Best Pancreaticojejunostomy in Hyderabad, India | Surgery & Cost
PACE Hospitals is a leading hospital for Pancreaticojejunostomy Surgery in Hyderabad, India, offering expert surgical care for chronic pancreatitis, pancreatic duct obstruction, ductal hypertension causing pancreatic dysfunction, severe abdominal pain due to pancreatic duct obstruction. Our highly skilled pancreatic surgeons specialize in minimally invasive and open surgical techniques.
At PACE Hospitals, our team of expert gastroenterology and hepatobiliary surgeons specialize in complex pancreatic surgeries, including Pancreaticojejunostomy, with a strong focus on precision, patient safety, and high success rates, ensures advanced, minimally invasive techniques for better outcomes and faster recovery.
Quick Navigation
• What is Pancreaticojejunostomy?
• When is Pancreaticojejunostomy Needed?
• Different Types of Pancreaticojejunostomy
• Pancreaticojejunostomy: Before & After Surgery
• Key Advantages of Pancreaticojejunostomy
• Life After Pancreaticojejunostomy: What to Expect
• Pancreaticojejunostomy Surgery Cost & factors
Book an appointment for Pancreaticojejunostomy Surgery
Pancreaticojejunostomy procedure appointment
Why Choose PACE Hospitals for Pancreaticojejunostomy Surgery?
State-of-the-art Robotic and Laparoscopic Facilities
Best Pancreatic Surgeons in Hyderabad, India
Precision Complex Pancreatic Surgeries with High Success Rates
Affordable & Cost-effective Treatment Options
What is Pancreaticojejunostomy Surgery?
Pancreaticojejunostomy definition
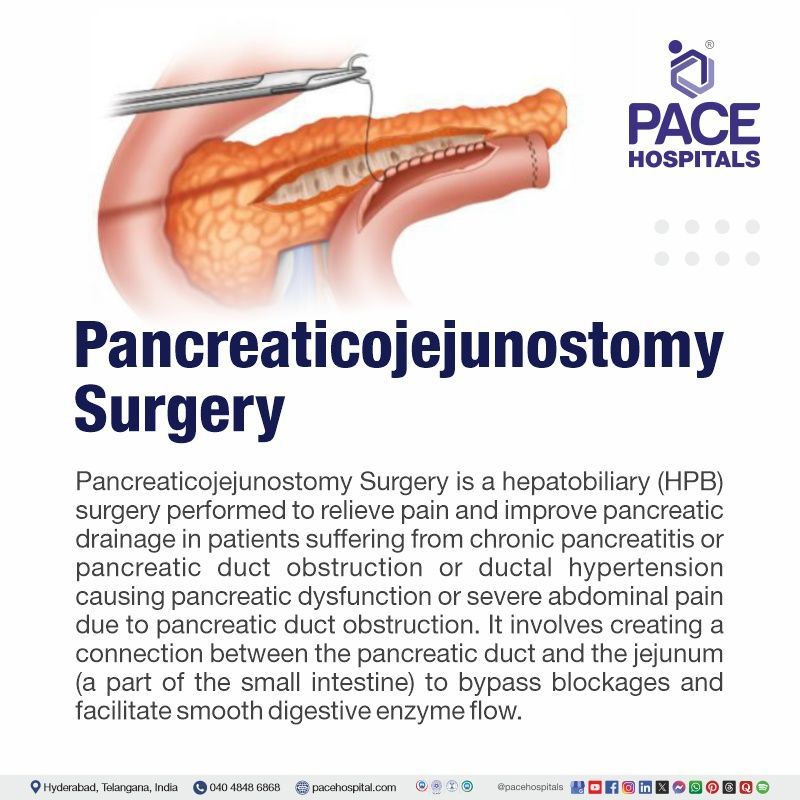
Pancreaticojejunostomy is a surgical procedure that creates an anastomosis between the pancreas and the jejunum to divert pancreatic secretions into the gastrointestinal tract. This procedure is often carried out on individuals with chronic pancreatitis, injuries to the pancreatic duct, or pancreatic cancer. Its purpose is to reinstate normal drainage of enzymes, minimize complications, and maintain pancreatic function, ultimately helping to avert further issues.
Pancreaticojejunostomy is a crucial procedure for treating various pancreatic diseases and complications, especially when the pancreatic duct is damaged, leading to exocrine insufficiency, pain, and sometimes pseudocyst formation.
