Heart Attack (Myocardial Infarction): Types, Symptoms, Causes, Treatment & Prevention
Heart attack definition
A heart attack, medically termed myocardial infarction, is a life-threatening condition that needs emergency help and is caused by the lack of blood flow and oxygen to the portion of the heart muscle (myocardium).
Most heart attacks are often caused by blockages in coronary arteries; these are the blood vessels that supply (carry) oxygen to the myocardium. If the blockage happens to this artery, it can cause a deficit of oxygen in the heart muscle. However, a prolonged shortage of oxygen to the myocardium can lead to cell damage and death. This damage can result in chest pressure or pain, spreading to the jaw, neck, shoulder, or arm.
It may be silent and unnoticed, or it can also be a major event causing a rapid drop in blood flow, which can lead to decreased heart function and sometimes potentially cause sudden death. Noticing the early signs of a heart attack and getting timely treatment is essential and may save a person's life.
Myocardial infarction meaning
"Myocardium" means "heart muscle", and "infarction" means "cram or to plug up," which refers to the clogging of an artery, derived from the Latin word "infarcire."
Prevalence of heart attack
Coronary heart disease (CHD) is the fundamental cause of most deaths of men and women worldwide. The estimated annual deaths have risen from 0.226 crore to 0.477 crore. Cases of CHD may differ between urban and rural areas, ranging from 1.6% to 7.4% in rural areas and 1% to 13.2% in urban areas. Myocardial infarction, accountable for over 15% of annual deaths, is the most common type of CHD. The incidence of MI is higher in men in all age-specific groups than in women.
As per the INTERHEART studies, it was found that smoking 1–5 cigarettes every day has elevated the chances of developing an acute MI by 40%. This risk might be raised with the amount (number) of tobacco smoked per day.

Types of heart attacks
Types of heart attacks can be categorized based on ST segment, a measurement from an Electrocardiogram (ECG), and the level of troponin (heart protein) in the blood. The below-mentioned discusses the different types of heart attacks:
A myocardial infarction is a form of ACS (ACS refers to a range of conditions where the arteries that supply oxygen, nutrients, and blood get blocked) where there is a blockage in the coronary arteries. There are three types of ACS, include:
- ST-segment elevation myocardial infarction (STEMI)
- Non-ST segment elevation myocardial infarction (NSTEMI)
- Unstable angina
ST segment defines the patterns that are visible on an electrocardiogram, which is a display of a person's heartbeat.
- STEMI: It is a type of myocardial Infarction (type of MI) which is also called as classic or massive heart attack that is characterized by a complete blockage of the coronary artery and a prolonged interruption of blood supply, resulting in extensive damage to the heart, mainly affecting the lower chambers. It requires immediate treatment to unblock the artery.
- NSTEMI: It is another type of MI, also called a mini heart attack, which is characterized by partial blockage of the coronary artery and some scarcity of blood supply. Although it causes less damage to the heart, it is still serious and needs prompt diagnosis and treatment. This mini heart attack symptoms may resemble a regular heart attack symptom.
- Unstable angina: It is also known as a silent heart attack, which can be similar to a STEMI heart attack and may be mistaken for indigestion, muscle pain, and more. It occurs due to excessive tightening of heart arteries, resulting in a drastic reduction of blood supply.
However, diagnostic tests may not show the damage to the heart. Although it is not seriously restricting the blood supply to the heart, it increases the risk of heart attack.
