Heart Failure: Symptoms, Causes, Types, Diagnosis, Treatment and Prevention
Heart failure definition
Heart failure, also called congestive heart failure, is a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood. The four most common causes that are responsible for about two-thirds of congestive heart failure are ischemic heart disease (IHD), chronic obstructive pulmonary disease (COPD), hypertensive heart disease, and rheumatic heart disease (RHD). Difficulty in breathing, extreme tiredness, swelling in ankles and legs, and lightheadedness are common symptoms of heart failure. The treatment aims to relieve systemic and pulmonary congestion and stabilizing hemodynamic status. A cardiologist can treat heart failure.
Heart failure meaning
Heart failure is a combination of two words
The term “heart” is derived from Old English “heorte " which means a hollow muscular organ that circulates blood.
The term “failure” is derived from the Anglo-French word “failer” which means the act of failing, it is also derived from Old French “falir " which means to be lacking; or not succeed.
Heart failure prevalence
Heart failure prevalence worldwide
In the year 2017, approximately 12 lakhs of hospitalizations were due to congestive heart failure. The current prevalence of congestive heart failure is 643.4 lakhs as per the Global Health Data Exchange registry. According to the Framingham Heart Study, the prevalence of heart failure is 8 per 1000 males aged between 50 to 59 years, with an increase to 66 per 1000 males aged 80 to 89. Heart failure incidence in men doubles with each 10-year age increase after the age of 65, whereas in women, the prevalence for the same age cohort, the incidence triples.
Heart failure prevalence in India
Based on disease specific estimates the prevalence of heart failure in India due to coronary heart disease (CAD), hypertension, obesity, diabetes, and rheumatic heart disease (RHD) ranges from 13 lakhs to 46 lakhs with an annual incidence of 4.916 lakhs to 18 lakhs. Because of the lack of surveillance systems to adequately capture the data the incidence and prevalence estimates of heart failure (HF) are unreliable in India.

Types of heart failure
The type of heart failure is named for where it occurs in the heart. The heart failure can affect either the right side or the left side of the heart and sometimes both halves are affected. The following are the types of heart failure:
- Left-Sided Heart Failure
- Heart Failure with Reduced Ejection Fraction (HFrEF)
- Heart Failure with Preserved Ejection Fraction (HFpEF)
- Right-Sided Heart Failure
- Biventricular Heart Failure
- Congestive Heart Failure (CHF)
Left sided heart failure
This type of heart failure involves the left ventricle of the heart (bottom left chamber of the heart). When enough blood is not pumped through the left ventricle, the blood backs up in the blood vessels that carry blood away from the lungs. Left sided heart failure is the most common type of heart failure which causes breathing issues. It can be further classified as heart failure with a reduced or preserved ejection fraction. They are described as follows:
- Heart failure with reduced ejection fraction: It is also called systolic heart failure; it is a heart failure with left ventricular ejection fraction less than or equal to 40 percent. The left ventricle cannot contract normally thereby resulting in reduced blood in circulation.
- Heart failure with preserved ejection fraction: Also called diastolic heart failure. In this, the left ventricle of the heart cannot relax normally. As a result, the heart cannot fill the blood between the beats and the blood backs up in the blood vessels that carry blood to the lungs. Heart failure with preserved ejection fraction is heart failure with left ventricle ejection fraction less than or equal to 50 percent.
Right-sided heart failure
This type of heart failure involves the right ventricle of the heart (bottom right chamber of the heart). In blood vessels that carry blood from the rest of the body to the heart, the blood backs up due to the insufficient blood pumping capacity of the right ventricle. This can result in swelling and inflammation due to pushing fluids out of the veins into the surrounding tissue.
Biventricular heart failure
It is a combination of left side and right sided failure involving both sides of the heart. In this type, the symptoms can be mixed (symptoms of both right and left heart failure).
Congestive heart failure (CHF)
It is a type of heart failure, and sometimes doctors use the two terms congestive heart failure and heart failure interchangeably. It is a weakened heart condition which results in fluid buildup in the feet, arms, lungs, and other organs. Shortness of breath (SOB), fatigue, arrhythmias (irregular heart rhythm) and edema are some of the symptoms of congestive heart failure.
