Gastroesophageal Reflux Disease (GERD) - Symptoms, Causes, Diagnosis & Treatment
PACE Hospitals
GERD Definition
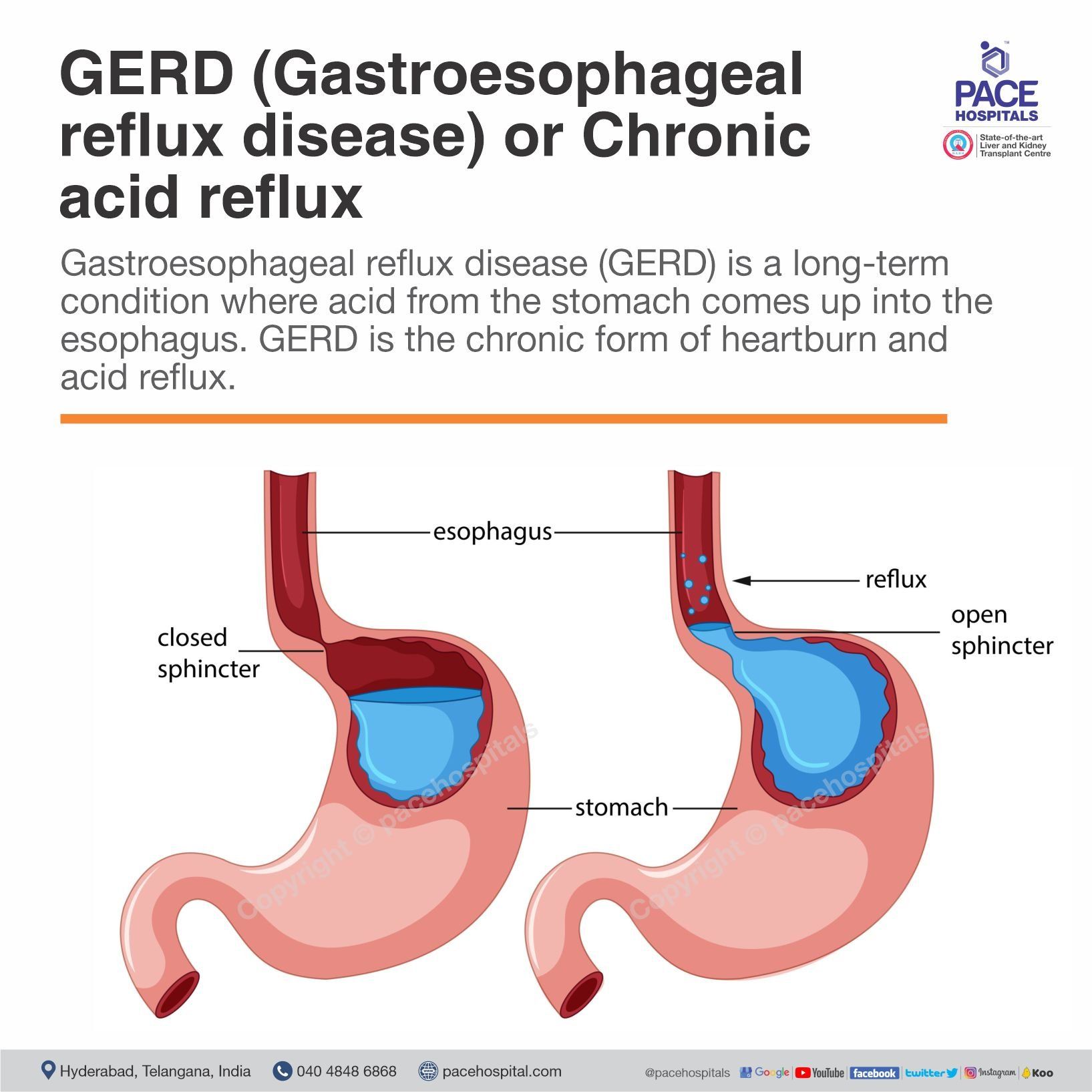
Gastroesophageal reflux disease (GERD) or chronic acid reflux is a long-term condition where acid from the stomach comes up into the esophagus, a muscular tube connecting the stomach with the throat (pharynx). Flowing back up acid into the esophagus causes irritation to the esophagus lining. Common symptoms include heartburn (a burning sensation behind the sternum), acid regurgitation (sour or burning fluid in the throat or mouth), chest pain, dysphagia (difficulty swallowing), nausea, bloating, and sore throat.
The causes of GERD involve factors that impair lower esophageal sphincter (LES) function or increase abdominal pressure, such as obesity, pregnancy, hiatal hernia, smoking, certain medications, and unhealthy lifestyle habits. If untreated, GERD can lead to serious complications, including esophagitis, esophageal strictures, Barrett's esophagus, gastrointestinal bleeding, and increased risk of esophageal adenocarcinoma.
A gastroenterologist, a physician specialised in digestive system disorders, can accurately diagnose and provide the correct treatment for GERD.
