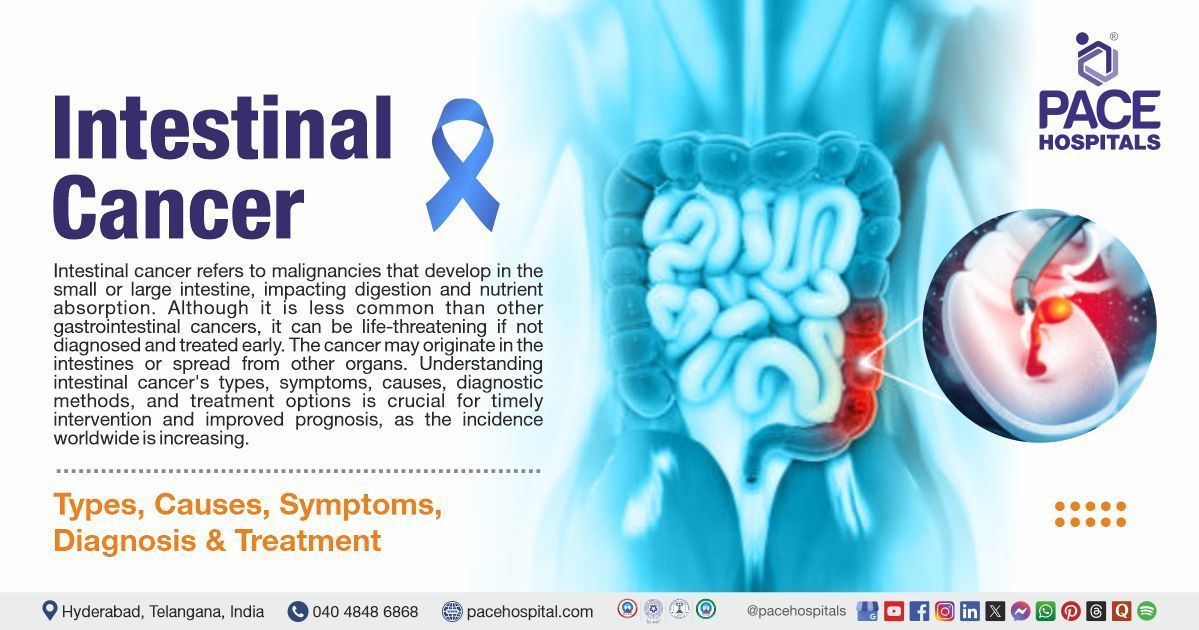
Intestinal Cancer: Types, Symptoms, Causes, Diagnosis & Treatment
Intestinal cancer refers to malignancies that develop in the small or large intestine, impacting digestion and nutrient absorption. Although it is less common than other gastrointestinal cancers, it can be life-threatening if not diagnosed and treated early. The cancer may originate in the intestines or spread from other organs. Understanding intestinal cancer's types, symptoms, causes, diagnostic methods, and treatment options is crucial for timely intervention and improved prognosis, as its incidence worldwide is increasing.

Types of Intestinal Cancer
Intestinal cancers are classified primarily based on their location and the cellular origin of cancerous tumor. some of the prominent types of intestinal cancer include:
Small Intestinal Cancer
This type is relatively rare and affects the small intestine, which includes the duodenum, jejunum, and ileum. The small bowel/ small intestine plays a key role in nutrient absorption, and tumors in this region can lead to severe malnutrition and obstruction. Common subtypes include:
- Adenocarcinoma: Arises from glandular cells, mostly in the duodenum, often associated with inflammatory conditions such as Crohn's disease.
- Neuroendocrine Tumors (Carcinoid Tumors): Slow-growing tumors that often occur in the ileum and secrete hormones that cause systemic symptoms.
- Lymphoma: Affects lymphoid tissue within the intestine, commonly associated with immunosuppressive conditions or infections such as the Epstein-Barr virus.
- Sarcoma (Gastrointestinal Stromal Tumors - GISTs) : Originates in the connective tissue of the intestinal wall and often presents as an abdominal mass with bleeding.
Colorectal Cancer (Large Intestinal Cancer)
This includes malignancies affecting the colon and rectum. Globally, colorectal cancer is one of the most common types of cancer and is influenced by genetic and environmental factors. Common types include:
- Adenocarcinoma: Accounts for over 90% of colorectal cancers and typically develops from pre-existing polyps.
