Human metapneumovirus (HMPV): Symptoms, Causes, Complications, Treatment and Prevention
Human metapneumovirus definition
Human metapneumovirus (HMPV) is a common cause of respiratory tract infections in infants, adults, the elderly, and people with impaired immune systems. It can cause cold-like symptoms like runny nose, sore throat and cough, etc. It was first discovered in the Netherlands in 2001 and has since spread worldwide. In 2016, the family was changed from Paramyxovirdae to Pneumoviridae.
This HMPV viral infection is more prominently observed in the winter. It is mainly transmitted through respiratory droplets from people infected with the virus. The virus targets epithelial cells in the respiratory tract, causing inflammation and clinical symptoms. The most common symptoms caused by HMPV infection are upper and/or lower respiratory tract infections, with lower respiratory tract infections being particularly common. Lower respiratory tract infections caused by HMPV can result in pneumonia, bronchiolitis, and acute asthma exacerbations.
As the virus grows slowly in cell culture, molecular techniques (such as reverse transcriptase PCR) are the primary diagnostic tool to detect HMPV. Currently, no vaccine is available, and the treatment is supportive.
Pulmonologists or infectious disease specialists often treat HMPV infections, particularly in cases of severe respiratory complications.
Human metapneumovirus meaning
Human metapneumovirus (HMPV) is a negative-sense, single-stranded RNA virus from the Pneumoviridae family. The term "metapneumovirus" is derived from the Greek language, where "meta" means "beyond" or "after," and "pneumon" refers to the lungs, emphasizing its connection to respiratory conditions. HMPV was initially found in 2001 in the Netherlands. It is closely linked to bird metapneumovirus, illustrating its zoonotic origins.
Human metapneumovirus prevalence
Prevalence of HMPV in the World
Human metapneumovirus was first identified in the Netherlands in 2001, causing clinical symptoms in children; however, serological studies showed that this pathogen had already been circulating in the Netherlands since 1958. HMPV infections can occur year-round, but peak prevalence in the northern hemisphere are seen in late winter and early spring.
These infections occur worldwide and are more prevalent among children, especially those under 2 years old, with an average age of approximately 22 months.
According to some studies, HMPV accounts for 90 to 100% of children aged 5 to 10. An estimated 142 lakh cases of HMPV-associated acute lower respiratory infections occurred in children worldwide in 2018, emphasising its significant impact on paediatric health.
Prevalence of HMPV in India
In India, the prevalence of Human Metapneumovirus (HMPV) among children with acute respiratory infections varies by area, with rates of 4% in Chennai, 5% in Pondicherry, and up to 12.7% in Vellore. Other studies have observed prevalence rates ranging from 3% to 5% in different locations, demonstrating that HMPV is an unneglectable respiratory infection in paediatric population across the country.
Human metapneumovirus types
Human metapneumovirus (HMPV) is divided into two distinct genetic lineages: Subtype A and Subtype B. Each subtype is then classified into two subgroups, leading to 4 different groups: A1, A2, B1, and B2. These subtypes have varying geographical distributions and can circulate concurrently during outbreaks, adding to the complexity of HMPV epidemiology.
Human metapneumovirus pathophysiology
The pathophysiology of HMPV includes the following:
- Viral structure: HMPV is a negative-sense single-stranded RNA virus from the Pneumoviridae family. Its genome is similar to that of the respiratory syncytial virus (RSV); however, it lacks certain non-structural genes.
- Infection mechanism: The virus infects airway epithelial cells by binding to them via glycoprotein interactions, particularly with heparan sulfate and other glycosaminoglycans. The fusion (F) protein facilitates the fusion between the viral envelope and the host cell membrane.
- Immune response: Upon infection, HMPV triggers an intense immunological response, including the release of chemokines and cytokines such as IL-6, IFN-alpha, TNF-alpha, and IL-2. This immune reaction can cause inflammation in the respiratory system, which contributes to symptoms like cough, wheezing, and, in extreme cases, bronchiolitis or pneumonia.
