Hydrocele - Types, Symptoms, Causes, Risk factors, Treatment and Prevention
Pace Hospitals
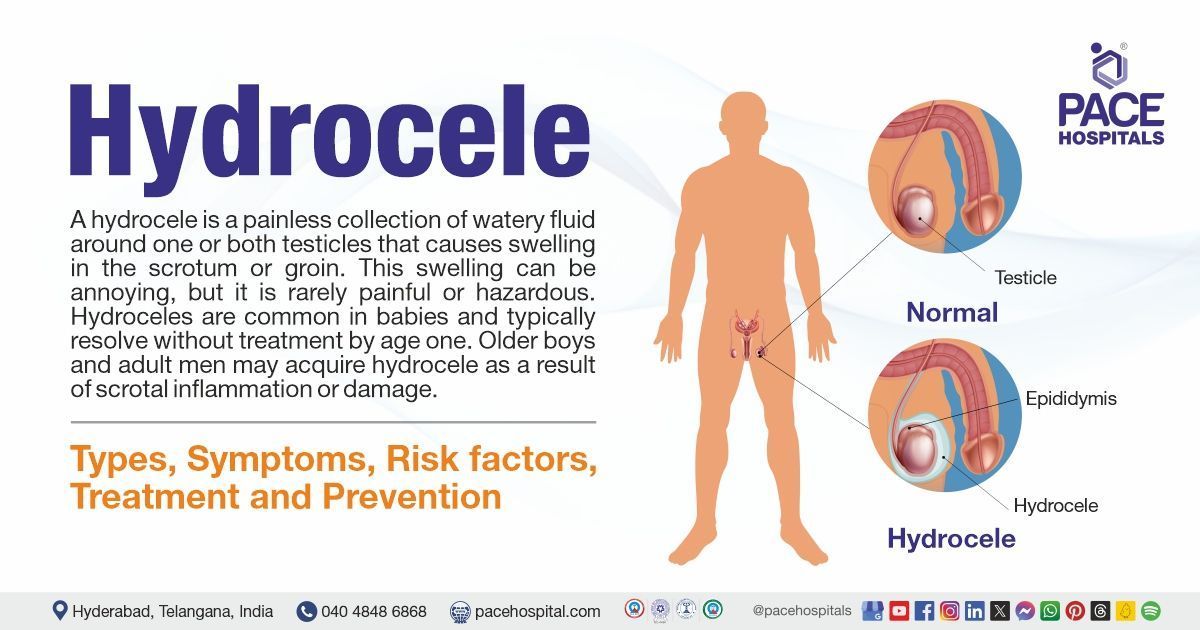
Hydrocele definition
A hydrocele is a condition characterized by a collection of fluid in the scrotum. This condition often makes the scrotum look large or inflamed (swollen). A hydrocele can occur on either one side or both sides of the scrotum. Hydroceles result from an imbalance in the secretion and reabsorption of fluid from the tunica vaginalis (a sac around the epididymis and testis).
Hydrocele can be treated by
urologists or andrologists who are experts in the field.
Hydrocele meaning
The term "hydrocele" is derived from the Greek words “hydōr” which means water and kēlē which means tumour (swelling). The word was first used in the late 1500s.
Hydrocele Prevalence
Prevalence of hydrocele worldwide
Hydrocele affects approximately 1% of adult males. More than 80% of newborn boys have a patent processus vaginalis (an unusual gap that separates the scrotum from the peritoneal cavity), but the majority close spontaneously by 1.6 years of age.
The incidence of hydrocele is rising with the increased survival rate of premature infants and the increasing usage of the peritoneal cavity for ventriculoperitoneal (VP) shunts, dialysis, and kidney transplants.
Most hydroceles are congenital (inborn) and appear in children around 1-2 years old. Chronic or secondary hydroceles most commonly affect men over the age of 40 years. Noncommunicating hydroceles are the most frequent kind of hydrocele worldwide, affecting about 3 crore men and boys.