Pancreaticojejunostomy
Indications
Pancreaticojejunostomy is a procedure that addresses conditions that disrupt the normal function of the pancreas and its ability to secrete digestive enzymes. Some of the major indications are:
- Chronic pancreatitis: Chronic pancreatitis causes obstructed, dilated, or damaged pancreatic ducts, leading to pain and pseudocyst formation. Pancreaticojejunostomy bypasses ducts for normal enzyme drainage.
- Pancreatic duct obstruction: Pancreatic duct obstruction, caused by conditions like strictures, stones, or trauma, can prevent normal enzyme flow and may necessitate surgical intervention for the restoration of its functioning.
- Pancreatic pseudocysts: Pancreaticojejunostomy can reduce pseudocyst formation and infection risk.
- Pancreatic ductal trauma: An anastomosis may be necessary after surgical or traumatic injuries to restore proper pancreatic enzyme flow and reduce complications like fistulas or abscesses.
- Pancreatic cancer: Pancreaticojejunostomy is often used after pancreatic tumor resection, particularly when the pancreatic duct is resected alongside the tumor, often performed as part of surgical treatment after Whipple or distal pancreatectomy.
- Pancreatic cystic lesions: Cystic lesions in the pancreas, especially those affecting the duct system, may require a pancreaticojejunostomy to restore pancreatic drainage and prevent further complications.
- Post-surgical complications: Pancreaticojejunostomy is a salvage procedure used when pancreatic duct damage occurs after other surgeries or when drainage procedures like pancreatic duct stenting fail.
Pancreaticojejunostomy types
Pancreaticojejunostomy involves various techniques, influenced by the underlying pathology, surgeon's preference, and anatomical factors. Some of these techniques are as mentioned below:
Lateral Pancreaticojejunostomy
Lateral pancreaticojejunostomy is a surgical procedure where the side of the pancreas is connected to the jejunum (part of the small intestine) to create an outlet for pancreatic enzymes. It is typically done when other treatments, such as drainage or medical management, are unsuccessful in managing the condition.
Longitudinal Pancreaticojejunostomy (Puestow Procedure)
Longitudinal pancreaticojejunostomy is a surgical procedure where the pancreas is connected to the jejunum along its length. It is typically performed to treat chronic pancreatitis or other pancreatic ductal obstructions. In this procedure, the pancreas is opened longitudinally, and the pancreatic duct is drained into the jejunum to allow pancreatic enzymes to flow directly into the small intestine, improving digestion and alleviating symptoms like pain and malabsorption.
End-to-end pancreaticojejunostomy
This technique involves the direct anastomosis of the pancreatic duct to the jejunum end is less common due to higher risk of stenosis or complications.
Modified blumgart pancreaticojejunostomy
The surgeon may combine end-to-side and end-to-end techniques or use adjunctive procedures like ductal stenting, depending on the patient's specific pathology.
Roux-en-Y pancreaticojejunostomy
The Roux-en-Y loop technique is used for pancreatic anastomosis, providing a stable and controlled environment for pancreatic drainage, particularly in cases of pancreatitis or ductal injury.
Pancreatic duct stenting with jejunostomy
A temporary or permanent stent may be placed in the pancreatic duct before anastomosis to maintain ductal patency in cases of significant dilation.
Differentiation between Lateral Pancreaticojejunostomy (LPJ) and Longitudinal Pancreaticojejunostomy (LPJ)
Lateral vs Longitudinal Pancreaticojejunostomy
Both lateral pancreaticojejunostomy (LPJ) and longitudinal pancreaticojejunostomy (LPJ) are surgical procedures for treating chronic pancreatitis. Lateral PJ is best for patients with pancreatic duct calculus and has a low rate of complications and mortality. whereas Longitudinal PJ is most appropriate for patients with a dilated main pancreatic duct without an inflammatory mass and has lower morbidity and mortality rates.
| Feature | Lateral Pancreaticojejunostomy (LPJ) | Longitudinal Pancreaticojejunostomy (LPJ) |
|---|---|---|
| Indication | Best for patients with pancreatic duct calculi (stones) | Suitable for patients with a dilated main pancreatic duct without an inflammatory mass |
| Surgical Approach | Side-to-side anastomosis between the pancreatic duct and jejunum | Longitudinal incision along the pancreatic duct with jejunal anastomosis |
| Primary Benefit | Effective in relieving pain and improving pancreatic drainage | Reduces ductal pressure and improves pancreatic function |
| Complications | Lower complication rates, but may not be suitable for all cases | Lower morbidity and mortality rates compared to other pancreatic surgeries |
| Mortality Rate | Low mortality rate | Even lower mortality and morbidity rates |
| Patient Suitability | Patients with obstructive pancreatic stones and minimal duct dilation | Patients with chronic pancreatitis and pancreatic duct dilation without an inflammatory mass |
Contraindications for pancreaticojejunostomy
While pancreaticojejunostomy is a versatile procedure, there are certain conditions where it may not be suitable:
- Advanced pancreatic cancer: If pancreatic cancer has spread metastatically to distant organs, a pancreaticojejunostomy may not be suitable and palliative measures may be considered instead.