- Incubation time: Human metapneumovirus (HMPV) spreads from person to person through respiratory droplets. The incubation time of HMPV lasts 3 to 5 days and varies by individual.
Human metapneumovirus causes
Human metapneumovirus (HMPV) is a main respiratory pathogen that mainly affects children but can cause serious illness in vulnerable people. The causes of HMPV infection are distinct, including the following factors:
- Genetic variability: The virus contains different genetic lineages (A and B), with differences that may affect transmission dynamics and infection rates in different populations.
- Zoonotic origins: HMPV is likely to have evolved from avian metapneumoviruses, implying that a zoonotic transmission from birds to humans could be the origin of infection.
- Environmental factors: The virus spreads more frequently during winter and early spring, overlapping with other respiratory infections, which enables its transmission in crowded indoor environments.
- Viral transmission: HMPV is mainly transmitted through respiratory droplets from infected people, especially in close contact situations.
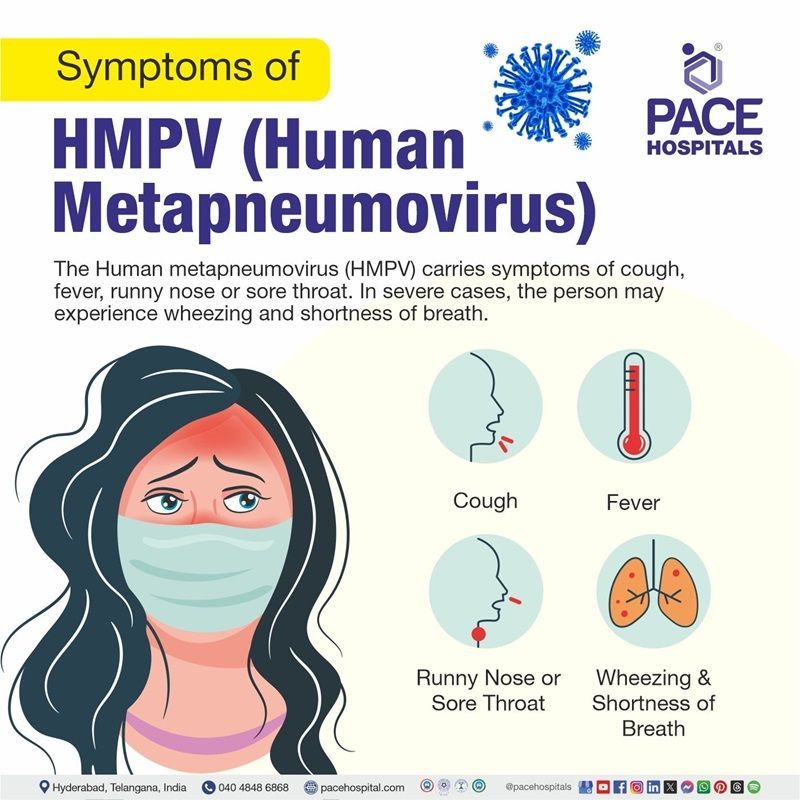
Human metapneumovirus symptoms
In general, clinical criteria alone cannot distinguish HMPV infection from other respiratory viruses. Human metapneumovirus can cause either upper or lower respiratory tract infection.
Adult patients with an HMPV infection may be asymptomatic or present with symptoms ranging from mild upper respiratory tract infections to severe pneumonia.