Heart attack symptoms
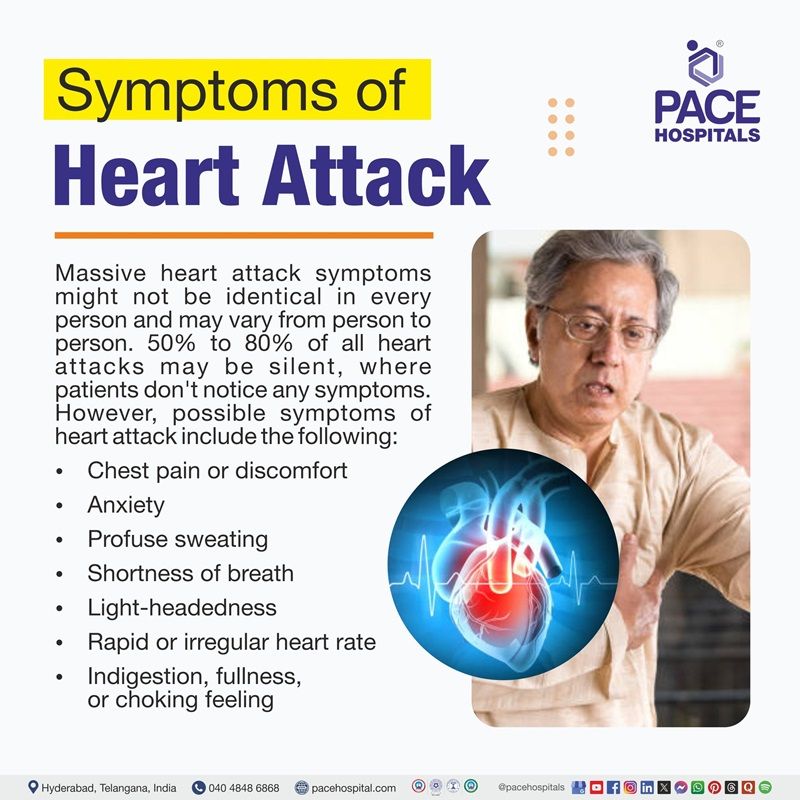
Massive heart attack symptoms might not be identical in every person and may vary from person to person. 50% to 80% of all heart attacks may be silent, where patients don't notice any symptoms. However, possible symptoms of heart attack include the following:
- Chest pain or discomfort: This pain may radiate to arms, shoulders, neck, back, jaw, or stomach (in some cases).
- Anxiety: It may be expected in patients with coronary heart disease (CHD), often displaying feelings of extreme worry.
- Profuse sweating: Pumping blood through blocked arteries may take more effort from the heart, leading to excess sweating for balancing the body temperature.
- Shortness of breath: The patient may not be able to take enough breath, along with chest discomfort.
- Light-headedness: It may be caused due to the reduced blood supply throughout the body.
- Rapid or irregular heart rate: If the patient's oxygen supply is decreased, it may disrupt the heart's electrical activity, resulting in fast or uneven heartbeats as a response to stress and damage to the myocardium.
- Indigestion, fullness, or choking feeling
- Nausea with or without vomiting
Patients having a heart attack often experience chest pain and might notice early warning signs of a heart attack such as fatigue, cold sweats, discomfort, or a general feeling of sickness in the days leading up to the attack. However, a particular type called ST-elevation myocardial infarction (STEMI) can occur suddenly without any warning signs.
Heart attack symptoms in women
Signs of heart attack in women include chest pain or discomfort, but they are more prone than men to experience heart attack without any chest pain or discomfort. Nausea, dizziness or extreme fatigue, and shortness of breath are the common heart attack symptoms in women. Women might experience these types of common symptoms before a heart attack, and most of them are similar to the symptoms of heart attack in men.
Heart attack causes
Massive heart attack causes include the following:
- Coronary artery disease: Blockage or narrowing of coronary arteries. The leading cause of heart attack is a condition known as coronary artery disease. However, some (5%) heart attacks may occur due to another cause such as
- Coronary artery spasm: Unusual narrowing of blood vessels.
- Coronary artery dissection: Sudden tear in the wall of a coronary artery.
- Uncommon medical conditions: Any disease that may cause unusual narrowing of blood vessels.
- Anomalous coronary arteries: A congenital heart defect.
- Stress cardiomyopathy or broken heart syndrome: A sudden weakness in heart muscle.
- Electrolyte imbalance: It is linked with cardiovascular emergencies and cause serious issues such as seizures, coma, and cardiac arrest
- Obstruction: Migrated from other areas in the body.
- Causes for sudden heart attack
- Hypertrophic cardiomyopathy: A condition that is characterized by the thickening of the heart muscle.
- Coronary artery abnormalities: A congenital condition that is characterized by a defect in one or more of the coronary arteries of the heart.
- Primary arrhythmias: Fluttering, racing, or pounding (irregular) heartbeats that occur within the heart.
- Arrhythmogenic right ventricular dysplasia: Uncommon, fatal disorder presented with dangerous heart rhythms.
- Myocarditis: Inflammation of the heart muscle called myocardium
- Marfan syndrome: An inherited condition that affects connective tissue.
The causes of a heart attack in women are the same as in men. However, women are more prone to MI that are not caused by coronary artery disease than men.
