or to stop bleeding.
- Intrauterine device (IUD): It protects against pregnancy for up to 7 years. IUD helps reduce pain and bleeding. However, it may not be effective if the endometriosis occurs for a long time.
- If the patient opts not to be pregnant, endometriosis medication such as GnRH agonists may be prescribed by the gynaecologist. These medicines help stop the woman's body from secreting specific hormones responsible for ovulation, the menstrual cycle, and the growth of endometriosis.
- Endometriosis surgery: Endometriosis laparoscopic surgery may be recommended if the patient has severe symptoms, when hormones are not providing relief, or if the patient is having fertility issues.
- Surgery will be performed either to cut away patches of endometriosis tissue or to remove part or all of the organs affected by endometriosis. Other treatments are also recommended alone or with any of the following treatments:
- Endometriosis pain treatment: Over-the-counter medicines may be suggested to treat mild symptoms such as mild pain etc.
Endometriosis prevention
It is neither possible to prevent endometriosis; nor there is a cure for it. However, the symptoms of this condition may be treated with medications or surgery (in some cases).
Nevertheless, one can decrease the probability of developing it by lowering the oestrogen hormone levels in the body. Oestrogen in women helps to thicken the endometrium (lining of the uterus) during the menstruation cycle.
To keep lower oestrogen levels or to decrease the levels of oestrogen, one can follow some precautions, such as:
- Exercise regularly: Regularly exercising for more than 4 hours a week may help them keep a low percentage of body fat. Lower amounts of body fat and regular exercise help reduce the amount of oestrogen in the body.
- Avoid large amounts of alcohol: Alcohol increases oestrogen levels, which increases the risk of endometriosis.
- Avoid large amounts of caffeine: Some studies showed that drinking more than one caffeinated drink daily, particularly sodas and green tea, may raise oestrogen levels.
Additionally, primary amenorrhea (failure of menses to occur by age 16 years), other dietary and lifestyle habits such as increased intake of omega-3 fatty acids, and other factors such as prolonged breastfeeding and tubal ligation are associated with a decreased risk for endometriosis.
Difference between endometriosis and adenomyosis
Adenomyosis vs endometriosis
Endometriosis and adenomyosis are similar but separate conditions which may happen together. Although these are similar, they have some differences, which include:
| Elements | Adenomyosis | Endometriosis |
|---|---|---|
| Definition | It is a gynaecologic condition that causes endometrial tissue in the endometrium (lining of the uterus) to grow into (myometrium) muscular wall of the uterus | Endometriosis is a chronic inflammatory gynaecologic condition, characterised by the presence of endometrial (tissue similar to the lining of the uterus-like tissue grows outside of the uterus and on other regions of the body where it doesn’t belong |
| Location | Mainly grows into the wall of the uterus (within the uterus) | It may grow on the fallopian tubes, ovaries, vagina or intestines (outside the uterus) |
| Commonly leads | Enlargement of the uterus and may lead to heavy menstrual bleeding | Pelvic pain and infertility |
| Causes | Age, childbirth and previous surgeries, | Retrograde menstruation, hormonal abnormalities, genetics |
| Symptoms | Feeling of abdominal bloating, fullness or heaviness, enlarged uterus, pelvic pain, severe cramps during periods, heavy or prolonged menstrual bleeding | Pelvic pain, pain during sex, getting difficulty to conceive, vaginal bleeding or spotting |
| Complications | Shortness of breath, anemia from heavy bleeding, fatigue | Infertility, adenomyosis or ovarian cyst |
Difference between endometrioma and endometriosis
Endometrioma vs endometriosis
Endometrioma is one of the common forms of endometriosis, where both appear as similar conditions. Although these are similar, they have some differences, which includes:
| Elements | Endometrioma | Endometriosis |
|---|---|---|
| Definition | Endometriomas are the cystic lesions (abnormal growths or fluid filled sacs) that arise from the disease process of endometriosis. | Endometriosis is a chronic inflammatory gynaecologic condition, characterised by the presence of endometrial (tissue similar to the lining of the uterus like tissue grows outside of the uterus and on other regions of the body where it doesn’t belong |