Symptoms of upper respiratory tract infections
- Cough
- Rhinorrhoea (Runny nose)
- Nasal congestion (Stuffy nose)
- Sore throat
Symptoms of lower respiratory tract infections
- Fever
- Wheezing
- Dyspnoea (shortness of breath)
- Hypoxia (low oxygen levels in body tissues)
- Hoarseness
- Purulent cough
Severe symptoms of HMPV
- Pneumonia
- Bronchiolitis
- Asthma
- COPD (chronic obstructive pulmonary disease) exacerbation
Gastrointestinal symptoms of HMPV
- Nausea
- Vomiting
- Diarrhoea
- Otitis media
Human metapneumovirus risk factors
Several risk factors can increase the occurrence of severe HMPV disease. They include the following:
Modifiable risk factors for human metapneumovirus (HMPV)
These factors can be changed or regulated to decrease the possibility of HMPV infection or severity. The main modifiable risk factors include:
- Exposure to tobacco smoke: Environmental tobacco smoke has been responsible for an increase in respiratory diseases, including HMPV, which emphasizes the need of smoke-free surroundings.
- Household crowding: Increased exposure in crowded living environments may contribute to the spread of HMPV, particularly among children and individuals at risk.
Non-modifiable risk factors for human metapneumovirus (HMPV)
Non-modifiable risk factors are innate characteristics that cannot be altered but influence a person's risk of HMPV. They include:
- Age: Infants under the age of six months, as well as older individuals with weakened immune systems, are significantly more likely to develop severe HMPV illness.
- Premature birth: Because of their immature lungs and immune systems, prematurely born children are more susceptible to severe HMPV symptoms.
- Comorbidities: Individuals with pre-existing medical conditions, such as chronic respiratory diseases or immunosuppression, heart or neural disorders, are more likely to develop serious illness from HMPV.
- Immunocompromised individuals: Patients with weaker immune systems, such as those people undergoing
chemotherapy or organ transplantation, have an increased risk of severe symptoms.
Human metapneumovirus complications
In certain patient populations, HMPV may result in serious illnesses necessitating hospitalization. The following are the complications associated with HMPV:
- Bronchiolitis: HMPV is the most common cause of bronchiolitis in children, accounting for nearly 65.7% of hospitalized pediatric patients. It is most common in newborns and young children, frequently necessitating hospitalization for respiratory assistance.
- Pneumonia: The virus can also lead to pneumonia, which occurs in approximately 14.3% of cases among children infected primarily with HMPV. This condition frequently requires medical attention and can cause considerable morbidity.
- Respiratory distress and ICU Admission: Severe respiratory distress is typical among hospitalized children with HMPV, with a significant proportion necessitating admission to pediatric intensive care units. Some individuals may require mechanical ventilators or other advanced respiratory assistance.
- Acute respiratory distress syndrome (ARDS) and multiorgan failure: In critical cases, HMPV infection can cause ARDS and multiorgan failure, particularly in children with previous medical conditions or immunocompromised adults.
- Acute asthma exacerbations: HMPV infection has been linked to asthma exacerbations, which occur in patients after infection. This can lead to higher morbidity in people with pre existing asthma problems.
Human metapneumovirus diagnosis
HMPV identification does not require confirmatory tests and is typically based on a clinical diagnosis. However, there are laboratory tests that can be used. Below are the steps involved in diagnosing HMPV:
- Clinical evaluation
- Medical history
- Physical examination
- Laboratory testing
- Swab tests
- Nucleic acid amplification tests (NAAT)- Reverse transcriptase-polymerase chain reaction (RT-PCR)
- Antigen detection tests- Immunofluorescence assays and enzyme-linked immunosorbent assays (ELISAs) and direct immunofluorescent-antibody (IFA) test
- Blood tests: Complete blood counts (CBC) and inflammatory markers
- Serological tests
- Imaging tests
- Chest X-ray or CT scans
- Advanced procedures
- Bronchoscopy
Human metapneumovirus treatment
Human Metapneumovirus (HMPV) treatment is mostly supportive, as there are presently no FDA-approved antiviral drugs particularly for this virus. The management options used may differ on the basis of the severity of the infection and the patient's overall condition. The following are the main steps involved in treating HMPV:
- Supportive measures
- Intravenous fluid hydration
- Supplemental oxygen support for hypoxemia via high flow nasal cannula or even mechanical ventilation
- Symptomatic management
- Anti-pyretic medications
- Bronchodilators
- Corticosteroids
- Antibiotics for secondary infections
- Antiviral medications
- Ribavirin: Although it is not approved specifically for HMPV infection, ribavirin has shown efficacy in some cases, mainly in immunocompromised patients
- Intravenous Immunoglobulin (IVIG)
- Experimental therapies
- Monoclonal antibodies
- Fusion Inhibitors and RNA Interference
Human metapneumovirus prevention
The vaccine for HMPV is currently unavailable. People are advised to practice appropriate personal and environmental hygiene to limit the risk of illness. Below are some of the preventive measures for HMPV:
Maintaining good hygiene
- Wearing a mask properly, including hand cleanliness before and after use, is essential.