The World Health Organisation (WHO) estimates that 2.5 crore males globally have hydrocele due to filariasis (filarial hydrocele). The most prevalent cause of hydrocele in adults worldwide is filariasis, a parasite infection caused by Wuchereria bancrofti. Filariasis affected more than 9 crore individuals across 52 nations.
Prevalence of hydrocele in India
Hydrocele is a common condition in India, accounting for about 1.26 lakh recorded cases according to 2023 data. In 2009, a study indicated that India accounted for 48% of the world's 2.67 crore hydrocele cases.

Types of Hydrocele
Hydroceles are categorized into two types they are:
- Primary hydrocele
- Secondary hydrocele
Primary hydrocele occurs when the spermatic cord's processus vaginalis merges at term (full term pregnancy) or within 1–2 years after birth, cutting off communication between the abdomen and the scrotum.
Primary hydrocele types
Primary hydrocele is subcategorized into 4 types of hydrocele, which include:
- Congenital hydrocele
- Infantile hydrocele
- Encysted hydrocele
- Vaginal hydrocele (primary vaginal hydrocele)
Congenital hydrocele: Congenital hydrocele at birth develops when the processus vaginalis connects with the peritoneal cavity.
Infantile hydrocele: In this case, the process vaginalis is destroyed at the level of the deep inguinal ring. However, the distal section stays open, allowing fluid buildup.
Encysted hydrocele (encysted hydrocele of cord): Both the proximal and distal sections of the processus vaginalis get destroyed, while the middle portion remains patent and fluid accumulates within it.
Vaginal hydrocele (primary vaginal hydrocele): The processus vaginalis remains patent only around the testes, which become impalpable (unable to feel by touch) when fluid accumulates.
Secondary hydrocele
This is frequently caused by an underlying illness, such as infection (filariasis, epididymal TB, syphilis), trauma, post-herniorrhaphy hydrocele, or cancer. This form of hydrocele is typically small, with the exception of secondary hydrocele caused by filariasis, which can be significantly large.
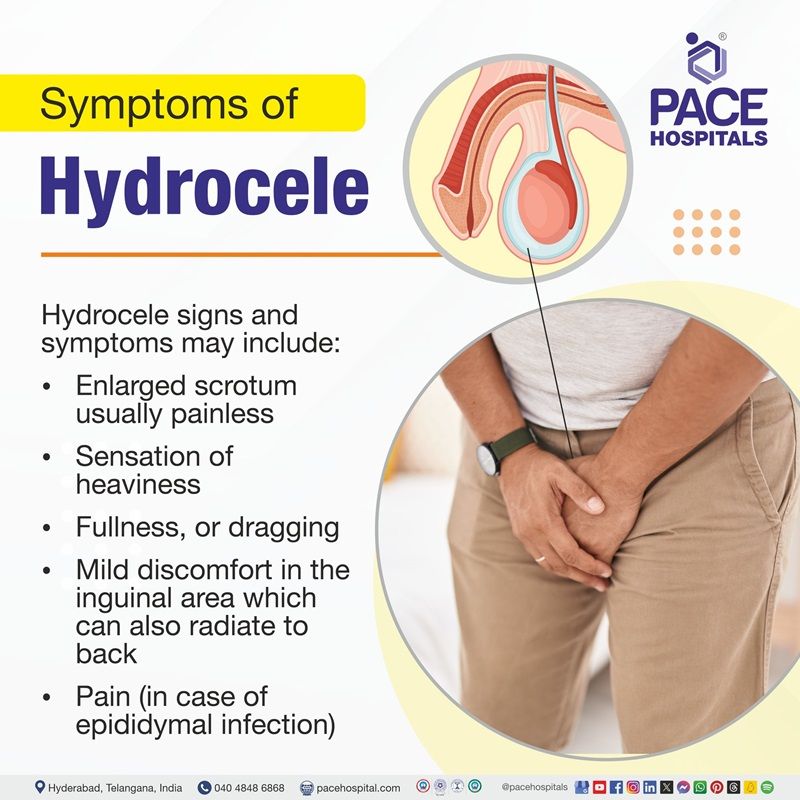
Hydrocele Symptoms
The majority of hydroceles are asymptomatic or subclinical. Even though it is usually painless and not a major health issue, identifying its signs is essential for prompt diagnosis and treatment in order to assist people in recognizing possible symptoms and obtaining the necessary medical guidance.