- Uncontrolled infections: Pancreaticojejunostomy is contraindicated in patients with active, uncontrolled intra-abdominal infections or sepsis until the infection is treated and controlled.
- Severe malnutrition or debilitation: In few cases, complications post-surgery could lead the patient to not be able to consume food for a period, during which the patient undergoes malnutrition.
- Severe ductal stricture: A pancreaticojejunostomy may not be effective in restoring adequate function in cases of extensive fibrosis or stricturing of the pancreatic duct.
- High surgical risk: Patients with high surgical risks due to comorbidities, poor cardiac function, or other complicating factors may not be suitable candidates for this procedure.
Pancreaticojejunostomy procedure
Pancreaticojejunostomy is typically performed under general anesthesia and involves several steps:
- Incision: A surgeon makes an incision to access the pancreas and the duodenum or jejunum, either through the upper abdomen or using a minimally invasive laparoscopic approach.
- Identification of the pancreatic duct: The surgeon meticulously dissects the pancreatic duct, identifying the area of obstruction or injury that requires bypass.
- Jejunum mobilization: The jejunum is moved to the pancreas site for anastomosis, usually after a Roux-en-Y loop is created for proper drainage.
- Pancreatic duct to jejunum anastomosis: The surgeon performs an anastomosis between the pancreatic duct and the jejunum, ensuring a tension-free process to minimize leakage or stricture formation, typically using an end-to-side technique.
- Ductal stenting (if necessary): A stent may be placed in the pancreatic duct to maintain patency and facilitate healing, which can be temporary or permanent depending on the patient's condition.
- Closure and drainage: The surgical site is closed after ensuring anastomosis integrity, and drains may be placed in the abdomen to monitor for fluid collections or complications.
Before the procedure
The preparation for pancreaticojejunostomy involves a comprehensive evaluation of the patient's condition, underlying pathology, and optimizing the patient for surgery as mentioned below:
- Medical history and physical examination: The patient's medical history, including pancreatitis, pancreatic cancer, and ductal trauma, is thoroughly reviewed and comorbid conditions are identified through a thorough physical examination.
- Imaging studies: Preoperative imaging is crucial for assessing the pancreatic duct and its surrounding structures, with common imaging modalities including:
- CT scan or MRI: Used to assess ductal dilation, pancreatic cysts, and other structural abnormalities.
- Endoscopic ultrasound (EUS): Used to evaluate the pancreas more precisely and assess for any cystic lesions or ductal irregularities.
- Magnetic resonance cholangiopancreatography (MRCP): Offers detailed visualization of the pancreatic duct system.
- Laboratory tests: Blood tests are essential for evaluating liver function, pancreatic enzyme levels, and overall health, including complete blood count and coagulation profiles.
- Nutritional support: Nutritional counseling and potential supplementation may be necessary for patients experiencing malabsorption or weight loss due to pancreatic dysfunction.
- Antibiotic prophylaxis: Antibiotic prophylaxis can be used to prevent postoperative infections, particularly in patients with underlying pancreatitis or pancreatic cancer.
- Informed consent: The patient must provide informed consent following a thorough discussion of the procedure, risks, benefits, and alternative treatments.
After the procedure
Postoperative care is crucial for a successful recovery and managing any complications following pancreaticojejunostomy.
- Intensive monitoring: Postoperatively, the patient is closely monitored in a high-dependency or ICU unit for signs of haemorrhage, infection, or respiratory complications.
- Pain management: Postoperative care often includes pain control, often managed with opioids and NSAIDs.
- Nutritional support: Early enteral feeding, often via a nasogastric tube or jejunal feeding tube, is initiated to provide nutrients and aid in the healing process, unless it is contraindicated.
- Antibiotics: Prophylactic antibiotics or targeted antibiotics based on cultures may be necessary to prevent infections, particularly in patients with chronic pancreatitis or pancreatic cancer.