| Location | Ovaries | Fallopian tubes, ovaries, vagina or intestines (outside the uterus) |
| Symptoms | Pain during sex, feeling urge to pee more, back pain, painful periods | Pelvic pain, pain during sex, getting difficulty to conceive, vaginal bleeding or spotting |
| Appearance | Filled with dark brown endometrial fluid (chocolate cysts) | Stromas or scar tissue (implants first look like small, flat patches, blebs, or flecks sprinkled on the surface of the pelvic organs or the lining of the pelvis, appearing clear, white, brown, red, black, or blue |
Difference between Endometritis vs Endometriosis
Endometritis vs Endometriosis
Endometritis and endometriosis are two different conditions. Endometritis is caused by a bacterial infection within the uterus, whereas endometriosis is never caused by an infection. Although these are not similar, both conditions affect the uterus. The following are the differences between endometritis and endometriosis:
| Elements | Endometritis | Endometriosis |
|---|---|---|
| Definition | It is an infection or inflammation of the inner lining of the uterus (endometrium). | It is a chronic inflammatory gynaecologic condition characterized by the presence of endometrial (tissue similar to the lining of the uterus-like) tissue grows outside of the uterus and on other regions of the body where it doesn’t belong, which is associated with painful symptoms. |
| Spreading | Bacteria from the cervix and vagina can ascend upwards and lead to inflammation and infection of the endometrium. | Endometriosis may occur other organs including the bladder, bowel, ovaries, fallopian tubes, and rarely in lungs, brain and skin. |
| Cause | It can be caused due to certain organisms such as chlamydia and gonorrhoea or mix of normal vaginal bacteria. | The cause of endometriosis is not known and not well understood. However, it is estimated that retrograde menstruation is the common pathogenesis of endometriosis which accounts for about 90% of women. Other causes includes genetic factors, hormonal irregularities, immune system issues. |
| Symptoms | Symptoms may include swelling of the abdomen, vaginal bleeding or discharge, discomfort with bowel movement (including constipation), fever, pain in the lower abdomen or pelvic region, and general discomfort, uneasiness, or ill feeling. | Signs and symptoms of endometriosis may not be the same for all women and usually be cyclic and worsen at the time of menstruation because these endometriotic lesions are hormonally responsive. Pelvic pain, vaginal bleeding or spotting, heavy periods and infertility are the common symptoms in endometriosis. |
| Treatment | Treatment includes antibiotics to treat the infection and prevent complications, other treatment includes fluids through a vein (by IV), rest. | Treatment of endometriosis includes hormonal treatments, pain medications. Sometimes surgery also needed for some patients. |
| Complications | Possible complications may include infertility, septicaemia, septic shock, pelvic or uterine abscess formation, pelvic peritonitis (generalized pelvic infection). | Complications of endometriosis include adhesions, ovarian cysts and fertility problems. |
| Prognosis | Prognosis of endometritis is good with prompt treatment | Prognosis may require long-term management. |
Uterine fibroids vs Endometriosis
Uterine fibroids and endometriosis are chronic gynaecologic conditions that affect the female reproductive system, such as pelvic and abdominal areas, but they take different forms. The following are the common differences between them:
| Elements | Uterine fibroids | Endometriosis |
|---|---|---|
| What is it | Non-cancerous growths made of muscle and tissue that form in or on the uterus | Endometrium like tissue grows outside of the uterus |
| Causes | There is no clear explanation about exactly what causes fibroids. They are thought to be caused by genes (they may run in families) and hormones in the body | Retrograde menstruation (main cause), genetic factors, immune system problems, hormonal irregularities. |
| Symptoms | Heavy bleeding, the feeling of fullness in the pelvic area, frequent urination, pain during sex, and lower back pain. Complications during pregnancy and labour, and reproductive problems. | Infertility, chronic pain, vaginal bleeding and spotting in between menstrual periods, painful menstruation, and heavy periods. |
| Complications | Although most fibroids are harmless, they can cause complications, including heavy bleeding, anaemia, and reproductive problems. | Complications of endometriosis include adhesions, ovarian cysts and fertility problems. |