- Lymphoma: Affects lymphoid tissue within the colon, which can lead to severe immune dysfunction.
- Gastrointestinal Stromal Tumors (GISTs): Similar to small intestinal sarcomas and can arise in any part of the digestive tract.
- Neuroendocrine Tumors: Less common but can develop in the colon and rectum, often diagnosed incidentally.
Intestinal Cancer Symptoms
Intestinal cancer, which includes malignancies of the small and large intestines, often presents with subtle or nonspecific symptoms in the early stages, making early detection challenging. The symptoms largely depend on the tumor's location, size, and rate of progression.
Small intestine cancer symptoms
Small intestinal cancer often carries mild symptoms, that are majorly asymptomatic and shows the below symptoms:
- Mild, intermittent abdominal discomfort: Patients may experience vague pain or cramping that is often dismissed as indigestion or gas.
- Changes in bowel habits: This may include occasional constipation, diarrhea, or unexplained fluctuations in stool consistency.
- Mild fatigue and weakness: Chronic low-grade anemia may develop due to occult (hidden) blood loss in stools, leading to early fatigue.
Large intestine cancer symptoms
Large intestinal cancer mostly shows progressive symptoms, that mainly indicate the growth of the tumor and surrounding structure involvement. Some of the large intestinal cancer progressive symptoms are mentioned below:
- Abdominal Pain and Discomfort
- Persistent pain that may be dull, cramping, or colicky.
- Pain intensity may increase over time as the tumor enlarges or causes obstruction.
- Tumors in the small intestine may cause episodic pain that worsens after meals due to partial obstruction.
- Bowel Habit Alterations
- Constipation or Diarrhea: Irregular bowel movements may indicate tumor-related obstruction or irritation.
- Narrowing of stools (pencil-thin stools): Often a sign of a growing tumor in the large intestine causing luminal narrowing.
- Incomplete evacuation: Patients may feel the urge to defecate but pass little stool, which may be associated with rectal or sigmoid colon involvement.
- Rectal Bleeding and Blood in Stool
- Hematochezia (bright red blood in stool): Suggests lower gastrointestinal bleeding, often associated with colorectal tumors.
- Melena (dark, tarry stools): Occurs when bleeding originates higher in the gastrointestinal tract, such as in the small intestine. Chronic blood loss can lead to iron-deficiency anemia, resulting in pallor, fatigue, and dizziness.
- Unexplained Weight Loss
- Cancer-induced hypermetabolism and systemic inflammatory responses contribute to weight loss, however, reduced nutrient absorption, especially in small intestinal cancers, exacerbates malnutrition.
- Fatigue and Weakness
- Chronic bleeding from tumors can cause persistent tiredness due to anemia, systemic inflammation, and increased energy expenditure for cancer treatment, resulting in reduced oxygen-carrying capacity.
- Loss of Appetite and Nutritional Deficiencies
- Tumor-related metabolic alterations can suppress hunger.
- Malabsorption syndromes may occur if the tumor affects the small intestine, thereby leading to deficiencies in essential vitamins and minerals.
- Bloating and Nausea
- Tumors causing partial obstruction can result in bloating and discomfort, particularly after meals.
- Delayed gastric emptying and intestinal motility disturbances can lead to persistent nausea.
- Intestinal Obstruction (Advanced Cases)
- Complete obstruction: Severe abdominal cramping, nausea, vomiting, and the inability to pass stool or gas.
- Bowel perforation (in extreme cases): Can lead to peritonitis, a life-threatening emergency requiring immediate surgery.
Intestinal Cancer Causes
Genetic Factors
- Family History: Individuals with a firs t-degree relative diagnosed with colorectal cancer have a higher risk.
- Inherited Syndromes: Conditions like Lynch syndrome (Hereditary Nonpolyposis Colorectal Cancer, HNPCC) and Familial Adenomatous Polyposis (FAP) significantly increase risk.
- Gene Mutations: Mutations in APC, KRAS, TP53 and SMAD4, as well as mismatch repair (MMR) genes, contribute to tumorigenesis.
Chronic Inflammatory Conditions
- Ulcerative Colitis & Crohn’s Disease: Long-standing inflammation can lead to DNA damage and malignancy.
Dietary & Lifestyle Factors
- High Consumption of Red & Processed Meat: These foods contain Contains carcinogens like heterocyclic amines and polycyclic aromatic hydrocarbons.