Heart attack risk factors
Heart attack risk factors are strongly associated with coronary artery disease (CAD). The following are the modifiable and non-modifiable risk factors of heart attack:
INTERHEART study identified many modifiable risk factors for CAD. The following are the myocardial infarction modifiable risk factors:
- Smoking: As per the INTERHEART studies, it was found that smoking causes heart attacks by increasing the formation of plaque in blood vessels.
- Hypertension: It may increase the workload of the heart, leading to structural and functional changes in heart muscle. As per some studies, it was proved that untreated high BP causes heart attack or increases the risk of heart disease.
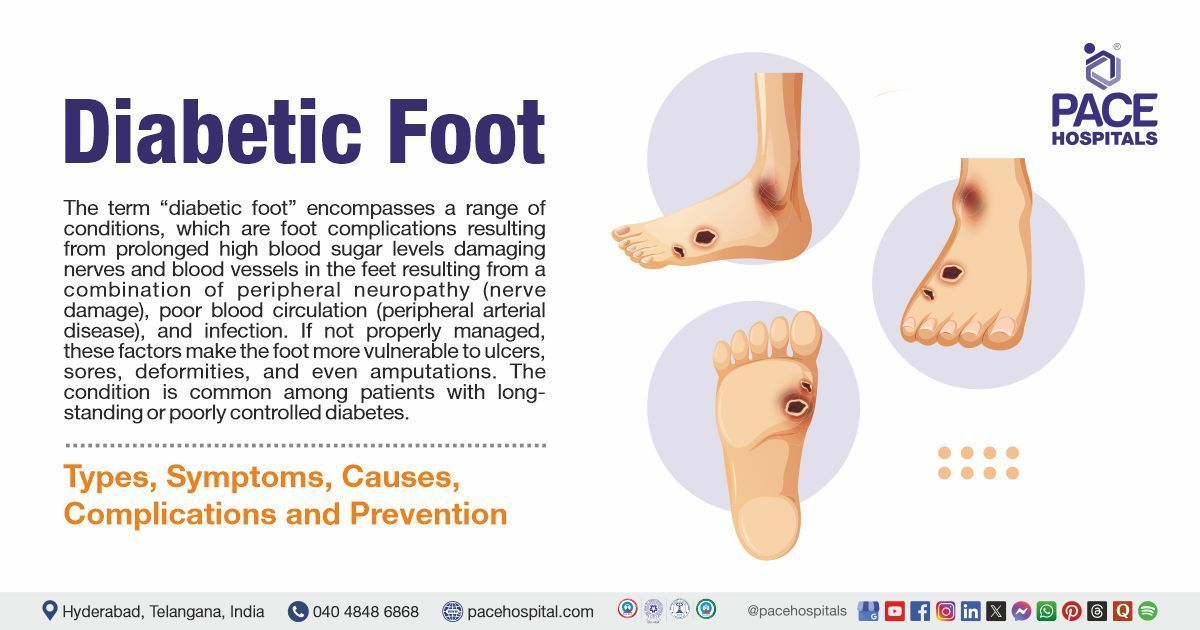
- Diabetes mellitus: Elevated blood sugar levels may harm the nerves and the blood vessels that control the person's heart.
- Abnormal lipid profile: Having a high lipid can raise the chances of development of heart disease.
- Alcohol consumption: Consuming can raise blood pressure and heartbeat, which may increase the workload on the heart and the risk of heart disease.
- Lack of physical activity: Sedentary lifestyles may lead to weight gain, which elevates the risk of high blood pressure, cholesterol, and diabetes.
- Obesity: Obese persons tend to have more blood, due to that, the heart pumps harder and may lead to heart disease over time.
- High-stress levels: Increased stress levels can release cortisol (stress hormone) and temporarily raise blood pressure. Chronic (long-term) stress can lead to increased blood pressure.
These factors should be modified to aid in reducing the risk of heart disease. Heart attack causes, and risk factors are not the same but might be linked in many cases.