Classification of heart failure based on the course of the disease
Heart failure can be classified based on the time of onset as:
Acute heart failure
This refers to a sudden onset or worsening of heart failure symptoms. It's a medical emergency requiring immediate treatment and hospitalization. Triggers can include a heart attack, uncontrolled high blood pressure, infection, or other acute illnesses.
Chronic heart failure
This is a long-term condition where the heart's ability to pump blood is progressively impaired. Symptoms may be present at rest or only with exertion and require ongoing management with medication, lifestyle changes, and sometimes devices or procedures. Acute episodes can occur within the context of chronic heart failure.
Causes of heart failure
Etiologies are broadly classified as intrinsic heart disease and pathologies that are infiltrative, valvular, congenital, myocarditis related, high output failure, and secondary to systemic disease. Ischemic heart disease (IHD), chronic obstructive pulmonary disease (COPD), hypertensive heart disease, and rheumatic heart disease (RHD) are the four most common etiologies that are responsible for 2/3rd of the cases. The congestive heart failure causes are as follows:
- Ischemic heart disease: It is the most common cause of congestive heart failure all around the world. The incidence of ischemic heart disease is increasing in developing countries as they follow Western diets and lifestyles. In these countries, the infectious burden has decreased by improved medical care.
- Valvular heart disease: It is a common intrinsic heart condition which causes congestive heart failure (CHF). In children and young adults, the common cause of valvular heart disease is rheumatic heart disease. Valvular heart disease is caused by an immune response to group A streptococcus, and age-related degeneration is also a the most common cause of valvular heart disease.
- Hypertension: Even in the absence of coronary artery disease or ischemic heart disease hypertension can cause heart failure. It is strongly associated with other co-morbidities for the development of congestive heart failure (CHF). Treating hypertension has been shown to lower the incidence of congestive heart failure.
- Cardiomyopathy: It is a heterogeneous group of diseases which are characterized by enlarged ventricles with impaired function which is not related to secondary causes such as ischemic heart disease (IHD), valvular heart disease (VHD), hypertension, or congenital heart disease.
- Inflammatory cardiomyopathy: Viral infection is the most common cause of inflammatory cardiomyopathy. Some other causes include bacterial, fungal, or protozoal infections; toxic substances or drugs; and immune-mediated diseases. Adenoviruses, enteroviruses, herpes virus 6, Epstein-Barr virus, and cytomegalovirus are some of the viral causes of myocarditis and inflammatory cardiomyopathy.
- Infiltrative cardiomyopathy: It causes a restrictive cardiomyopathy that is similar to genetically determined restrictive cardiomyopathy variant which marks normal ventricular systolic function.
- Stress-induced cardiomyopathy or Takotsubo: It is informally called broken heart syndrome, and it is an underrecognized cause of congestive heart failure that results in transient left-ventricular wall abnormalities.
- Peripartum cardiomyopathy: It is a main cause of maternal mortality, and it presents congestive heart failure due to LV systolic dysfunction that occurs during late pregnancy, postpartum, or up to several months after delivery.
- Obesity: As per the "Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity" study obesity is a leading cause of congestive heart failure in patients younger than 40 years of age.
- Tachycardia: Both tachycardia and arrythmias can induce a low output state in congestive heart failure. Factors such as electrophysiologic changes including prolonged duration and reduced amplitude of action potentials in the myocytes can induce typical neurohormonal response which ultimately leads to heart failure.
- Thyrotoxicosis: It is one of the rare causes of heart failure and occurs due to activation of the renin-angiotensin-aldosterone axis, which causes retention of sodium and water, as well as the upregulation of erythropoietin-stimulating agents, both of which increases blood volume.
- High output cardiac failure: It is associated with thiamine deficiency, a rare condition which is found primarily among patients who are elderly, homeless, or have alcohol abuse disorder. This deficiency of thiamine causes decreased ATP production and an accumulation of adenosine, causing systemic vasodilation. This leads to lowered systemic vascular resistance and increases cardiac output.