Hydrocele signs and symptoms may include:
- Enlarged scrotum usually painless
- Sensation of heaviness
- Fullness or dragging
- Mild discomfort in the inguinal area which can also radiate to the back
- Pain (in case of epididymal infection)
Uncomplicated hydrocele does not produce systemic symptoms such as fever, chills, nausea, or vomiting. Uncomplicated hydrocele does not cause genitourinary problems.
Chronically developed hydroceles appear to be larger than acutely developed ones.
Hydrocele Causes
Hydrocele can be congenital (frequent in babies) or acquired (in adults). The underlying causes range from structural difficulties with the processus vaginalis to trauma, infections, and other medical diseases. Understanding these causes is critical for selecting the best treatment options and dealing with potential complications.
Causes of hydrocele in infants
During fetal development, all newborns develop a brief tunnel through the abdominal wall. In boys, this connects the abdominal cavity to the scrotum. In girls, this connects the abdominal cavity to the labia. This tunnel is lined with a thin layer known as the processus vaginalis. This lining is an extension of the one that lines the inside of the abdominal cavity.
The tunnel that connects the abdominal cavity (the belly) to the scrotum has a purpose in boys. During development in the womb, the testicles grow inside the boy's abdomen and then descend through this tunnel to his scrotum. This tunnel and its lining are expected to shut off in both males and females before birth.
At times, when it seals off, some fluid becomes trapped around the testicles in the scrotum. This trapped fluid is known as a noncommunicating hydrocele. Sometimes the tunnel closes, but not fully. As a result, fluid can sometimes trickle down and build in the scrotum, making it appear larger, while it can also drain back into the abdominal cavity, making the scrotum appear normal. This is known as a communicating hydrocele because there is still a tunnel "communicating" between the abdomen and the scrotum.
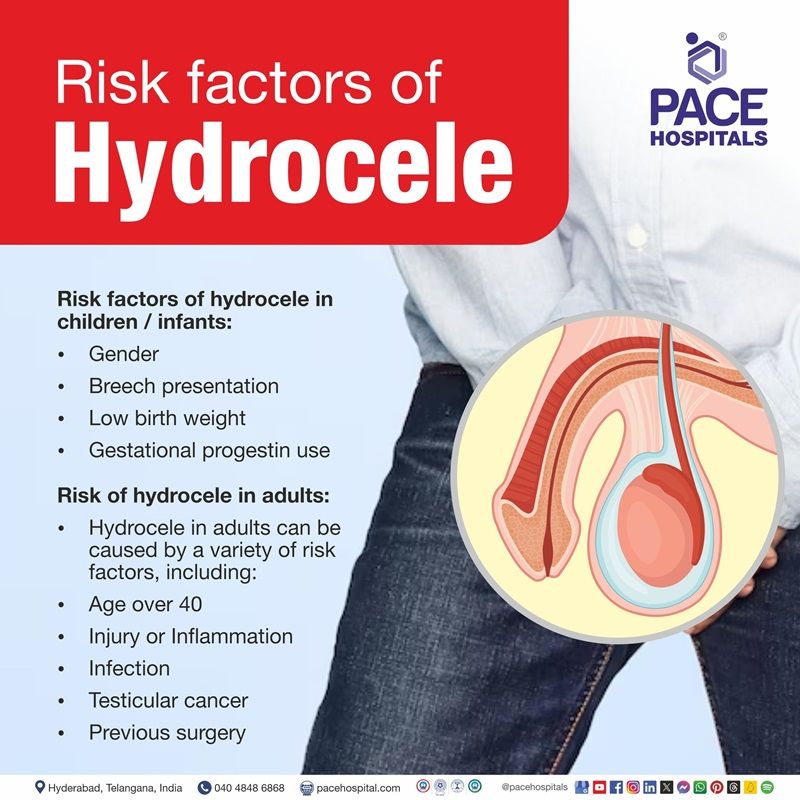
Hydrocele Risk Factors
Risk factors of hydrocele in children/ infants
Hydrocele is a common disorder in newborns, particularly newborn boys, characterized by fluid buildup in the sac enclosing the testicles. Understanding the risk factors related to hydroceles in babies is critical for early detection and management. Risk factors of hydrocele in children include:
- Gender: Hydroceles are much more prevalent in males than females.