GERD is the chronic form of heartburn and acid reflux. If you have symptoms of acid reflux more than twice a week, you might have a condition known as gastroesophageal reflux disease (GERD).
GERD Meaning
The term “Gastroesophageal reflux disease” (GERD) is derived from Greek and Latin roots:
- “Gastro-” meaning “stomach”.
- “Esophageal” meaning “food pipe”—the tube that carries food from the mouth to the stomach.
- “Reflux” means to “flow back “or “to return”.
- “Disease”- A medical term for a chronic or long-term condition.
Thus, GERD means the disease that causes backward flow (reflux) of stomach contents into the esophagus.
GERD Epidemiology
GERD Epidemiology Worldwide
GERD presents a significant and growing global public health burden, with its prevalence and incidence rising steadily over recent decades. The global prevalence of GERD was estimated at over 8,250 lakh cases. This increase is caused by several factors, such as an ageing global population, higher obesity rates, and changes toward more Western diets and lifestyles. The epidemiology of GERD acid reflux shows significant geographic variations, with higher prevalence rates traditionally seen in Western countries compared to East Asia.
GERD Epidemiology in India
In India, the epidemiology of GERD has seen a significant increase in prevalence, with recent studies showing a pooled rate of approximately 15.6%. Once considered less common than in Western nations, the prevalence is now recognised as similar or even higher in some areas, especially in urban settings. Some southern India studies report rates as high as 22.2%, while northern regions show 16.2% among certain hospital staff. The rise is mainly due to lifestyle changes that are linked to socioeconomic growth and Western habits.
Types of GERD
Gastroesophageal reflux disease (GERD) can be categorised by the presence or absence of physical damage to the esophagus, and by the location of the reflux. The GERD classification is as follows:
- Based on esophageal damage
- Non-erosive reflux disease (NERD)
- Erosive reflux disease (ERD)
- Based on the location of reflux
- Gastroesophageal reflux disease (GERD)
- Laryngopharyngeal reflux (LPR)
- Extraesophageal reflux disorder (EERD)
- Based on severity and progression
- Silent GERD (asymptomatic GERD)
- Mild GERD
- Moderate GERD
- Severe GERD
- Refractory GERD
Non-erosive reflux disease (NERD)
NERD is a form of GERD in which patients experience reflux symptoms such as heartburn and regurgitation but do not show visible damage to the esophageal lining upon endoscopic examination. The absence of mucosal erosion does not indicate that the condition is minor; rather, symptoms develop as a result of acid exposure, esophageal hypersensitivity, or functional abnormalities.
Erosive reflux disease (ERD)
Erosive reflux disease (ERD) occurs when reflux of acidic stomach contents leads to visible mucosal injury or inflammation in the esophagus. These ulcers or erosion can be seen during an upper gastrointestinal (GI) endoscopy. ERD is a more advanced stage of GERD than NERD, which is linked to severe symptoms and a higher risk of complications such as esophagitis, bleeding, strictures, or Barrett’s esophagus.
Gastroesophageal reflux disease (GERD)
The classic form of GERD involves the reflux of stomach contents primarily into the esophagus, the tube that connects the throat and stomach. Symptoms are felt in the chest and include heartburn and regurgitation.
Laryngopharyngeal reflux (LPR)
LPR is a subtype of reflux where the refluxate travels beyond the esophagus and reaches the throat (pharynx) and voice box (larynx). Common symptoms include hoarseness, sore throat, severe cough, throat clearing, and a sensation of a lump in the throat. It is often managed jointly by gastroenterologists and ear, nose, and throat (ENT) specialists.
Extraesophageal reflux disorder (EERD)
EERD refers to reflux that affects organs and tissues outside the esophagus, such as the respiratory tract, mouth, and sinuses. The refluxed material causes asthma-like symptoms, chronic bronchitis, dental erosions, sinusitis, or even otitis media in children. EERD reflects the systemic impact of reflux and highlights that GERD can influence multiple organ systems beyond the digestive tract.
Silent GERD
Silent GERD,is refers to the presence of esophageal mucosal injury without any noticeable reflux symptoms. It is often discovered incidentally during endoscopic evaluation for other conditions. Despite the absence of symptoms, silent GERD is clinically significant because it can still lead to complications such as Barrett’s esophagus or esophageal adenocarcinoma if left untreated.
Mild GERD
Mild GERD represents an early stage of the disease, which is characterised by infrequent and mild symptoms, generally occurring less than twice per week. There is minimal or no visible esophageal injury, and complications are rare at this stage. Mild GERD can be managed with lifestyle changes and over-the-counter medications.
Moderate GERD
In moderate GERD, symptoms happen more often and can be quite bothersome, usually appearing several times a week. Patients may have a lower quality of life, experience disturbed sleep, or show mild esophagitis during an endoscopy. At this point, it’s important to keep a close eye on the condition to avoid worsening it.
Severe GERD
Severe GERD is characterised by persistent, intense symptoms that can impair daily life and often indicate advanced esophageal damage such as severe esophagitis or ulceration. Patients may have complications like strictures or Barrett’s esophagus.