The following are the non-modifiable risk factors for myocardial infarction:
- Older age: The risk of heart attack may increase as a person gets older
- Male gender: Males are more suspectable to heart attack than woman
- Family history: A family history of stroke or heart disease may raise the risk of heart disease
Heart attack complications
Heart attack complications can be serious, and include as the following:
Ischemic (common in first few days)
- Angina pectoris: It is a condition that is characterised by chest pain caused by decreased blood flow to the myocardium
- Extension of infraction: Damage to a new area occurring after the first injury
- Reinfarction: Another heart attack (second heart attack) that occurs after the first heart attack
Arrhythmias (within 1–3 days)
- Sinus bradycardia: Slow heart rate that develops in the sinus node and
- Atrioventricular block: Disruption of electrical signals between the lower and upper chambers of the heart, leading to slowed conduction of signals
- Supraventricular arrhythmia: Unusual or abnormal heartbeat originates in atria (upper chambers) or
- Ventricular arrhythmia: Unusual or abnormal heartbeat originates in the ventricles (lower chambers)
Mechanical (usually 1st week to 1st month)
- Cardiogenic shock: Severe damage to heart muscles
- Heart rupture: Where the heart’s muscles, valves, or walls split apart
- Heart failure: Heart muscle cannot pump enough blood
- Myocardial dysfunction: It refers to a range of conditions that cause weakened heart muscle
Embolic (within first 2 weeks)
- Pericardial embolus: Blockage in a blood vessel that
- Left ventricular mural thrombus: Blood clot that develops in the inner wall of the left ventricle
Inflammatory: (first week to months)
- Pericardial effusion: Blocks blood supply to the heart sac
- Pericarditis: Inflammation and swelling of thin, sac-like tissue called pericardium (surrounds the heart)
The post heart attack complications may happen rapidly after a heart attack and become a cause of death. Within the 1st month after the heart attack or before reaching the hospital, some individuals die suddenly from a complication of heart attack.
Heart attack diagnosis
Heart attack diagnosis tests may start with a physical exam by a cardiologist using a stethoscope to find the abnormal sounds in the lungs (crackles). The following are the tests that might be performed to check heart health as well as to confirm the heart attack:
- History and symptoms
- Blood tests
- Electrocardiogram (ECG)
- Coronary angiography
- Exercise stress test
- Nuclear stress test
Silent heart attack diagnosis tests include electrocardiogram or echocardiogram stress test.
Heart attack treatment
If the patient receives heart attack treatment faster, there is a better chance to survive and alleviate the symptoms. It includes the following:
- First aid treatment for heart attack
- Medical management of myocardial infarction
- Surgical management of myocardial infarction
First aid treatment for heart attack
It is crucial to provide emergency management to a heart attack patient to prevent significant heart damage. Management of myocardial infarction may be classified into two types in the hospital as follows:
- Medical management of myocardial infarction
- Surgical management of myocardial infarction
The goal of the treatment is to restore blood flow quickly to reduce damage to the heart muscle. A cardiologist can choose the type of management based on the type of heart attack the patient has had and the overall condition of the patient.
Medical management of myocardial infarction
It is also called the pharmacological management of myocardial infarction, where medications are used to treat the heart attack. Medications for heart attack include the following:
- Thrombolytic therapy
- Oxygen therapy
- Anti-emetic drugs
- Pain medications
- Beta-blockers
- Blood thinners
- ACE inhibitors
- Statins
- Nitrates
- Antihypertensive drugs
Surgical management of myocardial infarction
Before proceeding with emergency surgery, a cardiologist may recognize signs of a heart attack, including an increased heartbeat and an irregular pulse. Blood pressure may initially be elevated but can drop later, leading to hypotension and cardiogenic shock, where the heart cannot pump enough blood and oxygen. The following surgical procedures can be performed by cardiothoracic surgeons or interventional cardiologists based on the patient's needs and condition:
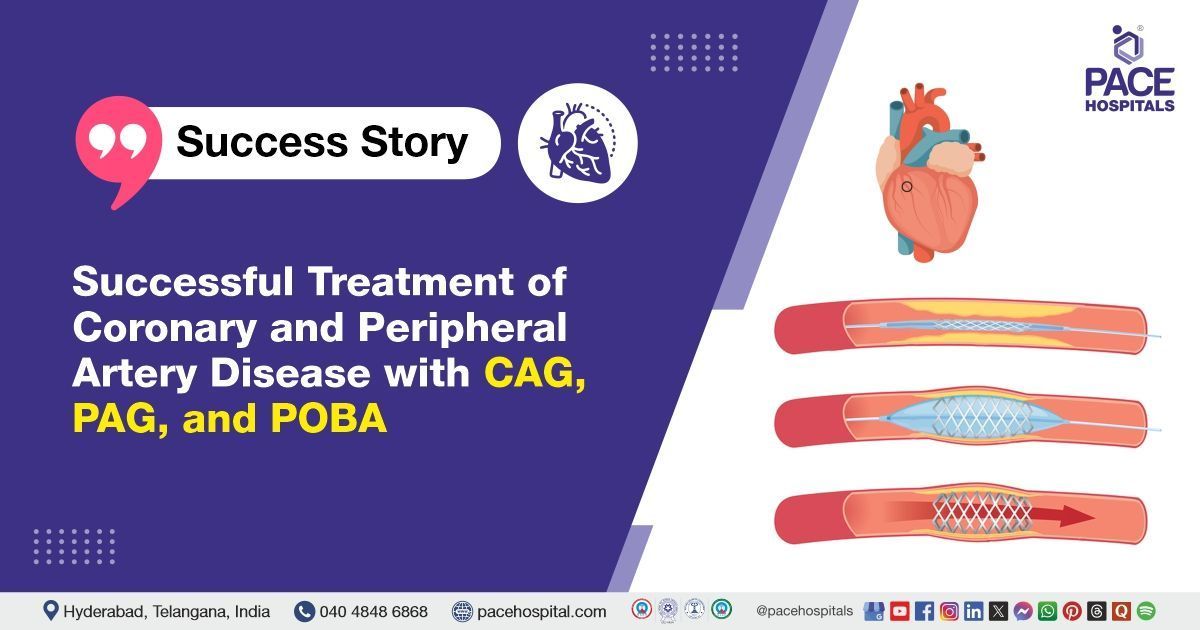
- Percutaneous Coronary Intervention (PCI)
- Balloon angioplasty
- Stent placement
- Coronary Artery Bypass Grafting (CABG) or bypass surgery
- Heart valve surgery
- Heart transplant
After a heart attack, cardiac rehabilitation and lifestyle modifications can help patients recover.
Heart attack prevention
Prevention of myocardial infarction may depend on many factors. It is not possible to control some risk factors, such as age and sex. However, many ways can help a person reduce the risk of a heart attack. These include:
- Getting regular health checkups: A checkup of overall health every year might detect early warning signs of heart disease, including symptoms that patients cannot feel.
- Stopping smoking: Quitting smoking and all vaping products can decrease the risk of heart disease.
- Maintaining a healthy weight: This may help prevent cholesterol deposition in arteries.
- Exercising regularly: Moderate physical activity four to five days a week can help achieve a healthy weight and lower the risk of heart attack.
- Managing the stress: Stress can increase the risk of heart disease; controlling the stress may help stay away from it.
- Eating healthy food: A healthy, balanced diet, which contains high protein and fibre foods, and avoiding highly saturated foods, is advised.
- Managing the existing conditions: Medical conditions, including high blood pressure, diabetes, obesity, etc, may increase the risk of heart disease. It is recommended to manage them to avoid getting heart problems.
- Limiting alcohol intake: Alcohol consumption can raise blood pressure and heart rate. Hence, a person may be less likely to get heart disease by limiting alcohol.
Patients have to take the prescribed medicine for heart attack prevention regularly.