- Breech presentation: Studies indicate that breech presentation is associated with an increased risk of hydrocele in neonates. Breech presentation is characterized when a fetus is positioned with the buttocks or feet pointing towards the birth canal rather than the head.
- Low birth weight: Low birth weight can increase the chance of developing a hydrocele by leaving the space between the abdomen and the scrotum open after birth.
- Gestational progestin use: Gestational progestin use can be a risk factor for causing hydrocele by preventing the closure of the processus vaginalis completely.
Risk of hydrocele in adults
Hydrocele in adults can be caused by a variety of risk factors, including:
- Age over 40: The majority of hydroceles occur in adults, particularly in men over the age of 40.
- Injury or Inflammation: A hydrocele can arise as a result of an injury. It may also form as a result of scrotal swelling, known as inflammation.
- Infection: An infection in the testicle, such as filariasis, or the coiled tube at the back of the testicle, can cause inflammation, leading to a hydrocele.
- Testicular cancer: According to the research, testicular/para testicular cancer may develop hydrocele testis as an accompanying symptom.
- Previous surgery:
In men after laparoscopic or transplant surgery, inadequate aspiration of irrigation fluid may induce hydroceles in individuals with a patent processus vaginalis or a minor hernia.
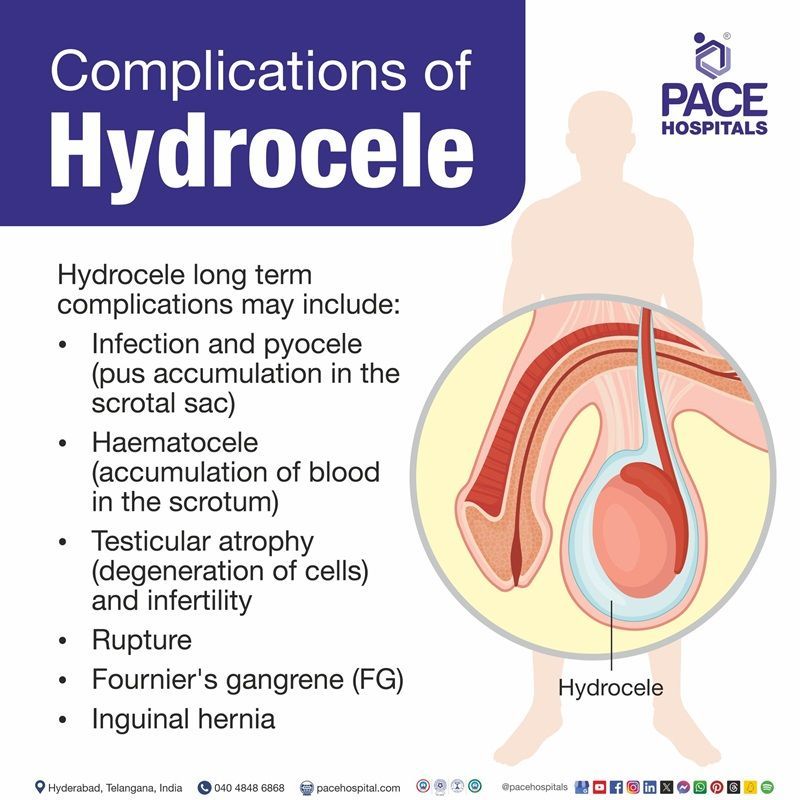
Hydrocele Complications
Hydrocele is usually a benign illness and can lead to a number of complications if left untreated. Understanding the complications is critical for timely intervention and management.