Refractory GERD
Refractory GERD refers to cases where symptoms continue even after the best medical treatment. This usually happens after at least 8 weeks of high-dose PPI therapy. This type of GERD may be caused by non-acid reflux, bile reflux, esophageal hypersensitivity, or a misdiagnosis.

GERD Symptoms
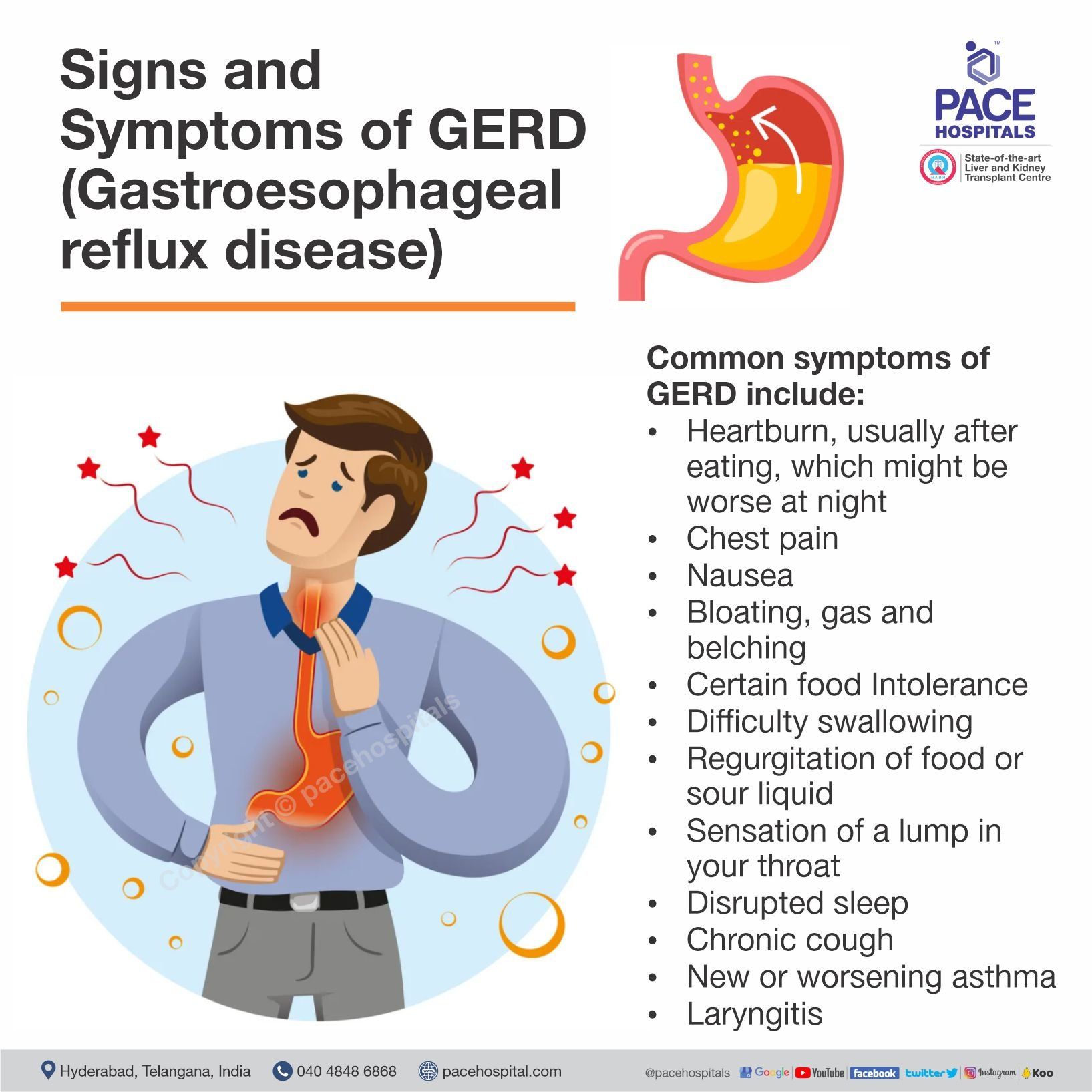
GERD is curable disease, but most of the time people don't know they are suffering from Gastroesophageal reflux disease because its symptoms are associated with many other conditions.
Common symptoms of GERD include:
- Heartburn, usually after eating, which might be worse at night
- Chest pain
- Nausea
- Bloating, gas and belching
- Certain food Intolerance
- Difficulty swallowing
- Regurgitation of food or sour liquid
- Sensation of a lump in your throat
If acid reflux occur during nighttime, one can experience:
- Disrupted sleep
- Chronic cough
- New or worsening asthma
- Laryngitis
Heartburn: This is the most common symptom of GERD, which can be described as a burning sensation in the chest or throat that often appears after eating or when lying down. It happens because the lower esophageal sphincter fails to close properly, allowing acidic stomach contents to flow back into the esophagus. The acid irritates the sensitive esophageal lining, leading to the characteristic burning pain.