Heart failure symptoms
Heart failure presents signs and symptoms of congestion and may also present with organ hypoperfusion or cardiogenic shock and shortness of breath as the most commonly reported symptom. The following are some of the congestive heart failure symptoms:
Common symptoms of heart failure
Patients with congestive heart failure may present signs of congestion. The following are some of the common signs and symptoms of congestive heart failure:
- Shortness of breath (SOB)
- Fatigue (tiredness)
- Swollen ankles and legs
- Lightheadedness
- Fainting
Less common symptoms of heart failure
The following are some of the less common symptoms of heart failure:
- A persistent cough which worsens at night
- Bloating tummy
- Wheezing
- Loss of appetite
- Weight loss or weight gain
- Confusion
- Increased heart rate
- Irregular heartbeat
Risk factors for heart failure
Risk factor can be anything which can increase the likelihood of developing a disease. There are several risk factors that contribute to the development of heart failure. Congestive heart failure risk factors are categorized below:
Modifiable risk factors for heart failure
Risk factors which can be modified by lifestyle changes are called modifiable risk factors. The following are some of the modifiable risk factors for heart failure:
- Hypertension: High blood pressure is a major risk factor for cardiovascular diseases. Due to uncontrolled blood pressure, the blood vessels of the heart get thicken or gets stiffen, forcing the heart to work harder.
- Diabetes: Over time high blood glucose levels can damage the blood vessels restricting the blood supply to the muscles of the heart. This insufficient blood supply can weaken the heart and lead to heart failure.
- Cholesterol: High cholesterol levels in the blood can build up fatty deposits in the arteries, narrowing the blood vessels and blocking the blood supply to the heart which weakens the heart and eventually lead to heart failure.
- Smoking: It is one of the major risk factors for heart diseases. The chemicals present in cigarette damage the blood vessels of the heart. Over time they cause narrowing of heart muscles which blocks or interrupts the blood supply to the heart and leads to heart failure.
- Alcohol: Excessive alcohol consumption can result in high blood pressure and obesity which in turn are the major risk factors for heart failure. It can also lead to cardiomyopathy, a disorder that affects the muscles of the heart.
- Obesity: Obesity or being overweight can increase the blood volume due to excess fat causing the heart to work harder and leading to a condition called ventricular hypertrophy. Obesity can also lead to other risk factors such as high blood pressure and increased inflammation which can strain the heart leading to heart failure.
- Diet: A diet which is high in saturated and trans fats causes buildup of cholesterol levels in the arteries which blocks the blood supply to the heart leading to heart failure.
- Lack of physical activity: Regular exercise strengthens the heart and improves the blood supply throughout the body. A sedentary lifestyle with no physical activities can weaken the heart muscles and contribute to heart failure.
Non-modifiable risk factors for heart failure
These factors cannot be controlled and modified by lifestyle modifications. The following are some of the non-modifiable risk factors:
- Gender: The type of heart failure differs according to gender. Heart failure with preserved ejection fraction has a greater prevalence in women and heart failure with reduced ejection fraction is higher in men.
- Race: It significantly increases the risk of heart failure. Black men have a 70 percent higher risk of developing heart failure compared to white men. Black adults are twice as likely to be hospitalized for heart failure compared to white adults.
- Family history: Genetic predisposition plays an important role in cardiovascular health. Individuals with family history of heart disease, hypertension, and diabetes are at an increased risk of developing heart failure.
- Advancing age: With advancing age the structural and functional changes of the heart increase and over time the arteries stiffen which decreases cardiac efficiency and increases the risk of atrial fibrillation leading to heart failure.
Complications of heart failure
Heart failure occurs when the heart is not capable of pumping enough blood. It can damage the heart, liver, lungs, kidneys, and other organs. Complications of congestive heart failure include the following:
- Reduced quality of life: Heart failure patients experience different physical and emotional symptoms such as shortness of breath, extreme fatigue (tiredness). The everyday routine such as physical and social activities is limited by these symptoms and results in poor quality of life.
- Cardiac cachexia: Heart failure can lead to cardiac cachexia. Cardiac cachexia is a condition that causes muscle wasting and significant weight loss in people with advanced heart failure.
- Arrhythmia and sudden cardiac death: Structural changes in the muscle of the heart causes abnormal electrical signals of the heart leading to arrhythmias. A failing heart can disrupt its own electrical signal.