- Hand hygiene should be practiced regularly, especially before touching one's eyes, mouth, nose; before eating; after using the restroom; after touching public facilities such as handrails or doorknobs; or when hands are contaminated with respiratory secretions from coughing or sneezing.
- When people sneeze or cough, they need to cover their nose and mouth with a tissue paper. They need to throw soiled tissues in a lidded trash bin, then thoroughly wash their hands.
- When experiencing respiratory symptoms, people need to use a surgical mask, stop working or attending school, avoid crowded places, and seek medical attention immediately.
- People must build up their bodies' immunity by eating a balanced diet, exercising regularly, getting enough rest, quitting smoking, and avoiding alcohol.
- Infected individuals are advised to avoid contact with children, older adults, and others with weakened immune systems.
- Individuals are advised to rub both hands with water and liquid soap for at least 20 seconds. Next, rinse with water and dry with a disposable paper towel or hand dryer. If hand washing facilities are unavailable or the hands are not visibly filthy, hand hygiene with 70 to 80% alcohol-based hand rub is an effective solution.
Maintain good environmental hygiene
- Cleaning and disinfecting, eating and drinking utensils after use can help to minimize the transmission of disease.
- Maintaining proper interior ventilation. Avoid crowded or poorly ventilated public settings; high-risk persons are advised to consider using surgical masks.
- Cleaning and disinfecting frequently touched surfaces like furniture, toys, and commonly shared items regularly with household bleach.
- Cleaning away obvious pollutants like respiratory secretions with absorbent disposable towels.
Difference between HMPV and COVID
HMPV VS COVID
Though both HMPV and
COVID primarily attack the respiratory system, these two viral infections are completely different in terms of severity and fatality. Both viruses transmit through respiratory droplets and contact with infected surfaces. Below are the parameters that help in differentiating HMPV and COVID:
| Parameters | Human Metapneumovirus (HMPV) | COVID |
|---|---|---|
| Virus family | Pneumoviridae | Coronaviridae |
| Symptoms | Cough, fever, wheezing, nasal congestion and shortness of breath. | Fever, shortness of breath, cough, tiredness, loss of taste and smell. |
| Seasonality | Typically, it happens in late winter and early spring. | Year-round transmission with several waves |
| Transmission | Primarily by respiratory droplets and touch. | Mainly by respiratory droplets and contact. |
| Affected people | Primarily affects small children, older people, and immunocompromised people. | Affects all age groups, with greater severity in older persons and those with comorbidities. |
| Mortality risk | In general, mortality risk is lower and considerable in vulnerable populations. | Increased mortality risk, particularly among older people and those with comorbidities. |
| Treatment | Supportive treatment | Antivirals and supportive care |
| Vaccination | No vaccine available | Effective vaccines are available |
Frequently Asked Questions (FAQs) on Human metapneumovirus (HMPV)
What isolation is needed for metapneumovirus?
Metapneumovirus (HMPV) is primarily transmitted through respiratory droplets, so patients should be isolated in a single room with contact and droplet precautions. Infection control measures similar to those implemented for RSV infections should be taken, including wearing masks, gowns and gloves when in contact with the patient and maintaining good hand hygiene until clinical recovery.