Chest pain: Chest pain in GERD occurs due to acid-induced inflammation of the esophageal wall or spasms of the esophageal muscles. The pain can mimic heart-related (angina) pain, but unlike cardiac pain, GERD-related discomfort is often related to meals and may improve with antacids.
Nausea: Nausea results from irritation of the stomach and esophagus caused by refluxed acid. Persistent reflux can slow gastric emptying, leading to a feeling of queasiness (the feeling of wanting to vomit). In some people, severe reflux episodes may even trigger vomiting. Nausea is often more noticeable after eating large or fatty meals, when the stomach is full and pressure increases.
Bloating, gas, and belching: These symptoms occur because GERD affects normal digestion and allows swallowed air to accumulate in the stomach and esophagus. When acid refluxes, it can increase swallowing frequency as a reflex response, leading to more air intake (aerophagia). The excess air causes bloating and pressure in the upper abdomen, prompting frequent belching or burping as the body tries to release the gas.
Certain food intolerance: For some people with GERD, particular foods may trigger or worsen their symptoms, leading to a perceived intolerance. Foods like spicy, fatty, or acidic foods, as well as coffee and alcohol, can relax the LES or increase stomach acid production, causing more severe reflux.
Difficulty swallowing (dysphagia): Difficulty swallowing occurs when chronic acid exposure causes inflammation, scarring, or narrowing (stricture) of the esophagus. Repeated irritation leads to thickening and reduced elasticity of the esophageal wall, making it harder for food to pass smoothly.
Regurgitation of food or sour liquid: Regurgitation is the effortless backflow of stomach contents into the throat or mouth. This happens when the LES becomes weak or opens abnormally, allowing partially digested food and acid to rise upward. Patients often experience a sour or bitter taste, especially when bending forward or lying down.
Sensation of a lump in the throat: Many GERD patients describe feeling as though a lump or foreign body is stuck in the throat. This “globus” sensation is caused by acid reaching the upper esophagus or throat, leading to muscle tightness and inflammation in the laryngopharyngeal area.
Disrupted sleep: GERD often worsens at night, especially when lying flat, because gravity no longer helps keep stomach contents in place. When acid refluxes into the esophagus during sleep, it can cause burning pain (heartburn), chest discomfort, coughing, or choking sensations that repeatedly awaken the person.
Chronic cough: Stomach acid reflux irritates the esophagus and throat, triggering the cough reflex. Sometimes small amounts of acid are inhaled, further irritating the airways. This cough often worsens after meals or at night. New or worsening asthma: Acid reflux can irritate the airways or trigger nerve reflexes that cause bronchoconstriction, leading to coughing, wheezing, and shortness of breath. GERD can make asthma harder to control, and asthma can, in turn, worsen reflux.
Laryngitis: When acid reaches the throat, it inflames the vocal cords, causing hoarseness, sore throat, frequent throat clearing, or loss of voice. This form of reflux, known as laryngopharyngeal reflux (LPR), often occurs without typical heartburn.
Generally many people have acid reflux symptoms every now and then, especially after eating large meals or lying down right after a meal. If acid reflux occur at least twice per week then it can be classified as GERD (Gastroesophageal reflux disease) sometimes symptoms become moderate to severe. In case of the persistent symptoms, consult a gastroenterologist.
GERD Causes
Gastroesophageal reflux disease (GERD) or chronic acid reflux caused by frequently happening acid reflux. The major cause of GERD is a malfunctioning LES. When the LES weakens or relaxes abnormally, stomach acid and contents flow back into the esophagus, creating discomfort and reflux symptoms. Several factors can contribute to this dysfunction:
- Weak or Incompetent lower esophageal sphincter (LES)
- Hiatal hernia
- Esophageal motility disorders
- Impaired mucosal defence
Weak or Incompetent lower esophageal sphincter (LES): Acid reflux happens when your LES doesn’t tighten or close properly. This allows digestive juices and other contents from your stomach to rise up into your esophagus.
The lower esophageal sphincter (LES) is a circular band of muscle at the end of your esophagus. When it’s working properly, it relaxes and opens when you swallow. Then it tightens and closes again afterwards.
Hiatal hernia: When part of the stomach pushes up through the diaphragm, it weakens the support of the lower esophageal sphincter (LES). This allows stomach acid to flow back more easily into the esophagus, causing reflux.
Esophageal motility disorders: Impaired esophageal muscle movement or weak peristalsis prevents proper clearance of acid from the esophagus, allowing acid to linger longer and cause irritation.
Impaired mucosal defence: The esophageal lining may become more sensitive or less able to resist acid injury, contributing to inflammation and discomfort even with minor reflux episodes.