- Cardiorenal disease: Heart failure can lead to cardiorenal disease by causing decreased blood supply to the kidneys due to decreased cardiac output leading to impaired kidney function which progresses to chronic kidney failure.
- Liver dysfunction: Congestion in the liver due to decreased cardiac output can damage liver cells leading to a condition known as liver cirrhosis.
- Mural thrombi and risk of thromboembolism: Due to poor contractility the blood stasis within the weekend heart chamber, combines with endothelial damage increasing the risk of clot formation.
- Recurrent hospitalizations: Heart failure requires frequent hospital admissions and long hospital stays as it is a medical emergency.
Congestive heart failure diagnosis
Heart failure diagnosis is primarily based on the presence and severity of symptoms and physical exam findings. When evaluating a heart failure patient, a comprehensive assessment is needed which includes a complete blood picture, iron profile, renal profile, and liver profile. The following are the steps involved in diagnosing heart failure:
Initial evaluation
- Medical history
- Physical examination
Diagnostic tests
- Laboratory tests (Basic metabolic and blood panel)
- Complete Blood Count (CBC)
- Complete renal profile
- Liver profile
- Urine examination
- Serum B-type natriuretic peptide (BNP) or N-terminal pro-BNP
- Troponin-I or Troponin-T
- Electrocardiogram (ECG)
- Imaging studies
- Chest radiographs
- Echocardiography
- Computed tomography
- SPECT-Myocardial Perfusion Imaging
- Cardiac magnetic resonance imaging
- Noninvasive stress imaging
- Radionuclide multiple-gated acquisition (MUGA) scan
- Other tests
- Genetic testing
- Cardiac catheterization
Heart failure treatment
There is no cure for heart failure. Treatment helps in relieving symptoms and prevents further damage to the heart. The goal of therapy for heart failure is to improve symptoms and quality of life, decrease hospitalizations, and improve cardiac mortality. The following are the steps involved in congestive heart failure treatment:
Nonpharmacological treatment for heart failure
Heart failure represents a significant public health concern with increasing prevalence, morbidity, and mortality despite increasing advancements in pharmacologic therapies. The following are the nonpharmacological measures for treating heart failure:
- Physical activity
- Dietary modifications
- Weight management
- Smoking cessation
- Stress management
- Adequate sleep
- Cardiac contractility modulation (CCM)
Pharmacological treatment of heart failure
The primary goal of pharmacologic therapy is to control symptoms of heart failure and to administer drugs that reduce mortality and morbidity in heart failure. The following are the drug classes used in treating heart failure:
- Vasodilators
- Diuretics
- Aldosterone inhibitors
- ACE inhibitors
- Anticoagulants or antiplatelets
- Digitalis glycosides
- Beta-blockers
- Tranquilizers
Surgical management of heart failure
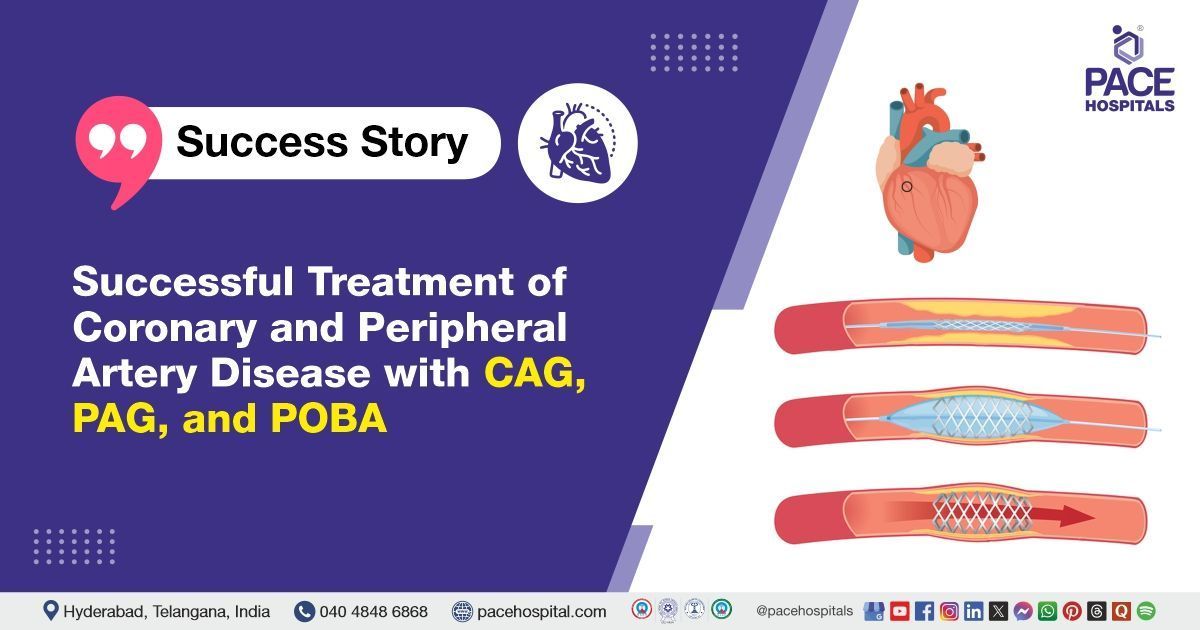
Surgery is required in severe cases to open or bypass the blocked arteries or to replace the valves of the heart. The following are some surgical procedures involved in treating heart failure:
- Heart valve surgery
- Coronary angioplasty or bypass
- Biventricular pacing therapy