- Low Fiber Diet: Fiber promotes bowel motility and reduces exposure to toxins.
- Obesity & Sedentary Lifestyle: These factors Increases inflammation and insulin resistance, promoting cancer growth.
- Smoking & Heavy Alcohol Consumption: Tobacco carcinogens and ethanol metabolism generate DNA-damaging agents.
Metabolic & Microbiome Factors
- Type 2 Diabetes: Hyperinsulinemia and chronic inflammation contribute to tumor progression.
- Gut Microbiome Dysbiosis: Imbalance in gut bacteria, particularly the overgrowth of Fusobacterium nucleatum, promotes inflammation and carcinogenesis.
Environmental & Medical Factors
- Carcinogen Exposure: Prolonged exposure to industrial chemicals, pesticides, or radiation increases the risk.
- Previous Radiation Therapy: Radiation in the abdominal region may damage DNA and trigger cancer.
Early detection through regular screening (such as
colonoscopy, stool tests, genetic testing) is crucial for prevention and better outcomes.
Intestinal cancer diagnosis
Accurate diagnosis is crucial for improving the patient’s prognosis and determining the most effective treatment plan for intestinal cancer. The diagnostic process involves a combination of clinical assessment, advanced imaging, and pathological analysis.
Medical History and Physical Examination
A thorough initial evaluation helps identify risk factors and early symptoms.
- Medical History: A detailed discussion covering persistent symptoms such as unexplained weight loss, changes in bowel habits, abdominal pain, rectal bleeding, and fatigue. Dietary habits and family history of colorectal or gastrointestinal cancers are also assessed.
- Physical Examination: Includes palpation of the abdomen to detect any lumps, tenderness, or organ enlargement. Signs of anemia (such as pale skin and fatigue) may indicate chronic blood loss from a gastrointestinal tumor.
Endoscopic Procedures
Endoscopic techniques allow direct visualization of the intestinal lining, aiding in early detection and biopsy collection.
- Colonoscopy: In this procedure, a colonoscope is inserted into the colon to examine if for polyps, tumors, or abnormal tissue. Biopsies can be taken during the procedure for histopathological evaluation.
- Upper Endoscopy (Esophagogastroduodenoscopy–EGD): Helps visualize the esophagus, stomach, and duodenum. This is particularly useful for detecting small intestinal cancers in the proximal region.
- Capsule Endoscopy: A small, pill-sized camera is swallowed to capture detailed images of the small intestine, which is particularly useful for identifying tumors or obscure gastrointestinal bleeding that other methods may miss.
Imaging Tests
Advanced imaging techniques would help to determine tumor size, location, and potential spread to nearby or distant organs.
- CT Scan (Computed Tomography) and MRI (Magnetic Resonance Imaging): These scans Provides detailed cross-sectional images to assess tumor invasion, lymph node involvement, and distant metastases.
- PET Scan (Positron Emission Tomography): Uses radioactive glucose tracers to detect active cancerous areas, aiding in staging and treatment planning.
- Barium X-ray (Small Bowel Follow-Through): Involves swallowing a barium contrast material, which coats the intestinal lining and highlights abnormalities such as strictures, tumors, or polyps on X-ray imaging.
Biopsy and Pathological Analysis
A biopsy is the gold standard test in confirming an intestinal cancer diagnosis
- Tissue Sample Collection: A small piece of abnormal tissue is obtained during endoscopy, surgery, or image-guided procedures.
- Histopathological Examination: The sample is analyzed under a microscope to identify cancerous cells, determine the cancer subtype (such as adenocarcinoma, or lymphoma, neuroendocrine tumor, etc.), and assess its aggressiveness.
- Molecular and Genetic Testing: Advanced tests like molecular and genetic testing usually done to identify genetic mutations, such as KRAS, BRAF, or MSI (microsatellite instability), which can guide targeted therapy.
Blood Tests
Blood tests usually help in assessing the overall health, understand indirect signs of cancer, and support in treatment response.
- Complete Blood Count (CBC): Identifies anemia, which may result from chronic blood loss due to a gastrointestinal tumor.
Tumor Markers
Some of the tumor markers are as mentioned below
- Carcinoembryonic Antigen (CEA): Elevated levels are seen in colorectal and intestinal cancers making it useful for monitoring treatment response.