GERD Risk Factors
The risk factors for GERD include several conditions and lifestyle elements that increase the likelihood of acid reflux and impairment of the esophageal barrier. These conditions that can increase risk of GERD:
- Overweight or Obesity
- Hiatal hernia
- Pregnancy
- Age
- Gender
- Lifestyle factors
- Use of certain drugs
- Anxiety and depression
- Delayed gastric emptying
- Lack of physical activity
- Scleroderma or CREST syndrome
Overweight or Obesity: Obesity is one of the strongest and most well-documented risk factors for GERD. Excess fat, particularly abdominal (visceral) fat, increases intra-abdominal pressure, which pushes against the stomach. This pressure overcomes the lower esophageal sphincter (LES), the valve that normally prevents reflux, allowing stomach acid to move upward into the esophagus.
Hiatal hernia: Bulging of the top of the stomach up into the diaphragm and the chest cavity. The diaphragm normally provides support to the LES by maintaining pressure at the junction between the stomach and esophagus. When this anatomy is altered, the LES becomes weakened or displaced into a low-pressure chest environment, making it unable to close properly.
Pregnancy: Pregnancy leads to GERD by hormonal and physical mechanisms. Increased amounts of hormones relax smooth muscles, particularly the LES. Meanwhile, the growing uterus increases intra-abdominal pressure, especially in the third trimester, compressing the stomach and promoting reflux.
Age: Advancing age leads to physiological changes that make reflux more likely. The LES naturally weakens, esophageal clearance slows, and peristaltic function declines with age. Additionally, older adults are more prone to hiatal hernia and delayed gastric emptying, both of which increase acid reflux.
Gender: While GERD affects both men and women, studies shows some gender-based differences. Men tend to have a higher prevalence of erosive GERD and Barrett’s esophagus, while women more often experience NERD and reflux symptoms during pregnancy or menopause due to hormonal changes.
Lifestyle factors: Unhealthy lifestyle play a major role in triggering reflux. Eating large meals, lying down after eating, or eating late at night increases the likelihood of acid reflux because the stomach is full and gravity no longer helps keep acid down. Smoking weakens the LES and reduces saliva production, which normally helps neutralise acid. Alcohol relaxes the LES and irritates the lining of the esophagus. Triggered food (fatty foods or fried foods) can stimulate acid production and slow down gastric emptying. Over time, these habits cause chronic reflux and inflammation of the esophagus.
Use of certain drugs: Many commonly used medications can increase GERD risk by relaxing the LES or irritating the esophagus. These include calcium channel blockers, vasodilators, bronchodilator, sedatives, anticholinergics, tricyclic antidepressants, and nonsteroidal anti-inflammatory drugs (NSAIDs). Some of these drugs lower LES pressure, while others delay gastric emptying or damage the mucosal barrier. When used long-term, they can significantly worsen or trigger reflux symptoms.
Anxiety and depression: Emotional stress, anxiety, and depression effects gut-brain interaction and autonomic nervous system function. They can increase gastric acid secretion, slow gastric emptying, and heighten esophageal sensitivity to acid, making symptoms feel more intense. Additionally, anxiety can cause muscle tension and poor eating habits that worsen reflux.
Delayed gastric emptying: Delayed gastric emptying (gastroparesis) occurs when the stomach takes longer time to empty into the small intestine. This causes prolonged gastric distension and increased pressure in the stomach, pushing contents upward through the LES. Conditions like diabetes or certain medications can slow gastric emptying. The result is more frequent and severe reflux episodes.
Lack of physical activity: A sedentary lifestyles slow digestion and contributes to weight gain, both of which increase reflux risk. Regular moderate exercise helps improve gastric motility and reduce GERD symptoms.
Scleroderma or CREST Syndrome: In scleroderma, especially CREST syndrome, the muscles of the esophagus become stiff and weak due to fibrosis. This weakening of the LES impairs food movement, allowing stomach acid to flow back easily into the esophagus, leading to chronic GERD.
GERD Complications
In most people, GERD doesn’t cause serious complications. But in case of delayed diagnosis and treatment, GERD can lead to serious or even life-threatening health problems.
- Esophageal stricture (narrowing of the esophagus) - Damage to the lower esophagus from stomach acid causes scar tissue to form. The scar tissue narrows the food pathway, leading to problems with swallowing.
- Esophageal ulcer (an open sore in the esophagus) - Stomach acid can wear away tissue in the esophagus, causing an open sore to form. An esophageal ulcer can bleed, cause pain and make swallowing difficult.
- Barrett's esophagus (precancerous changes to the esophagus) - Damage from acid can cause changes in the tissue lining the lower esophagus. These changes are associated with an increased risk of esophageal cancer.
- Esophageal adenocarcinoma which affects a small portion of people with Barrett’s esophagus.
- Asthma, chronic cough, or other breathing problems, which may develop if you breathe stomach acid into your lungs.
- Dental problems - tooth enamel erosion, gum disease or other dental problems.
GERD Diagnosis
The diagnosis of GERD is generally based on a combination of clinical symptoms, response to treatment, and diagnostic tests to confirm acid reflux and assess esophageal damage. To confirm a diagnosis of GERD, or to check for complications, gastroenterologists use one or more of the following procedures:
- Medical history: Assessment of symptoms, along with lifestyle factors, medications and family history.