Hydrocele long term complications may include:
- Infection and pyocele (pus accumulation in the scrotal sac)
- Haematocele (accumulation of blood in the scrotum)
- Testicular atrophy (degeneration of cells) and infertility
- Rupture
- Fournier's gangrene (FG)
- Inguinal hernia
Infection and pyocele: Infections can arise if the fluid within the hydrocele becomes infected, leading to a pyocele, which is defined by pus collection. This condition necessitates quick treatment to prevent irreparable damage.
Haematocele: Trauma or injury to the scrotum can cause bleeding into the hydrocele sac, which leads to a haematocele. If not drained, this condition might deteriorate and require immediate medical intervention.
Testicular atrophy (degeneration of cells) and infertility: Large hydroceles often block blood flow to the testis. This can induce testicular atrophy (a decrease in size of a tissue or organ caused by cellular shrinkage) and ultimately lead to infertility in men.
Rupture:
Fluid collection can cause pressure within the scrotum to rise over time, potentially resulting in a rupture. This can cause severe discomfort and may necessitate surgical intervention to resolve the problem.
Fournier's gangrene (FG): Fournier's gangrene (FG) can develop following an infected hydrocele. FG is a potentially fatal infection that can affect the genital and perineal areas. To avoid possible serious consequences, it is critical to get a diagnosis and treatment as soon as possible.
Inguinal hernia:
A hydrocele may be accompanied by an inguinal hernia, which carries additional risks and challenges if not treated.
Hydrocele Diagnosis
Diagnostic evaluation of hydrocele in infants/children
Most hydroceles are identified by recognizing the scrotum's unusual size. Parents or caretakers may be the first to detect the hydrocele, although it is usually recognized by a pediatrician or another general physician. In older children, the patient may be the first to notice that something is not right. The patient is referred to a surgeon when a hydrocele is suspected, the surgeon confirms the diagnosis and discusses treatment options with the family.
When the baby is taken to the doctor, he/she may perform a physical examination. The doctor will also examine the scrotum for fluid and pain and shine a light through it to see if there is fluid around the baby’s testicle.
The doctor will also check to see whether the child has a hernia. The infant may also get a blood test and an ultrasound to ensure that nothing else is causing the swelling.
Diagnostic evaluation of hydrocele in adults
Patients may initially visit a general physician with hydrocele pain and swelling. The general physician then refers the patient to a urologist/andrologist for further evaluation and management. Diagnostic evaluation of hydrocele is done using:
- Physical examination
- Laboratory tests
- Imaging tests
Physical Examination
- The urologist/andrologist will assess for pain and press on the belly and groin to rule out an inguinal hernia.
- Hydrocele transillumination test: Transillumination test for hydrocele involves a light that is directed through the scrotum to see the clear fluid surrounding the testicle.
Laboratory tests
Blood and urine tests are advised in order to rule out the infectious causes of hydrocele
Imaging tests
Imaging tests may be used to detect hernias, tumors, and other causes of scrotal (scrotum) enlargement.
Imaging tests that are used may include:
- Ultrasonography
- Duplex ultrasonography
- Plain abdominal radiography
- Computed tomography
Hydrocele Treatment
Hydrocele treatment for children
During the first consultation, the surgeon will examine the child's health, confirm the presence of a hydrocele, and determine whether any additional testing is required prior to the surgery. During the consultation, the surgeon will go over the risks, benefits, alternatives, outcomes, and problems of each treatment choice.
If the child has a hydrocele that needs to be repaired, hydrocele repair surgery will be scheduled. These operations are typically performed as outpatient procedures, which means the patient comes in and goes home on the same day. This technique is carried out under general anesthesia in pediatric patients.