| Treatment | Treatment options include over-the-counter drugs to reduce mild pain, iron supplements if the patient is having heavy bleeding, birth control treatments, and oral therapies. Depending on the condition, surgery (myomectomy) may be recommended in some people. | Treatment of endometriosis includes hormonal treatments, pain medications. Sometimes surgery also needed for some patients. |
Difference between Endometriosis pain vs kidney stone pain
Endometriosis pain vs kidney stone pain
Endometriosis pain and kidney stone pain are not similar, and both are different in the following ways:
| Elements | Endometriosis pain | Kidney stone pain |
|---|---|---|
| Character | Muscle spasm (stabbing pain), pain occurs during sex, during periods, urinating or bowel movements | Sharp, cramping pain |
| Radiation | It often leads to back pain and radiating leg pain | Often radiates to the lower abdomen or groin |
| Trigger | Cyclic pain that is progressive overtime especially during menstrual periods. | Severe pain that starts and stops suddenly, when the stones move down the tubes through which urine empties into bladder |
| Associated symptoms | Infertility, fatigue, nausea, depression and anxiety | Fever, blood in the urine, abnormal urine colour, nausea and vomiting |
| Duration | Chronic pain, may last for long time | Pain may last until stone passes |
PCOS vs Endometriosis
Polycystic ovarian syndrome (PCOS) and endometriosis are gynaecologic disorders, but both are completely different conditions where the differences between them may include as follows:
| Elements | Polycystic ovarian syndrome | Endometriosis |
|---|---|---|
| Definition | It describes the multiple small cysts (fluid-filled sacs) that form in the ovaries. | It is a chronic inflammatory gynaecologic condition characterized by the presence of endometrial (tissue similar to the lining of the uterus-like) tissue grows outside of the uterus and on other regions of the body where it doesn’t belong, which is associated with painful symptoms. |
| Causes | The exact cause of PCOS is not clear and not fully understood and may be associated with family history, genetics, poor lifestyle, and hormonal irregularities. | The cause of endometriosis is not known and not well understood. However, it is estimated that retrograde menstruation is the common pathogenesis of endometriosis which accounts for about 90% of women. Other causes includes genetic factors, hormonal irregularities, immune system issues. |
| Symptoms | Common symptoms of PCOS include weight gain, missed periods, irregular periods, light periods or no periods at all, excessive hair growth, difficulty getting pregnant, and oily skin or acne. | Signs and symptoms of endometriosis may not be the same for all women and usually be cyclic and worsen at the time of menstruation because these endometriotic lesions are hormonally responsive. Pelvic pain, vaginal bleeding or spotting, heavy periods and infertility are the common symptoms in endometriosis. |
| Complications | Patients with this condition have a high risk of developing certain health issues such as infertility, high blood pressure, type 2 diabetes, and problems with the heart and blood vessels. | Complications of endometriosis include adhesions, ovarian cysts and fertility problems. |
| Treatment | There is no cure for the polycystic ovarian syndrome, but some treatments can improve symptoms. The possible treatment options include birth control pills, diabetic medications, and lifestyle modifications (changes in diet and physical activity). | Treatment of endometriosis includes hormonal treatments, pain medications. Sometimes surgery also needed for some patients. |
FAQs - Frequently asked questions on Endometriosis
Is endometriosis dangerous?
Endometriosis is not life-threatening; however, if it is not treated over time, it can cause cysts, adhesions, and scar tissue, leading to long-term (chronic) pain, especially during menstrual periods and infertility. It may impact the quality of life by causing serious complications such as ovarian cysts or adhesions and mental health issues such as depression.
What are the first signs of endometriosis?
The primary signs and symptoms of endometriosis may include pelvic pain, especially during periods, painful sex, and infertility. Other symptoms of this condition include vaginal bleeding, fatigue, and depression; however, symptoms of endometriosis are non-specific and may overlap with other diseases, such as irritable bowel syndrome (IBS) and pelvic inflammatory disease (PID), making diagnosis challenging.
Can endometriosis cause cancer?