- Physical examination: The doctor checks for signs of anemia, weight loss, or abdominal tenderness that might suggest complications.
- Therapeutic trial
- Proton pump inhibitor trial therapy: A short course of PPIs is given to see if symptoms improve.
- Functional diagnostic tests
- Esophageal manometry: A flexible tube is threaded into your esophagus to measure the strength of your esophageal muscles.
- Ambulatory esophageal reflux monitoring: This test measures how often and how long acid refluxes into the esophagus.
- Esophageal pH monitoring: A monitor is inserted into your esophagus to learn if and when stomach acid enters it.
- Esophageal impedance-pH monitoring: This advanced test detects both acidic and non-acidic reflux by measuring changes in electrical resistance (impedance) and pH.
- Endoscopic evaluation
- Upper gastrointestinal (GI) endoscopy: A flexible tube with a tiny camera is threaded into your esophagus to examine it and collect a sample of tissue (biopsy) if needed.
- Imaging studies
- Barium swallow/barium radiograph: Barium solution, and X-rays are taken to visualise the esophagus and stomach.
GERD Treatment
Gastroesophageal reflux disease treatment focuses on relieving symptoms, healing the esophageal lining, preventing complications, and reducing acid reflux. Management includes lifestyle changes, medications, and sometimes surgery, depending on severity.
- Non-pharmacological treatment
- Maintaining a healthy body mass index (BMI)
- Lifestyle and dietary changes
- Elevating the head of the bed
- Patient education
- Pharmacological treatment/ GERD medications
- Proton pump inhibitors (PPIs)
- Histamine-2 receptor antagonists (H2Ras)
- Potassium-competitive acid blockers (P-CABs)
- Antacids
- Prokinetics and GABA-B agonists
- Mucosal protective agents
- Endoscopic therapies
- Magnetic sphincter augmentation
- Transoral incisionless fundoplication (TIF)
- Surgical interventions
- Laparoscopic Nissen fundoplication
- Laparoscopic anterior 180° fundoplication
- Bariatric surgery
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
GERD Prevention
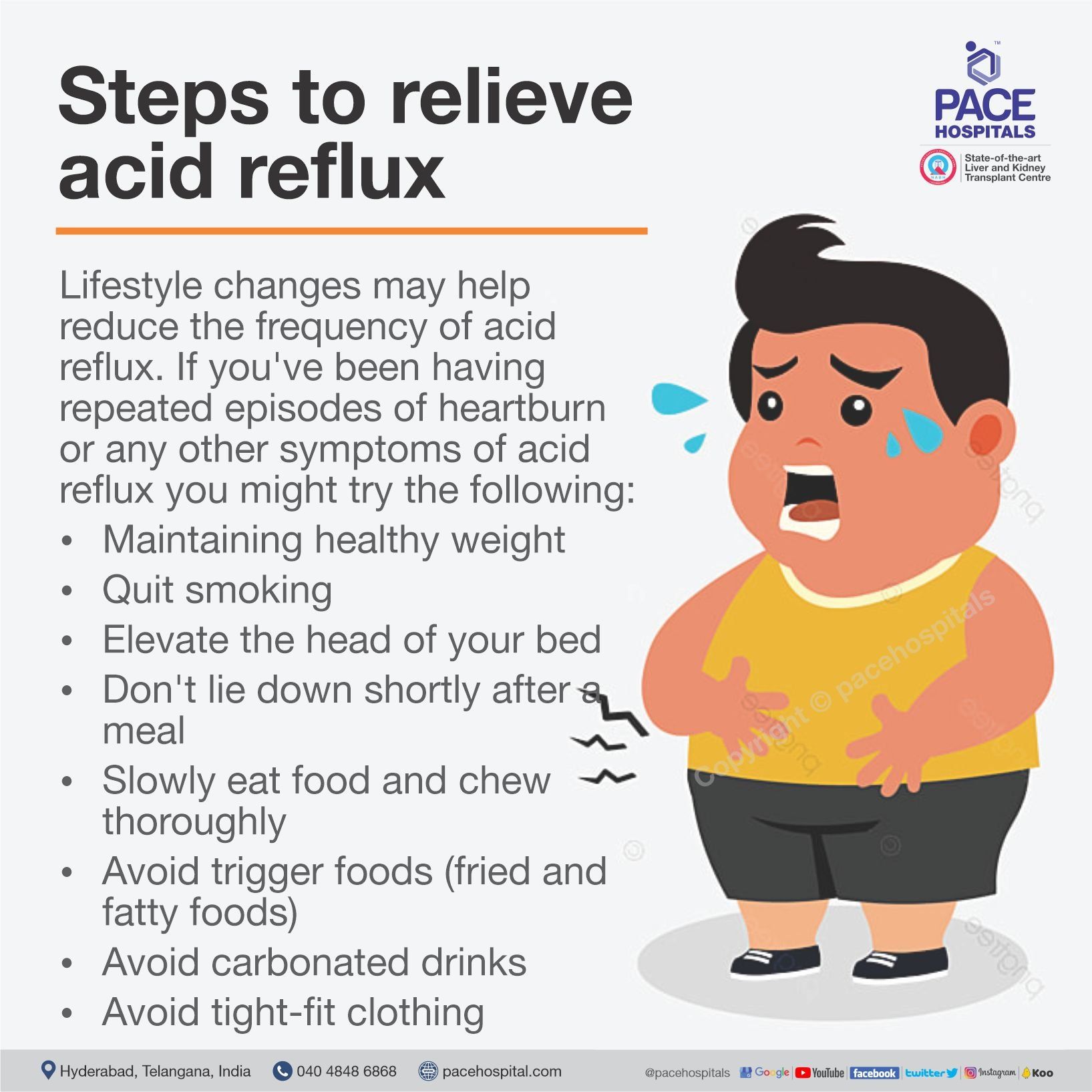
Lifestyle changes may help reduce the frequency of acid reflux. If you've been experiencing frequent episodes of acid reflux, heartburn or any other symptoms of acid reflux, these steps will help in relieving acid reflux:
- Maintaining healthy weight - Excess weight put pressure on your abdomen, pushing up your stomach and causing acid to reflux into your esophagus.