- Implantable cardioverter defibrillator (ICD)
- Ventricular assist devices (VAD therapy)
- Cardiac resynchronization therapy (CRT)
- Heart transplant
Heart failure prevention
The best way to prevent heart failure is to avoid the conditions that can contribute to the development of heart failure. The following are some of the measures of congestive heart failure prevention:
- Avoid smoking: Smoking is one of the major risk factors for cardiovascular diseases. Smoking can permanently damage the blood vessels of the heart. Therefore, smoking cessation is important to reduce or prevent cardiovascular complications.
- Diet: It is an important risk factor in cardiovascular diseases. Fatty deposits from an unhealthy diet can gradually build up on the inside of the artery walls, narrowing the arteries which can block the blood flow. Following a diet that is heart healthy which is low-saturated fat, high-fiber, high-plant food diet can substantially reduce the risk of developing heart disease.
- Body weight: Obesity or being overweight can increase the risk of high blood pressure, diabetes, and high cholesterol levels which in turn are major risk factors for heart failure. Maintaining an ideal body weight is crucial as weight loss is considered a therapeutical goal in treating heart diseases.
- Treating comorbidities: It is important to treat underlying conditions like hypertension, diabetes, and high cholesterol, as these are major risk factors for heart failure.
Difference between heart attack and heart failure
heart attack vs heart failure
Heart attack and heart failure are both cardiovascular diseases. A heart attack refers to the damage to the heart muscle that is caused due to prolonged ischemia whereas heart failure is a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood. The following are the parameters that differentiate a heart attack and heart failure:
| Parameters | Heart attack | Heart failure |
|---|---|---|
| Definition | A heart attack, also called myocardial infarction, is a medical emergency that is caused by the inadequate blood supply to one part of the myocardium. | Also called congestive heart failure, is a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood. |
| Symptoms | Chest pain, upper extremity pain, mandibular, or epigastric discomfort that occurs during rest. | Shortness of breath (SOB), fatigue (tiredness), swollen ankles and legs, lightheadedness and fainting. |
| Causes | It is closely related to coronary artery disease and is caused due to complete blockage of the blood supply. Risk factors include smoking, hypertension, diabetes, and dyslipidemia. | The four most common causes that are responsible for about two-thirds of congestive heart failure cases are ischemic heart disease (IHF), chronic obstructive pulmonary disease (COPD), hypertensive heart disease, and rheumatic heart disease (RHD). |
| Treatment | Reperfusion therapy is indicated in all patients. Drug classes such as nitrates, beta-blockers, and anti-thrombotic therapy are included in the management of myocardial ischemia. | It can be managed by a few lifestyle modifications, with the use of medications, devices implanted to control heart rhythms and surgical interventions. |
Frequently Asked Questions (FAQs) on Heart failure
Can heart failure be reversed?