No, endometriosis cannot cause cancer, and the disease itself is not a cancer. However, endometriosis is associated with an increased risk of developing epithelial ovarian cancer (EOC), but many women with endometriosis never develop ovarian cancer. Therefore, early identification and management of this condition may help to decrease the risks that are associated with it.
Can I get pregnant with endometriosis?
Yes, one can become pregnant with endometriosis. Most women with endometriosis may have a normal pregnancy. However, many women with endometriosis can have a difficult time getting pregnant because this condition is a common cause of infertility. Medical help and extra monitoring will be recommended because, during pregnancy, endometriosis can improve, but it often returns later and may cause problems becoming pregnant again.
How do you heal endometriosis naturally?
There is no way to heal or cure endometriosis. However, enhanced awareness followed by early identification (diagnosis) and management may slow the natural progression of endometriosis and reduce the long-term burden of painful symptoms. Lifestyle changes and natural remedies may help manage this condition and can influence oestrogen levels, inflammation, and menstrual cycle regularity.
Is endometriosis a disease?
Yes, endometriosis is a disease in which tissue similar to the endometrium (the lining of the uterus that grows outside the uterus) is present. This leads to inflammation and formation of scar tissue (adhesions, fibrosis) forming in the pelvic region and rarely at other parts of the body. It can start at a woman's first menstrual period and last until the menopause.
What happens if endometriosis is left untreated?
If endometriosis is left untreated, it may cause serious complications such as infertility, reduced fertility, and adhesions or ovarian cysts. It may cause pain during urination, painful sex, chronic inflammation, and depression. However, these effects may depend on the severity and duration of the endometriosis and how long it remains untreated.
When does endometriosis develop?
Endometriosis can develop at any age, including teenagers, young women, and women who have had children. According to some specialists, endometriosis is more likely to be found in those who have never been pregnant. It's a long-term (chronic) condition that can have a significant impact on a woman's quality of life.
How do I know if I have endometriosis?
If the person is experiencing symptoms such as pelvic pain, vaginal bleeding, severe menstrual cramps, painful sex, or getting difficult to pregnant, these symptoms may indicate endometriosis. However, symptoms of endometriosis are non-specific and may overlap with other diseases, such as irritable bowel syndrome (IBS) and pelvic inflammatory disease (PID). Hence, it is recommended that one consult a gynaecologist if one may experience the symptoms mentioned above.
Is scar endometriosis dangerous?
Scar endometriosis is an uncommon (rare) condition and is challenging to diagnose. It may not be life-threatening; however, it may result in delayed or misdiagnosis and cause emotional and physical distress to the patient.
Can I have endometriosis after menopause?
Although rare, endometriosis after menopause could be a possibility. Endometriosis is an oestrogen dependant inflammatory condition; in a menopausal woman with a history of endometriosis, a drop in levels of oestrogen after menopause relieves the endometriosis-related symptoms but generates certain menopausal ones such as hot flushes, mood swings, etc.
Can endometriosis cause irritable bowel syndrome?
There is no evidence that endometriosis can cause irritable bowel syndrome (IBS). However, women diagnosed with endometriosis have a two to three-fold increased risk of irritable bowel syndrome compared to women without endometriosis. Although they are two different conditions with distinct causes, many women experience both conditions simultaneously.
Does endometriosis affect implantation in IVF?
Yes, endometriosis may affect implantation in in-vitro fertilization (IVF). Some studies found that women who have endometriosis have significantly lower pregnancy rates (lower chance of getting pregnant) after in-vitro fertilization and embryo transfer as compared to women without endometriosis due to endocrine abnormalities (hormonal imbalances), immune and inflammatory disorders, and fibrosis (tissue scarring).
How to prevent endometriosis pain?
It is not possible to prevent symptoms if the patient has endometriosis, but they can be managed. To manage endometriosis pain, healthcare professionals will give pain medications, simple analgesics, and hormonal treatments. Physiotherapists may develop some programs such as exercises and relaxation techniques designed to reduce pain, help strengthen pelvic floor muscles, and manage stress and anxiety.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Hafeezpet, Madeenaguda, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc).

CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
FOLLOW US
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital near me.