- CA 19-9: May be elevated in advanced cases, though it is not specific to intestinal cancer.
Intestinal Cancer Treatment
The treatment of intestinal cancer depends on the type of intestinal cancer, its stage, and the patient’s health. Options include:
- Surgical Treatment: Surgical treatment is one of the primary choice of treatment, especially in case of early diagnosed cancer. Some of the cancer types are:
- Segmental Resection or Colectomy: Removal of the cancerous segment of the intestine.
- Laparoscopic Surgery: Minimally invasive surgery with quicker recovery times and reduced complications.
- Stoma Creation (Colostomy/Ileostomy): Performed in some cases after tumor removal, particularly for rectal cancers.
- Radiation Therapy: Radiation therapy can be given as an adjuvant therapy along with chemotherapy and surgery. Some of the important types are:
- External Beam Radiation: Used in rectal cancer and locally advanced cases.
- Intraoperative Radiation Therapy (IORT): Targets residual cancer cells during surgery.
- Chemotherapy and Targeted Therapy: Systemic
chemotherapy and immunotherapy options, including checkpoint inhibitors are used for advanced-stage cancers.
Intestinal Cancer Survival Rate
The survival rate for intestinal cancer varies based on the type and stage. For small intestine adenocarcinoma, the 5-year survival rate is around 70–80% for localized cases, 50–60% for regional spread, and 10–20% for distant metastases, with an overall survival of 30–40%. Colorectal cancer has a better prognosis, with a 90% survival rate for localized cases, 70% for regional spread, and 15–20% for distant metastases, with an overall survival rate of 65%. Early detection and appropriate treatment significantly improve outcomes.
Frequently Asked Questions (FAQs) on Intestinal Cancer
Is intestinal cancer curable?
Intestinal cancer can be curable if detected early and treated appropriately. Localized cases (confined to the intestine) have high survival rates with surgery, while advanced stages may require chemotherapy, radiation, or targeted therapy. Prognosis depends on the stage, type, and treatment response.
What causes intestinal cancer?
Though the exact cause of intestinal cancer is unknown, but factors such as like genetic mutations, family history, inflammatory bowel diseases (Crohn's disease, ulcerative colitis), smoking, alcohol consumption, high-fat diets, obesity, and exposure to carcinogens are associated with an increased risk. Genetic conditions like Lynch syndrome also elevate the likelihood of developing intestinal cancer.
How is intestinal cancer diagnosed?
Diagnosis of intestinal cancer involves a combination of medical history evaluation, physical examination, endoscopic procedures (colonoscopy, capsule endoscopy), imaging tests (CT, MRI, PET scan), and biopsies. Blood tests, including tumor markers like CEA and CA 19-9, also help assess cancer presence and progression.
Is intestinal cancer hereditary?
Yes, some cases are hereditary. Conditions such as Lynch syndrome, familial adenomatous polyposis (FAP), and Peutz-Jeghers syndrome significantly increase the risk. Individuals with a family history of colorectal or small bowel cancer should undergo genetic counseling and regular screenings.
What is the survival rate of intestinal cancer?
Survival rates differ based on cancer type and stage at diagnosis. Small intestine adenocarcinomas have a 5-year survival rate of 65-75% when localized but drop significantly if metastasized. Colorectal cancer has a 91% survival rate in early stages but declines with advanced disease.
What is intestinal cancer?
Intestinal cancer refers to malignant tumors that develop in the small intestine (small bowel cancer) or large intestine (colon and rectal cancer). It can originate from different cell types, including adenocarcinoma, carcinoid tumors, gastrointestinal stromal tumors (GISTs), and lymphomas. These cancers can block digestion, cause bleeding, and spread to other organs if not treated early.
What are the symptoms of intestinal cancer?
Intestinal cancer symptoms include abdominal pain, bloating, unexplained weight loss, nausea, vomiting, fatigue, blood in stool, black/tarry stools, anemia, changes in bowel habits (diarrhea or constipation), loss of appetite, and obstruction symptoms like severe cramps, vomiting, or an inability to pass stool.
Can ultrasound detect intestinal cancer?
Ultrasound is not the primary imaging tool for detecting intestinal cancer but can help identify masses, obstructions, or fluid buildup. Endoscopic ultrasound (EUS) provides better visualization of tumors in the gastrointestinal tract, while CT scans and colonoscopy are more definitive for diagnosis.