Difference between cardiac arrest and heart attack
Cardiac arrest vs heart attack
Cardiac arrest and heart attack are the conditions that cause damage to the heart. Although these are similar, they have some differences:
| Elements | Cardiac arrest | Heart attack |
|---|---|---|
| Definition | Cardiac arrest is an electrical problem characterised by sudden stoppage of the heartbeat due to the sudden triggering of an electrical malfunction, resulting in an irregular heartbeat. | A heart attack is a circulation problem characterised by blockage of blood flow to the heart muscle. |
| Causes | The leading cause of cardiac arrest is ventricular tachycardia or ventricular fibrillation, which are types of arrhythmias. | Blockage of coronary arteries with plaque, leading to blood clots and preventing the blood from flowing to the heart |
| Symptoms | No warning Initially, the patient may pass out and become unconscious | Chest pain is the main symptom of a heart attack Others include light-headedness, fatigue, shortness of breath, and nausea |
| Risk factors | Essential risk factors include prior cardiac arrest, congenital heart defects, coronary heart disease, heart valve disease, and arrhythmias caused by faulty gene. | Risk factors for heart attack might include smoking, elevated blood pressure, older age, stress, family history of heart disease, and atherosclerosis. |
| What happens | The heart rhythm may stop the pumping of blood over the body, which might lead to death within minutes. | The heart muscle may die due to lack of oxygen, but the heart continues to beat. |
| Time frame | It may happen within seconds, the patient loses consciousness, and death also occurs if prior treatment is not given. | It can be silent and unnoticed; however, it progresses through symptoms over hours to days. |
| What to do? | Call an ambulance, if possible, perform the CPR and AED | Call the ambulance. If the patient is not breathing and doesn’t find a pulse, perform CPR |
Difference between heart failure and heart attack
Heart failure vs heart attack
Heart failure and heart attack are both types of heart disease. Although they have some common causes, they may also differ in many ways such as:
| Elements | Heart failure | Heart attack |
|---|---|---|
| Definition | Heart failure or congestive heart failure is characterised by the inability of the heart to pump efficiently. | It is a sudden loss of blood supply to the myocardium (heart muscle). |
| Causes | It may be caused by coronary artery disease, genetic cardiomyopathy, faulty heart valves, irregular heartbeat, acquired heart disease. | The Leading cause of this condition is CAD-coronary artery disease. |
| Symptoms | Symptoms of left-sided heart failure may include fatigue, bluish colour of lips or fingers, sleepiness, and trouble breathing. However, symptoms of right-sided heart failure may include nausea, abdominal pain, weight gain, loss of appetite, and urination frequently. | Chest pain or discomfort is the key symptom of a heart attack that radiates to the neck, shoulders, jaws, and neck. Others include light-headedness, fatigue, shortness of breath, and nausea. |
| Diagnosis | Usually, it includes medical history, physical examination, echocardiogram, CT scan, MRI scan, EKG, and stress tests. | Diagnostic tests may involve blood, stress, electrocardiogram (EKG), and coronary angiography. |
| Treatment | It has no cure; however, treatments aim to aid a person to live longer with reduced symptoms. The choice of treatment may depend on the type of heart failure. | Treatment may be given to reduce blood pressure, clotting, and strain on the heart. |
Difference between panic attack and heart attack
Panic attack vs heart attack
Panic attacks and heart attacks are different medical conditions. However, they both impact the heart health. Such as:
| Elements | Panic attack | Heart attack |
|---|---|---|
| Definition | It happens when stress hormones trigger the person's fight or flight response, which may elevate the heart rate. | It is the condition where the patient's heart lacks the blood supply. |
| Symptoms | In this condition, the symptoms may resolve within 20-30 minutes, including sweating, trembling, increased or racing heart rate, tingling in the hands, and pain that gets better over time. | Chest pain or discomfort (main symptom) and others include coughing, cold-sweating, light-headedness, fatigue, shortness of breath, and nausea. |
| Causes | It might be triggered by different factors such as genetics (family history of panic disorder), stressful life events, imbalances in neurotransmitters, medical conditions, use of substances (alcohol, caffeine, drugs), phobias, or triggers. | It is majorly caused by coronary artery disease, and other causes include coronary artery spasm, coronary artery dissection, and uncommon medical conditions. |
| Time and duration | It lasts for a few minutes and gets better over the time. | It lasts from minutes to hours and becomes worse with time. |
| Severity | It may not be life-threatening. However, it may cause distress. | It is a medical crisis and requires immediate help. |
Frequently Asked Questions (FAQs) on Heart attack
Can anxiety cause a heart attack?
No, anxiety does not directly cause a heart attack. However, it might play a role in the development of coronary artery disease (CAD) due to irregular fluctuations in blood pressure, which can lead to high blood pressure, disturbances in heart rhythm, or even a heart attack.
A faulty stress response might promote inflammation, which can damage the artery linings and lead to the buildup of coronary plaque. Hence, it is recommended to manage stress to reduce the risk of heart problems.
Can a heart attack occur without symptoms?
Yes, a heart attack can occur without noticeable symptoms, a condition called a "silent heart attack." People may not experience typical chest pain or discomfort, but it can still cause damage to the heart muscle, which can be detected later through tests like an ECG.
What lifestyle changes can prevent a heart attack?