Yes, heart failure can be reversed in some cases. Though heart failure is severe and life-limiting, it doesn’t always get worse and can be reversed. However, complete reversal is not always possible, especially if there's significant scaring or damage to the heart. The possibility of reversal is based on the cause and severity of the condition.
Can heart failure be cured?
There is no cure for heart failure, but it can be managed, which can help in living a longer life with fewer symptoms. The treatment is based on the type of heart failure and its severity. It can be managed by a few lifestyle modifications, with the use of medications, devices implanted to control heart rhythms and with surgical interventions.
What is life expectancy with congestive heart failure?
Life expectancy is high for heart failure patients, and it varies based on the severity of the condition, genetics, age, and other factors. A study of nearly 60,000 heart failure patients showed that survival rates were 75.9 percent at one year, 45.5 percent at five years, 24.5 percent at 10 years, and 12.7 percent at 15 years.
Can ECG detect heart failure?
Yes, ECG can detect heart failure. It is a simple noninvasive test that records the electrical activity of the heart. Any abnormality in the rhythm of the heart or damage to the heart muscles can change the electrical activity of the heart. The physician may examine the traces and specific features of heart failure. It may also show evidence of prior infarction, chamber enlargement, intraventricular conduction delay, or arrhythmia.
How is heart failure diagnosed?
Diagnosis of heart failure is primarily based on the presence and severity of symptoms and physical exam findings. It is diagnosed by considering the medical history and physical examination of the patient which is followed by a comprehensive assessment which includes laboratory tests, imaging studies, ECG, genetic testing, and cardiac catheterization.
Why is creatinine high in heart failure?
Creatinine levels are high in acute decompensated heart failure patients. It is due to vascular congestion, a mechanism which involves increased central venous pressure having a negative impact on the nephron, promoting greater absorption of water and sodium, and increased interstitial pressure which is the main physio-pathological mechanism along with impaired kidney function.
What is the treatment for heart failure?
Treatment generally depends on the type of heart failure and severity. Though there is no cure for heart failure, treatment can help manage the symptoms and improve life. The treatment plan includes medications, some lifestyle modifications such as quitting smoking, managing stress, and with surgical interventions.
Why is oxygen needed for congestive heart failure?
Oxygen therapy is often used often in the management of patients with cardiac diseases and investigated for more than a century. The role of supplemental oxygen therapy in these patients is to improve the oxygenation of diseased myocardial tissue of the heart.
Cardiac resynchronization therapy (CRT) also called a biventricular pacemaker is an advanced pacemaker which can be implanted in heart failure patients. These pacemakers send small electrical venesections every three or impulses to the left and right ventricles to help them contract at the same time, and they have shown stunning success in improving health and survival in heart failure patients.
A complete blood picture, iron profile, renal profile, and liver profile are used as initial diagnostics tests for diagnosing heart failure patients. Complete blood picture can detect anemia which indicates infection triggering heart failure, a complete renal profile indicates the degree of renal injury associated with heart failure and liver profile can indicate hepatic congestion which is secondary to heart failure.
How does heart failure feel like?
Patients with heart failure may feel short of breath, may feel tired even while resting, may feel an urge to urinate often, and may also feel nauseous. Apart from this heart failure is presented with cough, difficulty in sleep, and loss of appetite.
What ejection fraction indicates heart failure?
The percentage of blood that is pumped out by the left ventricle of the heart for every heartbeat is the ejection fraction. 55 percent to 65 percent is a normal, healthy ejection fraction. Ejection fraction, which is less than 40 percent, is considered as heart failure.
Does a defibrillator help with congestive heart failure?
Yes, implantable defibrillators can help in the treatment of congestive heart failure. They have proven to be more effective than drugs in reducing the risk of sudden-death in some patients. Empiric implantable cardioverter defibrillator (ICD) which targets the general public with mild to moderate heart failure can increase the impact of this therapy by helping prevent sudden death and to improving the long-term survival of the patients.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Hafeezpet, Madeenaguda, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc).

CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
FOLLOW US
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital near me.