How to prevent small intestinal cancer?
To prevent small intestinal cancer, maintain a healthy diet rich in fruits, vegetables, and fiber while reducing processed meats and red meat. Avoid smoking, limit alcohol, maintain a healthy weight, exercise regularly, and manage underlying conditions like Crohn’s disease or celiac disease.
What are the different types of intestinal cancer?
Intestinal cancer can be classified into several types:
- Adenocarcinoma: The most common type, usually occurring in the small intestine or colon.
- Carcinoid Tumors: Slow-growing neuroendocrine tumors.
- Gastrointestinal Stromal Tumors (GISTs): Arising from the wall of the digestive tract.
- Lymphomas: Cancers of the immune system that develop in the intestine.
Risk factors include age (more common in people over 50), high-fat and low-fiber diets, smoking, excessive alcohol consumption,
inflammatory bowel diseases (IBD) (Crohn's disease, ulcerative colitis), genetic predisposition, obesity, and prior history of polyps or colorectal cancer.
While not entirely preventable, risk reduction strategies include maintaining a high-fiber, low-fat diet, avoiding processed meats, exercising regularly, quitting smoking, limiting alcohol intake, managing inflammatory bowel disease, and undergoing regular screenings, especially for high-risk individuals.
What is the difference between small and large intestinal cancer?
Small intestinal cancer is less common and may include adenocarcinomas, carcinoid tumors, or GISTs. Large intestinal cancer (colorectal cancer) is more frequent and often develops from polyps. The treatment approach and prognosis differ based on tumor location and type.
How do polyps relate to intestinal cancer?
Polyps are abnormal growths in the intestinal lining. While most are benign, some, especially adenomatous polyps, can become cancerous over time. Regular colonoscopies help detect and remove polyps before they turn into malignancies.
How does intestinal cancer spread?
Intestinal cancer can spread locally to nearby tissues, regionally to lymph nodes, or distantly through the bloodstream or lymphatic system, affecting the liver, lungs, peritoneum, and bones. Metastatic cancer requires systemic treatment such as chemotherapy or targeted therapy.
What are the warning signs of advanced intestinal cancer?
Advanced-stage symptoms include severe weight loss, persistent abdominal pain, intestinal obstruction,
jaundice (if the liver is involvement occurs), difficulty swallowing, rectal bleeding, changes in stool shape, and general weakness or extreme fatigue.
How effective is chemotherapy for intestinal cancer?
Chemotherapy is effective, particularly for advanced or metastatic cases. It may be used as neoadjuvant therapy (before surgery) to shrink tumors or adjuvant therapy (after surgery) to eliminate residual cancer cells. Targeted drugs enhance chemotherapy effectiveness in certain patients.
Can diet impact intestinal cancer risk?
Yes, a diet high in fiber (vegetables, fruits, whole grains) and low in processed and red meats reduces the risk. High-fat diets and excessive alcohol consumption are associated with an increased likelihood of developing intestinal cancer. Omega-3 fatty acids may offer protective benefits.
How does Lynch syndrome increase intestinal cancer risk?
Lynch syndrome is a genetic condition due to mutations in DNA mismatch repair genes (MLH1, MSH2, MSH6, PMS2). It increases the risk of colorectal and small bowel cancers, often at an earlier age, requiring regular colonoscopy and genetic screenings.
What role do tumor markers play in intestinal cancer diagnosis?
Tumor markers like CEA (Carcinoembryonic Antigen) and CA 19-9 are used to monitor treatment response and detect recurrence. However, they are not always specific and should be interpreted alongside imaging and biopsy results for accurate diagnosis.
Is robotic surgery beneficial for intestinal cancer?
Yes, robotic-assisted laparoscopic surgery offers minimally invasive tumor removal with greater precision, reduced blood loss, rapid recovery, and fewer complication rates compared to traditional open surgery. It is especially useful in complex cases requiring delicate intestinal reconstructions.
What is the role of immunotherapy in treating intestinal cancer?
Immunotherapy, such as immune checkpoint inhibitors (e.g., pembrolizumab, nivolumab), is effective in patients with microsatellite instability-high (MSI-H) tumors or mismatch repair-deficient (dMMR) cancers. It enhances the immune system's ability to target and destroy cancer cells, offering promising outcomes in select cases.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Hafeezpet, Madeenaguda, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc).

CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
FOLLOW US
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital near me.