- Quit smoking - Smoking decreases the lower esophageal sphincter's ability to function properly.
- Elevate the head of your bed - If you regularly experience heartburn while trying to sleep, place wood or cement blocks under the feet of your bed so that the head end is raised by 6 to 9 inches. If you can't elevate your bed, you can insert a wedge between your mattress and box spring to elevate your body from the waist up. Raising your head with additional pillows isn't effective.
- Don't lie down shortly after a meal - Wait at least three hours after eating before lying down or going to bed.
- Slowly Eat food and chew thoroughly - Put down your fork after every bite and pick it up again once you have chewed and swallowed that bite.
- Avoid trigger foods and drinks that cause reflux - Common triggers include fatty or fried foods, tomato sauce, alcohol, chocolate, mint, garlic, onion, and caffeine.
- Avoid tight-fit clothing - Clothes that fit tightly around your waist put pressure on your abdomen and the lower esophageal sphincter.
Difference between GERD and Acid Reflux
Both GERD and acid reflux involve the backflow of stomach contents into the esophagus and can cause comparable symptoms, such as heartburn and regurgitation. However, their frequency and clinical implications vary greatly. Differentiating between the two is critical for correct diagnosis and suitable treatment.
GERD vs Acid Reflux
| Parameters | GERD | Acid reflux |
|---|---|---|
| Definition | A chronic condition in which acid reflux is frequent and causes symptoms or harm. | Acid reflux is the occasional backward flow of stomach acid into the esophagus |
| Type | Long-term disease | Symptom or occasional event |
| Frequency | Occurs frequently (≥2 times per week) | Happens rarely or after certain foods/behaviors |
| Symptoms | Frequent heartburn, chest pain, cough, hoarseness, difficulty swallowing | Heartburn, sour taste, regurgitation |
Difference between GERD and Peptic Ulcer Disease
GERD disease and peptic ulcer disease (PUD) are two different conditions that both involve damage from stomach acid, but they affect different parts of the digestive tract. While they share similar symptoms, there are significant distinctions in their underlying causes, site of pain, and potential complications.
GERD vs Peptic Ulcer Disease
| Parameters | Gastroesophageal reflux disease (GERD) | Peptic ulcer disease (PUD) |
|---|---|---|
| Definition | A chronic disorder in which stomach acid often refluxes into the esophagus, producing irritation or inflammation. | A condition in which open sores (ulcers) form in the lining of the stomach or duodenum due to acid damage. |
| Primary site affected | Esophagus | Stomach or duodenum |
| Main cause | Weak or relaxed lower esophageal sphincter (LES), allowing acid reflux | Helicobacter pylori infection or long-term NSAID (painkiller) use |
| Symptoms | Regurgitation, chest pain, sour taste, cough, hoarseness | Nausea, bloating, vomiting, loss of appetite, black stools (if bleeding) |
| Complications | Esophagitis, Barrett's esophagus, esophageal strictures, and esophageal cancer. | Bleeding, perforation, gastric outlet obstruction, and peritonitis |
| Diagnosis | Based on symptoms, endoscopy, and 24-hour pH monitoring | Endoscopy and H. pylori testing (urea breath test, stool antigen, or biopsy) |
| Treatment | Lifestyle changes, proton pump inhibitors (PPIs), and surgery if needed | PPIs, antibiotics for H. pylori eradication, and avoiding NSAIDs |
Frequently asked questions (FAQs) on GERD
Is GERD a lifetime disease?
Yes, gastroesophageal reflux disease (GERD) is a chronic, usually lifelong disease that often may return if the treatment is stopped or discontinued and can progress to major complications.
How to cure GERD permanently?