What is the mortality rate for HMPV?
The mortality rate for human metapneumovirus (HMPV) is generally low but varies with the infection's severity and the patient's health. While healthy individuals typically experience mild infections, high-risk groups—such as the elderly, young children, and immunocompromised individuals, may face higher mortality rates. Crude mortality rates for HMPV pneumonia can range from 10% to 80% in small studies of patients with cancer or those who have had hematopoietic cell transplantation (HCT).
How serious is HMPV?
Human metapneumovirus (HMPV) typically causes mild cold-like symptoms in healthy individuals but can be serious for vulnerable populations. It accounts for 6% to 12% of exacerbations in chronic obstructive pulmonary disease (COPD) cases. In immunocompromised patients, HMPV can lead to severe lower respiratory tract diseases, with mortality rates between 10% and 80%. In children, it can cause bronchiolitis and pneumonia, leading to 5% to 10% of hospitalizations for acute respiratory infections.
What are the precautions for human metapneumovirus?
To prevent the spread of human metapneumovirus (HMPV), wearing a mask, avoiding touching the face, and covering coughs and sneezes is helpful. Staying away from sick individuals and practicing good hand hygiene while regularly disinfecting surfaces is also essential to prevent human metapneumovirus (HMPV).
Is there a vaccine for human metapneumovirus?
Soon after its discovery in 2001, HMPV was quickly recognized as a common cause of lower respiratory tract infections in immunocompromised patients, young children, and older adults. Although HMPV is a clinically significant pathogen, no vaccine is currently available.
How is human metapneumovirus treated?
There are currently no antiviral medications available that specifically treat human metapneumovirus. However, this HMPV virus is typically treated with supportive care, including rest, hydration, and over the counter medications to relieve symptoms such as fever and congestion. In severe cases, such as in immunocompromised individuals or those with respiratory distress, oxygen therapy or mechanical ventilation may be required.
Is human metapneumovirus just a cold?
Human metapneumovirus (HMPV) can cause symptoms similar to a common cold, such as cough, congestion, and sore throat. However, it can also lead to more severe respiratory illnesses like bronchiolitis, pneumonia, or asthma exacerbations, especially in young children, the elderly (adults over 65), people with breathing problems and immunocompromised individuals. While often mild, it can be more serious in vulnerable populations.
How long does a fever last with HMPV?
The average duration of fever in cases positive for human metapneumovirus (HMPV) is approximately 10 days, reaching its peak during the illness. Young adults who experience re-infection with HMPV typically show mild cold and flu-like symptoms, with fever occurring in a small percentage of those infected.
Is human metapneumovirus the same as RSV?
Human metapneumovirus (HMPV) and respiratory syncytial virus (RSV) are both respiratory viruses. HMPV belongs to the same genus as RSV (Pneumovirus) and can cause similar symptoms such as cough, fever, and wheezing. However, the highest risk for severe illness from HMPV occurs between 6 and 12 months, while RSV is more capable of causing severe illness in infants under 6 months.
Do you need antibiotics for human metapneumovirus?
No. Antibiotics only treat bacteria. Since HMPV is a virus, antibiotics won't work. However, some patients who develop pneumonia from HMPV may also experience a bacterial infection simultaneously (secondary bacterial infection). If a healthcare professional prescribes antibiotics, it will be to treat any secondary infections.
Yes, it is possible to get human metapneumovirus (HMPV) more than once. Immunity after an infection may not be long-lasting, and re-infection can occur, especially since the virus has multiple strains.
Human Metapneumovirus (HMPV) is typically diagnosed using RT-PCR (Reverse Transcription Polymerase Chain Reaction). This is the most common and accurate method for diagnosing HMPV infection.
HMPV RT-PCR test is a sensitive technique that detects the virus's genetic material (RNA) within respiratory samples such as nasal swabs, throat swabs, or sputum.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Hafeezpet, Madeenaguda, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc).

CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
FOLLOW US
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital near me.