- Gradual mobilization: Early mobilization is recommended for patients to decrease the risk of deep vein thrombosis (DVT) and expedite recovery.
Advantages of pancreaticojejunostomy
Pancreaticojejunostomy offers several potential benefits:
- Restores pancreatic drainage: The main advantage is the enhancement of normal pancreatic ductal function, thereby reducing the likelihood of pancreatic insufficiency and its associated complications.
- Pain relief: The procedure can significantly reduce or eliminate pancreatic pain caused by ductal obstruction in chronic pancreatitis.
- Prevention of pseudocysts: PJ can prevent or treat pseudocyst formation by redirecting pancreatic secretions, thereby reducing the risk of infection or rupture.
- Improved quality of life: Post-surgery, many patients, particularly those with chronic pancreatitis or ductal obstructions, experience substantial enhancements in their quality of life.
Pancreaticojejunostomy complications
As with any major surgery, pancreaticojejunostomy carries a risk of complications, including:
- Anastomotic leaks: Leakage from the pancreaticojejunostomy site, a common complication in early postoperative periods, can lead to peritonitis and necessitate additional surgical intervention.
- Pancreatic fistula: Incorrect healing of the pancreatic duct or leakage can lead to the formation of a pancreatic fistula, potentially causing sepsis or abscess.
- Infection: Postoperative infections are prevalent and can affect the surgical site, abdomen, or the pancreas itself.
- Stricture formation: Over time, scar tissue can form around the anastomosis, causing a narrowing of the pancreatic duct and potentially obstructing pancreatic drainage.
- Delayed gastric emptying: This can occur after surgery, causing nausea, bloating, and vomiting.
- Nutritional deficiency: Long-term complications of pancreatic cancer include malabsorption and vitamin deficiencies, particularly in patients with preexisting pancreatic insufficiency.
- Bile duct injury: During pancreatic or jejunum dissection, the bile duct may be injured, potentially causing bile leaks or
jaundice.
Life after Pancreaticojejunostomy Surgery
Postoperative recovery after pancreaticojejunostomy can be prolonged, and patients must adjust to pancreatic disease consequences. Symptoms improve, but long-term follow-up care is necessary for long-term recovery.
- Pancreatic enzyme replacement: Enzyme replacement therapy may be necessary in cases of persistent pancreatic insufficiency.
- Dietary modifications: Patients with chronic pancreatitis or pancreatic surgery may require a specific diet to enhance nutrient absorption.
- Regular monitoring: Follow-up imaging and blood tests are crucial for monitoring for complications like anastomotic stricture, pseudocyst formation, or disease recurrence.
- Psychosocial support: Patients with chronic pancreatitis or pancreatic cancer may benefit from psychological support to cope with the emotional and psychological impacts of the disease.
Pancreaticojejunostomy recovery time
Pancreaticojejunostomy recovery typically involves a 7–10 days hospital stay, with gradual diet reintroduction and pain management. Most patients can resume light activities within 2–6 weeks, but full recovery often takes 6 weeks to 3 months. Long-term, some may need pancreatic enzyme supplements or insulin. Close follow-up is essential to monitor for complications like infection or delayed gastric emptying.
Pancreaticojejunostomy Surgery Cost in Hyderabad, India
Pancreaticojejunostomy Surgery Cost in Hyderabad, India varies from ₹2,20,000 to ₹4,55,000 (US$2530 to US$5250). The final procedure cost depends on various factors, including type of surgical technique (open or laparoscopic), severity, required diagnostic procedures, hospital facilities, surgeon expertise, hospital stay & ICU care, medical procedures & medications, post-surgical care & rehabilitation.
Pancreaticojejunostomy is a hepatobiliary (HPB) surgery performed to relieve chronic pancreatitis symptoms, pain and improve pancreatic drainage. PACE Hospitals, a leading HPB surgery hospital in Hyderabad, India, offers affordable and high-quality pancreaticojejunostomy surgery (Lateral Pancreaticojejunostomy for pancreatic duct stones and Longitudinal Pancreaticojejunostomy for a dilated pancreatic duct without an inflammatory mass) with expert gastroenterology and hepato-pancreato-biliary (HPB) surgeons, advanced robotic and laparoscopic facilities.
Success rate of pancreaticojejunostomy
The success rate of pancreaticojejunostomy is typically 80% to 90%, depending on factors like surgeon skill, patient health, and post-operative care. Proper management reduces the risks of complications like leaks or infections. When done correctly, it restores pancreatic enzyme drainage and improves digestion.