GERD is usually not considered fully cured, but it can be controlled for long periods. Long-term control relies on lifestyle changes (losing weight, avoiding trigger foods that worse symptoms, not lying down after meals) plus medications (especially proton pump inhibitors) to reduce acid damage. In patients with anatomical problems like large hiatal hernia or where medicines fail, surgery or endoscopic procedures can offer lasting relief.
What to eat with GERD?
A diet for GERD should focus on non-irritating, low-fat, high-fibre foods. Good choices include oatmeal, whole grains, lean proteins (chicken, fish), non-acidic vegetables, bananas, and melons. Low-fat yogurt may be soothing. Avoid spicy, fried, citrus, tomato, chocolate, caffeine, and carbonated drinks, which often worsen symptoms.
Can GERD cause chest pain?
Yes, GERD can cause chest pain that may feel similar to heart-related pain. This pain results from stomach acid irritating the esophagus. It is usually a burning or squeezing sensation behind the breastbone, often after eating or when lying down.
How long does GERD take to heal?
Healing time for GERD varies, but with proper treatment and acid-reducing medications like PPIs, healing of the esophagus can occur within 4 to 8 weeks. Symptoms often improve sooner, but ongoing treatment might be needed to prevent relapse. Without treatment, GERD symptoms and damage can persist or worsen over time.
What is the difference between a hiatal hernia and GERD?
A hiatal hernia and GERD are distinct but often related medical conditions.
- A hiatal hernia is an anatomical issue where part of the stomach bulges out through the diaphragm into the chest cavity. It is a known risk factor for GERD because it impairs the function of the LES.
- GERD is a functional disorder caused by the reflux of stomach contents, while a hiatal hernia is a structural problem that can disrupt the anti-reflux barrier and lead to GERD.
Is GERD infectious?
No, GERD is not an infectious disease. It results from physical problems such as a weak valve between the stomach and esophagus or other body functions affecting acid reflux. GERD cannot spread from person to person because it is not caused by bacteria or viruses. However, infections like Helicobacter pylori can cause other stomach problems, but do not cause GERD itself.
Is curd good for GERD?
Yes, curd or yoghurt can be good for some people with GERD as it is a low-acid dairy product and contains probiotics that may improve digestion. However, tolerance varies; some may find that dairy worsens symptoms. It’s best to try small amounts and see how your body reacts. If curd causes discomfort or increases symptoms, it’s better avoided.
Can GERD cause mouth ulcers?
Yes, studies indicate a link between GERD and mouth ulcers. The reflux of gastric contents, which contain highly acidic substances like stomach acid, pepsin, and bile salts, into the oral cavity can damage the protective mucosal tissues. This acid exposure, which may be exacerbated by reduced salivary flow in some GERD patients, may cause inflammation and lead to the development of oral ulcers.
What is the difference between NERD and GERD?
Non-erosive reflux disease (NERD) is a subtype of GERD, not a distinct disorder. The key difference lies in the presence or absence of visible damage to the esophageal lining. In NERD, patients experience classic GERD symptoms like heartburn, but an endoscopy shows no signs of erosion or injury. NERD accounts for the majority of GERD cases and can be caused by acid, non-acid, or weakly acidic reflux, with symptoms sometimes resulting from a heightened sensitivity to reflux events.
Can GERD cause blood in mucus?
GERD usually does not directly cause blood in mucus. However, severe GERD may lead to irritation, inflammation, or esophageal damage, which can rarely cause bleeding. Blood from the esophagus might sometimes appear in the mucus coughed up. Any presence of blood should be medically evaluated, as it may indicate other causes like infections, injuries, or more serious conditions requiring prompt attention.
Can GERD cause wheezing?
Yes, GERD can cause wheezing by irritating the airways and lungs. Acid reflux sometimes reaches the throat and airway, leading to coughing, wheezing, or worsening asthma symptoms. The acid can cause inflammation and tightening of the air passages, making breathing difficult.
Does exercise reduce GERD?
Exercise can help reduce GERD symptoms by improving digestion and maintaining a healthy body mass index (BMI), which lowers gastric pressure. However, high-impact or strenuous activities, especially those involving straining of the abdominal muscles, can increase intra-abdominal pressure and make reflux symptoms worse. It is recommended to avoid intense exercise right after eating to prevent reflux.
When to consult a doctor for GERD?
Consult a doctor for GERD if there is frequent heartburn, regurgitation, or acid reflux that lasts more than a few weeks, especially if symptoms interfere with sleep or daily life. Signs that indicate a need for medical care are:
- Persistent burning sensation in the chest or throat
- Difficulty or pain while swallowing
- Frequent vomiting or regurgitation of food or sour liquid
- Unexplained weight loss or loss of appetite
- Chronic cough, hoarseness, or sore throat
- Chest pain that occurs after eating or lying down
If these symptoms continue or worsen, it is important to see a GERD doctor for an accurate diagnosis and treatment. Seek emergency medical attention if there is a sign of vomiting of blood, black or tarry stools, or severe chest pain, as these may indicate complications such as esophageal bleeding or ulceration. A general physician or gastroenterologist can provide the right GERD treatment to manage symptoms and reduce long-term risks.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868