Adopting a healthy lifestyle, including eating a balanced diet rich in fruits, whole grains and vegetables, exercising regularly, avoiding smoking, limiting alcohol, and managing stress, can significantly lower the risk of a heart attack. Maintaining a healthy weight and monitoring cholesterol levels are also crucial.
How does high blood pressure contribute to heart attacks?
High blood pressure can damage the blood vessels over time, making them less elastic and more prone to plaque buildup, increasing the risk of blockages in the arteries, which can lead to a heart attack. It also forces the heart to work harder, contributing to heart disease.
Can a child have a heart attack?
No, a child can rarely have a heart attack. However, the child may develop heart disease or heart attack, especially if they have any of the following conditions:
- Congenital heart disease (birth-related heart conditions) e.g., Anomalous origin of the left coronary artery
- Acquired heart disease, e.g.: Rheumatic heart disease and Kawasaki disease
- Chest trauma
What are the 5 types of myocardial infarction?
The following are clinically classified into five types based on the cause and circumstances of the event:
- Type 1: Spontaneous MI because of coronary plaque erosion or rupture with occlusive (blockage) or non-occlusive thrombus.
- Type 2: MI due to imbalance such as due to increased or decreased supply in oxygen, demand, or supply without any evidence of coronary plaque disrupture. e.g., coronary embolism, coronary artery spasm, arrhythmias, anaemia, hypertension or hypotension
- Type 3: Sudden cardiac death (cardiac arrest) occurs with suggestive symptoms of myocardial ischemia (detection of myocardial ischemia in autopsy examination).
- Type 4: MI related to prior coronary intervention - 4a: After percutaneous coronary intervention (PCI) and 4b: Due to scaffold thrombosis or stent thrombosis as documented by angiography or at autopsy
- Type 5: MI linked to coronary artery bypass grafting (CABG)
Why is ST elevation in myocardial infarction?
ST elevation in MI reflects damage to the heart muscle or transmural ischemia caused by a blocked coronary artery. It happens because of changes that occur in electrical activity, reflected as elevated ST segments on ECG (electrocardiogram), which indicates acute heart muscle injury or heart muscle death.
How does myocardial infarction cause arrhythmia?
MI may cause arrhythmias by interrupting the normal electrical activity of the heart, leading to unstable electronic conditions and abnormal heart rhythms due to conduction block, tissue damage, scar formation, electrolyte imbalances (e.g., hypokalaemia and hypomagnesemia), hypoxia. Patients may develop arrhythmias in the first week after MI as a result of damage to the heart muscles.
Pain in a heart attack patient may radiate from the center of the chest or left side to the neck, shoulders, back, lower jaw, or arms (especially left), and rarely in the stomach (below the ribs in the middle of the patient upper abdomen), occurs because of shared nerve pathways between the upper abdominal region and heart, may lead to referred pain. This sensation or pain may mimic the gastric discomfort or indigestion and confuse the symptoms of a heart attack.
How to stop a heart attack in 30 seconds?
It is not possible to stop a heart attack on one's own. Taking immediate medical treatment is the only way to prevent heart damage.
However, a nearby person may perform first-aid treatment on the patient until medical help arrives. For example, if the patient is not breathing or does not have a pulse, begin CPR, which involves hard and fast chest compressions at a rapid rhythm of 100–120 compressions per minute to restore oxygen and blood flow.
How does a heart attack feel like?
The heart attack pain or discomfort may feel like squeezing or aching, uncomfortable pressure, or tightness that spreads to the back, shoulder, neck, jaw, teeth, or upper belly, and the patient may feel sick or weak, light-headed or faint, and cold sweat.
Most heart attacks or myocardial infarctions are characterized by the discomfort or pain on the left side or center of the chest that is persistent (lasts for more than a few minutes) or that goes away and comes back again.
Is heart attack genetic?
No, heart attacks are not completely genetic, but having a family history of heart attack, stroke or being diagnosed with heart disease before the age of 60 may increase the risk of heart disease, or chances of developing this condition may be higher than normal people. However, other factors such as diet, lifestyle, physical activity, and other medical conditions also play a significant role.
What is the heart rate during a heart attack?
As per a study, it was found that patients with a heart rate of above 80 beats/minute at the time of treatment had a higher risk of death from heart attack. However, according to the American Heart Association, having an elevated heart rate is not a well-grounded sign (reliable indication) of a heart attack.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Hafeezpet, Madeenaguda, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc).

CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
FOLLOW US
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital near me.