Frequently asked questions (FAQs) on Pancreaticojejunostomy Surgery
What are the risks of pancreaticojejunostomy?
Complications may include leaks, infections, delayed gastric emptying, pancreatic fistulas, or bleeding. Proper surgical technique and post-operative care are crucial in minimizing these risks and ensuring successful recovery.
How long does the recovery take after pancreaticojejunostomy?
Recovery time varies, but typically, patients stay in the hospital for about 5–7 days. Full recovery may take several weeks, with gradual reintroduction to normal activities. Follow-up care is essential for monitoring healing and function.
Is pancreaticojejunostomy a permanent procedure?
Yes, once the pancreas is connected to the jejunum, the procedure is permanent. It helps in maintaining pancreatic enzyme drainage to aid digestion, especially if part of the pancreas was removed.
Are there alternatives to pancreaticojejunostomy?
Alternatives depend on the underlying condition. Some patients may not require pancreaticojejunostomy if the condition can be managed with other treatments, such as medication, drainage tubes, or different surgical options like pancreaticoduodenectomy.
Can I resume normal activities after pancreaticojejunostomy?
Most patients can gradually resume normal activities after a few weeks, depending on how well they heal. However, strenuous activity should be avoided for several weeks, and lifting heavy objects should be limited to avoid strain.
Why is pancreaticojejunostomy performed?
This procedure is typically done to restore the flow of pancreatic enzymes into the small intestine after the removal of part of the pancreas or the duodenum, particularly in cases of pancreatic cancer, chronic pancreatitis, or trauma.
What are the symptoms of complications after pancreaticojejunostomy?
Symptoms of complications may include fever, abdominal pain, swelling, jaundice, or difficulty eating. If any of these occur, it is important to contact the surgeon or healthcare expert immediately to avoid further issues.
How is the success of pancreaticojejunostomy determined?
Success is typically determined by the patient's recovery, absence of complications, and the restoration of normal pancreatic function. Follow-up imaging and tests are used to ensure proper drainage and healing.
What dietary changes are required after pancreaticojejunostomy?
Patients may need to follow a low-fat diet initially to reduce pancreatic stress. Digestive enzyme supplements may be prescribed to help with nutrient absorption. Long-term adjustments will depend on individual recovery and digestive function.
Can pancreaticojejunostomy lead to diabetes?
Yes, if a significant portion of the pancreas is removed, patients may develop diabetes due to reduced insulin production. Regular blood sugar monitoring and diabetes management may be necessary after surgery.
What is the role of the surgeon in pancreaticojejunostomy?
The surgeon carefully performs the procedure, ensuring that the pancreas and jejunum are securely connected. The goal is to minimize the risk of leaks or complications while restoring pancreatic function for digestion.
How is the procedure performed?
Pancreaticojejunostomy involves connecting the pancreas to the jejunum, usually via an anastomosis. It is often done during a Whipple procedure or after a pancreatic resection, requiring precise surgical skills and proper post-op care.
Can pancreaticojejunostomy be performed laparoscopically?
Yes, pancreaticojejunostomy can be performed laparoscopically in some cases, especially in patients who do not have large tumors or extensive disease. Laparoscopic surgery offers benefits like smaller incisions and faster recovery times.
What is the role of post-operative care after pancreaticojejunostomy?
Post-operative care includes managing pain, preventing infections, monitoring for complications (e.g., pancreatic fistula), and ensuring proper nutrition and hydration. Early mobilization and follow-up visits are important for tracking progress and healing.
What are the long-term effects of pancreaticojejunostomy?
In the long term, patients may experience improved digestive function, but some may develop complications like digestive enzyme insufficiency or
diabetes. Regular follow-up visits are important to monitor pancreatic function and overall health.
Is there a risk of pancreatic leakage after pancreaticojejunostomy?
Yes, pancreatic leakage is one of the most common complications after pancreaticojejunostomy. It occurs when digestive juices leak from the pancreas into the abdominal cavity, potentially causing infection or inflammation, but can usually be treated with proper care.
How do you monitor pancreatic function after pancreaticojejunostomy?
Monitoring pancreatic function typically involves blood tests to assess enzyme levels, imaging studies (like CT scans), and regular follow-up with the surgeon to evaluate for signs of complications or dysfunction.
What is the role of enzyme replacement therapy after pancreaticojejunostomy?
After the procedure, patients may require enzyme replacement therapy to aid digestion. This is especially important if the pancreas no longer produces enough digestive enzymes. The therapy helps to break down food and improve nutrient absorption.