Adult hydrocele treatment
Hydrocele Surgery is the preferred treatment for hydrocele and is recommended when the condition becomes serious or bothering. Hydroceles caused by an inguinal hernia should be surgically repaired as soon as possible. Hydroceles that do not resolve on their own after a few months may require surgery.
Simple hydroceles in children commonly resolve without surgery. Hydroceles in adulthood rarely resolve on their own. If surgery (hydrocele operation) is required, it is a simple procedure with highly favorable outcomes.
Types of hydrocele operations (surgeries) that are used to manage hydrocele include:
- Hydrocelectomy (open surgery)
- Hydrocelectomy with plication
- Hydrocelectomy with excision
Hydrocele treatment without surgery
Aspiration and Sclerotherapy
Aspiration and sclerotherapy are minimally invasive techniques that treat symptomatic hydroceles and cysts by emptying fluid and injecting a solution to scar the inner lining of the cyst or hydroceles.
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Prevention of Hydrocele
Hydroceles are not usually preventive, but there are some strategies that one can follow to lower the chances of acquiring hydrocele:
- Protecting testicles: Wearing an athletic cup or jockstrap may help when playing sports or engaging in other activities that may cause injury to the testicles.
- Treating infections: Immediate treatment of any infections or inflammation may help to prevent complications related to the testicles (hydrocele).
- Practicing good hygiene: Maintaining good hygiene may help to prevent infections that eventually prevent the complications related to infection.
- Examining the testicles: Checking the testicles on a regular basis for swelling and unexpected changes may help in early detection and timely management of hydrocele.
Hydroceles in infants are usually caused due to congenital defects and are unable to prevent.
Difference between Hernia and Hydrocele
Hernia vs Hydrocele
Hydroceles and hernias are the two distinct disorders that can cause swelling in the groin or scrotum, but their causes and symptoms differ. The table below contains the key differences between hydrocele and hernia.
| Feature | Hernia | Hydrocele |
|---|---|---|
| Definition | An organ protruding through a weak area in the abdominal wall | Accumulation of fluid in the scrotum |
| Location | Can occur at any place in the body ex: groin, abdomen | Confined to the scrotal sac |
| Symptoms | Pain may occur when lifting or straining | Generally painless swelling of the scrotum |
| Transillumination | Negative (solid mass does not transmit light) | Positive (light passes through fluid) |
| Reduction | Usually requires surgical management to resolve the issue | Fluid may be aspirated or resolved on its own |
| Age group | Can occur at any age, most common in adults | Common in infants and young children |
Difference between Hydrocele and Varicocele
Hydrocele vs varicocele
Varicocele and hydrocele are both scrotal diseases, however, they are very different in nature and implications. The key differences between hydrocele and varicocele are listed below.
| Feature | Hydrocele | Varicocele |
|---|---|---|
| Definition | Collection of fluid in the scrotal sac | Enlargement of veins within the scrotum (pampiniform plexus) |
| Cause | The cause is generally unknown, but often occurs due to infection and injuries | Caused by defective valves in the veins, leading to inadequate blood flow. |
| Symptoms | Typically manifests as a painless swelling | May induce a dull discomfort or heaviness in the scrotum, which often worsens upon standing. |
| Appearance | Smooth, soft, and fluid-filled scrotal mass | Feels like a "bag of worms" due to enlarged veins |
| Impact on fertility | Generally, does not affect fertility | Impaired blood flow and temperature regulation can lead to reduced fertility. |
| Treatment | May require aspiration or surgery if symptomatic | Often treated with surgery (varicocelectomy) if symptomatic or affecting fertility |
Frequently Asked Questions (FAQs) on Hydrocele
Can hydrocele cause infertility?
In most cases, hydroceles do not directly cause infertility, although they can have an impact on fertility. Over the course of this condition, the sperm concentration may be affected and may also impose a significant impact on sexual health if left untreated.
Does hydrocele cause erectile dysfunction?
Research indicates that, though hydroceles normally present as a painless lump (mass), they can develop into psychological issues that cause sexual dysfunction. Married males with hydrocele were more likely to experience sexual dysfunction, including a decrease in sexual desire and trouble becoming tumescent (getting erections).
What are the symptoms of hydrocele in children?
The only indication that may be noticed in children is that one or both of the child’s testicles may get enlarged. Even if the swelling doesn’t cause any pain to the child, the child has to be taken to a pediatrician or another qualified healthcare professional to rule out the cause, such as an infection, a tumor, or a hernia.
Is a hydrocele dangerous?
No, a hydrocele is usually not dangerous and does not affect the testicles. However, if a hydrocele is large enough to cause discomfort or pain, or if it is related to an underlying causes, it may need to be addressed.
Can a woman have a hydrocele?
Yes. Hydrocele of the canal of nuck, also known as a female hydrocele, is an extremely unusual complication of an anatomical defect caused by a patent processus vaginalis in females. Historically, it was more common in pediatric patients, but with improved awareness, more adult diagnoses have been made.
Can hydrocele cause testicular atrophy?
Yes. A hydrocele is a fluid-filled enlargement in the scrotum that can compress the testicles and reduce blood flow. This can cause testicular atrophy, which is the shrinking of the testicles.
Can hydrocele cause low testosterone levels?
Hydroceles normally do not alter testosterone levels or the testicle's ability to make testosterone. However, if not treated, sperm concentration and motility can be affected.
What are bilateral hydroceles?
Bilateral hydrocele is a disorder in which fluid accumulates around both testicles, causing swelling in the scrotum. Bilateral hydroceles are frequently idiopathic (unknown cause) in nature, however they can also be related to inflammation, infection, testicular torsion, or cancer.
What is funicular hydrocele?
Funicular hydrocele is a rare disorder in which the processus vaginalis fails to seal properly, resulting in a fluid-filled sac surrounding the testicle. The funicular hydrocele has two variations: the encysted variant, which is not related to the peritoneal cavity, and the funicular form, which is associated with the peritoneal cavity.
Can hydrocele be treated without surgery?
Yes, a hydrocele can be managed without surgery in certain cases by aspiration and sclerotherapy. Aspiration and sclerotherapy are two minimally invasive procedures that treat fluid-filled cysts by emptying the fluid and injecting a solution to scar the cyst lining.
What happens if hydrocele is not treated?
If left untreated, hydrocele can lead to many complications such as inguinal hernia, testicular atrophy (cell degeneration) infertility, and rupture, etc.
Can hernia cause hydrocele?
Yes, a hernia can lead to a hydrocele, specifically Inguinal hernias, can cause the formation of a communicating hydrocele. This occurs when the channel through which the hernia protrudes stays open, allowing fluid from the abdominal cavity to leak into the scrotum and surround the testicle.
What is the best treatment for hydrocele?
Surgery is the preferred treatment for hydrocele and is recommended when the condition becomes serious or annoying. Herniotomy is performed on congenital hydroceles that do not resolve naturally. Acquired hydroceles, on the other hand, go away once the primary underlying problem is treated.
Can a man live with hydrocele?
Most of the time, a hydrocele causes no pain or harm. however, if the scrotum appears swollen, and causes annoying symptoms, it is highly recommended to consult a health care expert.
When to See a Doctor for Hydrocele?
A disorder known as a hydrocele occurs when fluid builds up around the testicle, resulting in scrotal enlargement. Early on, it is frequently painless and can go unnoticed. However, it can develop and become uncomfortable if treatment is not received.
Key warning symptoms:
- Painless scrotal swelling
- Feeling of heaviness or discomfort
- Increase in swelling over time.
- Pain or tightness in the scrotum
If these symptoms persist or worsen, see a hydrocele specialist or urologist. Early diagnosis and timely treatment can relieve discomfort and prevent complications.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles