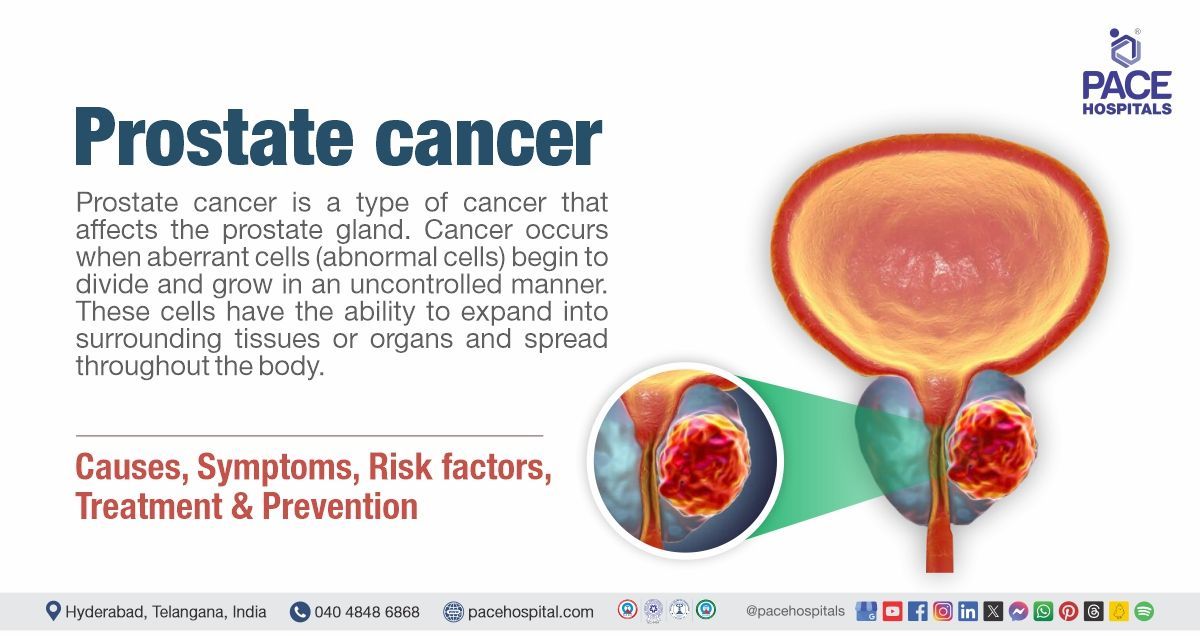
Prostate Cancer - Causes, Symptoms, Risk factors, Treatment and Prevention
Prostate cancer definition
Prostate cancer is a type cancer that affects the prostate gland. Cancer occurs when abnormal cells (abnormal cells) begin to divide and grow in an uncontrolled manner. These cells have the ability to expand into surrounding tissues or organs and spread throughout the body.
A multidisciplinary team (MDT) of physicians and other health care providers collaborates to treat prostate cancer. The multidisciplinary team may include, a
urologist, radiation oncologist, medical oncologist, radiologist, etc.
Prostate cancer meaning
Prostate cancer is the culmination of two words in which “prostate” is derived from the Greek word "prostátēs", which means "one who stands before" or "protector, guardian".
The word "cancer" is derived from the Greek word "karkinos", meaning which "crab". The Greek physician Hippocrates (460-370 BC) adopted the phrase to characterise tumors, probably because the spreading projections of a cancer resemble crab legs. Celsus, a Roman physician (25 BC-50 AD), later translated the Greek phrase into “cancer”, the Latin word for crab.
In 1853, J. Adams, a surgeon at The London Hospital, recorded the first case of prostate cancer that he detected through histological examination. Adams described this illness as "a very rare disease" in his study. Amazingly, 150 years later, prostate cancer has become a major health concern.
Prostate cancer prevalence
Prevalence of prostate cancer worldwide
Prostate gland cancer is the second most frequent cancer in males worldwide, accounting for the fifth highest cause of cancer death in men. Here are some statistics regarding the prevalence of prostate cancer:
Prostate cancer incidence worldwide
Male prostate cancer is the third most commonly diagnosed malignancy (cancer) worldwide. It is a highly uncommon disease, with incidence rates ranging from 6.3 to 83.4 per 100,000 men worldwide. Age-standardized incidence rates are highest in Northern Europe and lowest in South Central Asia.
Prostate cancer mortality rate
The death rate for prostate cancer varies based on the stage of diagnosis, as well as other factors including age and race.
Prostate cancer has a 5-year survival rate of more than 99% for early-stage patients, but just 34% for advanced or metastatic prostate cancers.
The 5-year survival rate decreases with age, with a larger risk for men aged 70-79 years and men over 80 years.
Estimated new cases of prostate cancer worldwide
In 2020, there were an anticipated 1.4 million new cases of prostate cancer worldwide
Prevalence of prostate cancer in India
Prostate cancer is the second leading cancer among males in major Indian cities such as Delhi, Kolkata, Pune, and Thiruvananthapuram, the third leading cancer in cities such as Bangalore and Mumbai, and one of the top ten leading cancers in the rest of India's population-based cancer registries (PBCR). The PBCRs in Bangalore (Annual Percentage Change: 3.4%), Chennai (4.2%), Delhi (3.3%), Mumbai (0.9%), and Kamrup urban district (11.6%) showed a statistically significant rise in incidence rates over time.
Compared data available from multiple cancer registries demonstrated that the average yearly cancer incidence rate for prostate cancer in India ranged from 5.0 to 9.1 per 100,000 men per year.

Types of prostate cancer
The types of prostate cancer in men determine which sort of cell the cancer began in. Prostate cancer is classified into various categories, including:
- Adenocarcinoma of the prostate
- Acinar adenocarcinoma of the prostate
- Ductal adenocarcinoma of the prostate
- Transitional cell carcinoma of the prostate
- Squamous cell carcinoma of the prostate
- Small cell prostate cancer
- Sarcoma
- Lymphoma
Adenocarcinoma prostate cancer
Adenocarcinoma is the most frequent kind of prostate cancer that arises from the gland cells that line the prostate gland and its tubes and produce the prostatic fluid. Adenocarcinoma of the prostate is classified into two types:
- Acinar adenocarcinoma of the prostate
- Ductal adenocarcinoma of the prostate
Acinar adenocarcinoma of the prostate
Acinar adenocarcinoma is a kind of prostatic adenocarcinoma, which is the most common type of prostate cancer in most people that arises in the acini cells that line the prostate’s fluid-secreting glands.
Ductal adenocarcinoma of the prostate
Ductal adenocarcinoma is another type of prostatic adenocarcinoma that arises in the cells of the prostate gland ducts, which is an uncommon but more aggressive cancer (tends to grow and spread faster) than acinar adenocarcinoma.
Transitional cell carcinoma of the prostate
Transitional cell carcinoma, also known as urothelial cancer of the prostate, begins in the cells that border the tube that transports urine outside of the body (the urethra) and accounts for 2 – 4% cases. This type of cancer typically starts in the bladder and progresses to the prostate. However, it can occasionally originate in the prostate and progress to the bladder opening and surrounding tissues.
Squamous cell carcinoma of the prostate
This type of malignancy (cancer) grows from the flat cells that cover the prostate, called basal cells and typically develops and spreads faster than prostate adenocarcinoma.
Small cell prostate cancer
Small cell prostate cancer is also classified as neuroendocrine cancer that typically grows faster than other types of prostate cancer. Other rare types of prostate cancer include:
- Sarcoma (cancers in bones and soft tissues)
- Lymphoma (lymphatic system cancer)
Aggressive types of prostate cancer
Out of the various types of prostate cancers mentioned above, ductal prostate cancer and neuroendocrine prostate cancer (small cell prostate cancer) are considered aggressive prostate cancer and has the potential to spread very quickly to the lymph nodes.
Prostate cancer symptoms
Prostate cancer symptoms in males can vary greatly, and many men may not show any signs until the disease has advanced. Early detection is critical, as prostate cancer is one of the most common tumors in males. Symptoms based on the prostate cancer stages are mentioned below:
Stage 1 prostate cancer symptoms
Stage 1 prostate cancer, also called localised prostate cancer, is an early-stage malignancy that is limited to the prostate gland and has not gone beyond it. Many men may not experience noticeable symptoms at this early stage. However, potential signs and symptoms that may indicate stage1 prostate cancer, which can be considered as early symptoms of prostate cancer, include:
- Urinary hesitancy (difficulty in starting urination)
- Postmicturition dribbling (involuntary loss of urine after urination)
- Poor urinary stream
- Haematuria (blood in urine)
- Hemoejaculate (rarely) (presence of blood in ejaculate)
- New-onset erectile dysfunction
Stage 2 prostate cancer symptoms
As mentioned, early stages of prostate cancer often present with no symptoms; however, stage 2 symptoms can be mild (not so severe) and might present with noticeable changes, including:
- Urinary hesitancy (trouble urinating)
- Hematospermia (blood in semen)
- Discomfort in the pelvis
Stage 3 prostate cancer symptoms
Prostate cancer is classified as stage III when it has spread beyond the capsule surrounding the prostate gland and may involve adjacent tissues. By stage 3, early signs may include urinary issues, including:
- A weak urinary stream
- Frequent urination
- Urinary incontinence
- Nocturia (urinating at nighttime)
- Haematuria (blood in urine)
- Unable to urinate after an urge to urinate
- Hematospermia (blood in semen)
Erectile dysfunction is also seen in patients with stage 3 prostate cancer
Stage 4 prostate cancer symptoms
Stage 4 prostate cancer happens when prostate cancer has spread to distant organs or tissues at the time of diagnosis. If the cancer in the prostate has started to spread, patients may experience symptoms such as:
- Bone pain
- Fatigue (tiredness)
- Feeling generally unwell
- Unintended weight loss
Prostate cancer causes
Causes of prostate cancer in men are numerous and can vary significantly between people. Age is one of the major risk factors, with males over 50 having a significantly higher chance of being diagnosed. Men who have a family history of prostate cancer are more likely to develop the disease. Lifestyle factors, such as nutrition and physical activity levels, have been associated with prostate cancer.
Gene changes linked to prostate cancer
DNA is the material found in cells that makes up genes and determines their function. Cancer develops due to the accumulation of genetic alterations (mutations) in the DNA because these mutations affect genes that control cell proliferation, replication, cell death, and DNA repair.
Humans typically resemble their parents because they inherit DNA from them. However, genes affect more than just physical appearance.
As mentioned above, some genes generally control mechanism, including when cells should grow, divide to generate new cells, or correct DNA errors, while others cause cells to die when they should.
When these mechanisms are disrupted, some cells multiply abnormally, resulting in the formation of a tumor. As the tumor grows, its cells acquire more mutations, allowing it to induce the formation of new blood vessels to sustain future growth.
A tumor may eventually develop large enough to invade neighboring organs, such as the seminal vesicles or bladder. In advanced tumors, cells may have the ability to detach from their original tissue site and evade the immune system.
These cells can go through the lymphatic system to neighboring lymph nodes or through the circulation to the bone marrow and (in rare cases) other bodily regions. Cancer cells continue to develop and disturb normal bodily functions in these new places. Metastasis (spreading) generates the majority of the suffering associated with prostate cancer and can finally kill the patient.
Inherited gene mutation
Certain gene mutations can pass on through the generations, and such inherited mutated genes are thought to be a major factor in 10% of prostate tumors (cancer). Cancers that develop due to inherited gene mutations are called hereditary cancers.
Hereditary prostate cancer has been associated with inherited mutations in a number of genes, including:
- BRCA1 and BRCA2: These genes usually aid in the repair of DNA errors in cells (or cause the cell to die if the error cannot be corrected). Mutations in these genes (particularly BRCA2 gene mutation) have been associated to an increased risk of prostate cancer.
- CHEK2, ATM, PALB2, and RAD51: Mutations (alterations) in these DNA repair genes could be responsible for some hereditary prostate cancers.
- DNA mismatch repair genes (such as MSH2, MSH6, MLH1, and PMS2): These genes typically aid in the repair of DNA errors (mismatches) that might occur when a cell prepares to divide into two new cells. (Cells must create a new copy of their DNA every time they divide.) Men with inherited mutations in one of these genes have Lynch syndrome (also known as hereditary non-polyposis colorectal cancer, or Hereditary nonpolyposis colorectal cancer-HNPCC), and are at a greater risk of colorectal, prostate, and other types of cancers.
- RNASEL (formerly known as HPC1): The usual function of this gene is to assist cells in dying when something goes wrong within them. Inherited abnormalities in this gene may allow cells with defects to live longer than expected, increasing the risk of developing prostate cancer.
- HOXB13: This gene plays a vital role in prostate gland development. Mutations in this gene have been associated to early-onset prostate cancer (prostate cancer diagnosed at a young age), which occurs in some families.
Acquired gene mutations
Some genes can alter during an individual's lifespan. This form of mutation is not passed on to children and can only be found in cells derived from the original altered cell. They are referred to as acquired mutations.
When a cell prepares to divide into two cells, it must make a duplicate of its DNA for each new cell. This procedure isn't always perfect, and errors might occur, resulting in damaged DNA in the new cell. It is unclear how often these DNA alterations are random and how often they are impacted by other factors (such as food, hormone levels, and so on).
In general, the faster prostate cells grow and divide, the more mutations are likely to occur. As a result, anything that accelerates this process may increase the risk of prostate cancer.
Causes of prostate cancer in young males
The reasons for prostate cancer development in younger men are quite unclear. It appears that early onset prostate cancer is correlated with certain genes. More research is necessary to determine the potential significance of factors such as physical activity, obesity, HPV infection, and exposure to environmental chemicals that cause cancer.
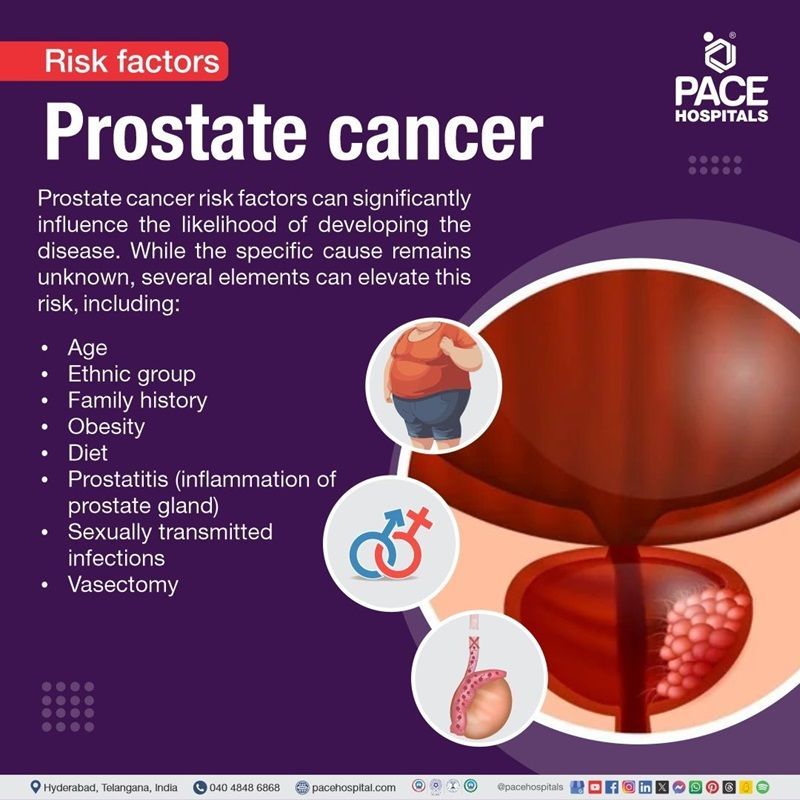
Prostate cancer risk factors
Prostate cancer risk factors can significantly influence the likelihood of developing the disease. While the specific cause remains unknown, several elements can elevate this risk, including:
- Age
- Ethnic group
- Family history
- Obesity
- Diet
- Prostatitis (inflammation of the prostate gland)
- Sexually transmitted infections
- Vasectomy
- Chemical exposure
Age: The prostate cancer risk rises with age, and the majority of cases are identified in men over 50 years of age as a risk factor for prostate cancer.
Ethnic group: Black males are more likely than Asian men to develop prostate cancer.
Family history: Research indicates that having a close female relative who developed breast cancer may also raise the risk of developing prostate cancer. Having a brother or father who developed prostate cancer before the age of 60 tends to enhance the risk of developing prostate cancer.
Obesity: According to recent studies, there may be a connection between obesity and prostate cancer. Having a healthy diet and regular exercise can help to manage obesity, thus reducing the risk of prostate cancer.
Diet: According to some research on this topic of food and prostate cancer, a diet heavy in calcium may be associated with one of the higher risk factors for prostate cancer.
Prostatitis (inflammation of prostate gland): Some studies have suggested that prostatitis (inflammation of the prostate gland) may be associated with an increased risk of prostate cancer, but others have found no such link. Inflammation is frequently observed in prostate tissue samples that include malignancy however the relationship between the two is unclear, and research is ongoing.
Sexually transmitted infections: Researchers have investigated whether sexually transmitted infections (such as gonorrhoea or chlamydia) increase the risk of prostate cancer because they promote prostatic inflammation. So far, investigations have produced inconsistent outcomes, with no definite conclusions made.
Vasectomy: Some research studies have suggested that men who have a vasectomy (minor surgery to make them sterile) have a slightly higher risk of prostate cancer, but other studies have found no increase in risk. The investigation into this probable link is still ongoing.
Chemical exposure: According to research, exposure to some chemicals may raise the risk of developing prostate cancer. For example: research studies have revealed a relationship between exposure to arsenic and an increased risk of prostate cancer. There is some indication that firefighters may be exposed to substances that raise their risk of prostate cancer.
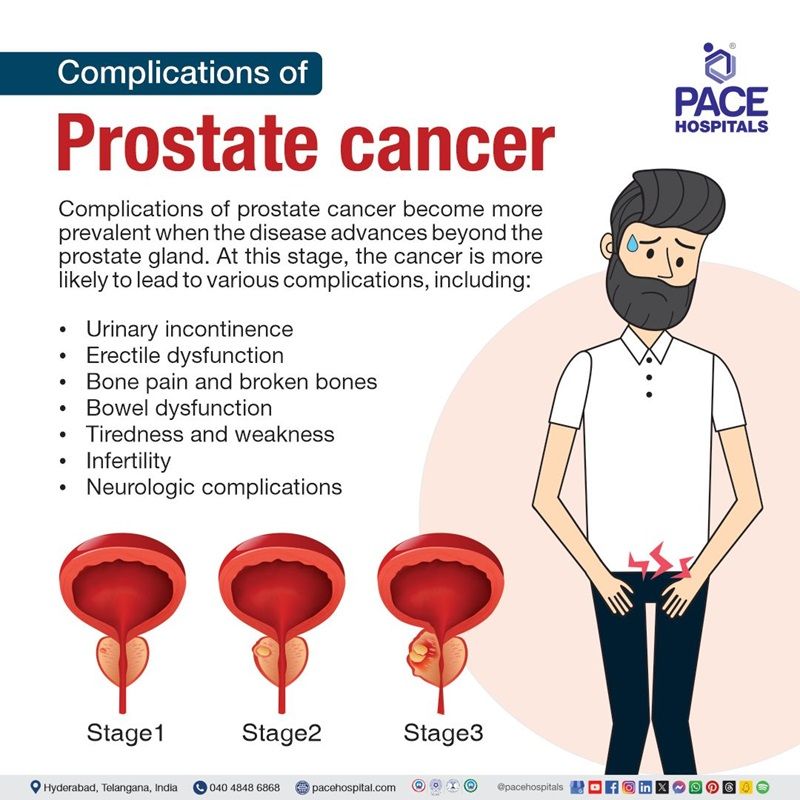
Complications of prostate cancer
Complications of prostate cancer become more prevalent when the disease advances beyond the prostate gland. At this stage, the cancer is more likely to lead to various complications, including:
- Urinary incontinence: Prostate cancer and its treatment options can cause urinary incontinence, or the inability to control the bladder.
- Erectile dysfunction: Prostate cancer and the treatments used to treat this cancer, can induce erectile dysfunction, which is the inability to get a full erection
- Bone pain and broken bones: Advanced prostate cancer can cause a variety of pains, such as patients may experience bone pain (feels like a dull aching) when it spreads to the bones. If the tumour could press on a nerve, resulting in a stabbing or burning feeling.
- Bowel dysfunction: Radiation, chemotherapy, hormone treatments, and surgery might make it difficult to eat or digest food regularly. Patients may have nausea, vomiting, loose stools, and diarrhoea.
- Tiredness and weakness: Radiotherapy for prostate cancer can cause fatigue and weakness that can continue for several weeks after treatment has ended.
- Infertility: After radiotherapy or hormone therapy for prostate cancer, patients may generate little or no sperm. These treatments can also harm sperm, by lowering the sperm count. As a result, patients may find it more difficult to have children naturally.
- Neurologic complications: Rare neurologic consequences include peroneal neuropathy, cerebellar ataxia (unexpected lack of coordination in muscular action due to cerebellar damage or illness), limbic encephalitis (abnormal limbic system and hypothalamus), and brain-stem encephalitis.
Prostate cancer diagnosis
Prostate cancer diagnosis typically occurs through screening, as most cases are detected before symptoms arise. While early prostate tumours often remain asymptomatic, more advanced malignancies may present noticeable symptoms that prompt further investigation, including:
- Medical history
- Physical examination
- Digital rectal examination
Suppose prostate cancer is suspected based on screening test results or symptoms. In that case, more testing will be required to confirm the actual diagnosis. If the patient consults general physician (primary care physician). In that case, the patient will be referred to a urologist who specialises in the treatment of genital and urinary tract illnesses, including prostate cancer. The urologist may follow those above-mentioned diagnostic criteria and other advanced prostate cancer tests, including:
- PSA (prostate specific antigen) blood test
- Prostate cancer PSA levels
- Prostate cancer biopsy
- Imaging tests
- Other tests
PSA (prostate specific antigen) blood test
PSA is a protein produced by cells in the prostate gland. The PSA test is a blood test for prostate cancer that measures the amount of PSA in the blood. Increased levels of PSA may indicate prostate cancer.
Prostate cancer PSA levels
PSA value in prostate cancer may vary as there is no specific values for PSA in the blood. In the past, PSA readings of 4.0 ng/mL or lower were considered normal. However, some patients with PSA levels below 4.0 ng/mL have prostate cancer, and many with higher PSA values between 4 and 10 ng/mL do not have prostate cancer.
Prostate cancer biopsy
A biopsy is a technique in which tiny samples of the prostate are taken and examined using a microscope. If the findings of a PSA blood test, digital rectal examination, or other testing indicate that the patient has prostate cancer, the patient may require biopsy for prostate cancer detection.
Imaging tests
- Transrectal ultrasound (TRUS)
- Magnetic resonance imaging (MRI)
- Multiparametric MRI (mpMRI)
- MRI/ultrasound fusion-guided prostate biopsy
- Bone scan
- Positron emission tomography (PET) scan
- Computed tomography (CT) scan
Other tests
Other tests that may help to diagnose prostate cancer include:
- Prostate cancer gene 3 (PCA3) test
- Prostate Health Index (PHI)
- Lymph node biopsy
Prostate cancer Gleason score
The appearance of normal prostate cells changes under the microscope as they transform into cancer cells. The pathologist assigns a Gleason grade to the prostate cancer on a scale of 1 to 5 based on how similar it appears to healthy prostate tissue. The higher the Gleason score, the more unusual the cancer cells appear.
Prostate cancer treatment
Prostate cancer treatment includes various options where the oncologist may determine the type of treatment suitable according to the patient’s condition and common therapies for prostate cancer include:
Conservative management (Expectant management)
- Active surveillance
- Watchful waiting
Surgical management (Prostate cancer surgery)
- Radiation therapy
- External radiation therapy
- Internal radiation therapy (brachytherapy)
- Other therapies
- Cryotherapy
- Chemotherapy
- Biological therapy
- High-intensity focused ultrasound
- Hormone treatments
- Targeted therapy
There are various treatment options for prostate cancer. The oncologist may determine the type of treatment suitable based on the patient’s condition. Some common therapies for prostate cancer include:
Conservative management (Expectant management)
- Active surveillance: Prostate cancer is closely monitored by performing prostate specific antigen (PSA) testing and prostate biopsies on a regular basis and treated only if it spreads or produces symptoms.
- Watchful waiting: No tests are performed. The physician will only address any symptoms that may arise. This procedure typically suggested for men who are not expected to live longer than ten years. Watchful waiting is a therapeutic strategy in which a patient's condition is closely monitored without treatment until symptoms change or arise. It is sometimes referred to as active surveillance.
Surgical management (Prostate cancer surgery)
A prostatectomy is a surgical procedure in which healthcare experts remove the prostate. A radical prostatectomy involves removing both the prostate and the seminal vesicles. Surgical management of prostate cancer includes various options, such as:
Radiation therapy
- Radiation therapy for prostate cancer involves using high-energy rays (similar to x-rays) to eliminate cancer. There are two kinds of radiation therapy:
- External radiation therapy: An equipment outside the body delivers radiation to cancer cells.
- Internal radiation therapy (brachytherapy): Radioactive seeds or pellets are surgically implanted into or near the cancer to kill cancer cells.
Other therapies
Depending on the extent of spread of prostate cancer to lymph nodes and other organs, other therapies that can be used to treat prostate cancer include:
- Cryotherapy: Cryotherapy for prostate cancer is less frequently used and involves using a special probe inserted inside or near the prostate cancer to freeze and kill the cancer cells.
- Chemotherapy: Chemotherapy for prostate cancer is done using specialized medications (prostate cancer drugs), including tablets, injections, or a combination of the two to reduce or destroy cancer that has spread to other parts of the body.
- Biological therapy: Biological therapy for prostate cancer works with the immune system to help it fight cancer or to manage the negative effects of other cancer treatments.
- High-intensity focused ultrasound (prostate cancer ultrasound): High intensity ultrasound for prostate cancer therapy uses high-energy sound waves (ultrasound) to attack cancer cells. This high intensity ultrasound to treat prostate cancer is not commonly used.
- Hormone treatments: Hormone treatments for prostate cancer prevents cancer cells from receiving the hormones they require to develop. This is sometimes termed androgen deprivation therapy (ADT).
- Targeted therapy: Prostate cancer targeted therapy is done using medications that target cancer cells while causing minimal damage to healthy cells. Targeted therapy is used to treat prostate cancer that has progressed to other regions of the body and is resistant to hormone therapy.
Best treatment for prostate cancer in early stages
Early-stage prostate cancer can be treated with either surgery or radiation therapy. These treatments aim to cure cancer permanently and have almost the same success in treating cancer.
The concerned physician may treat the early-stage prostate cancer either with radiation or surgery depending on the overall condition of the patient.
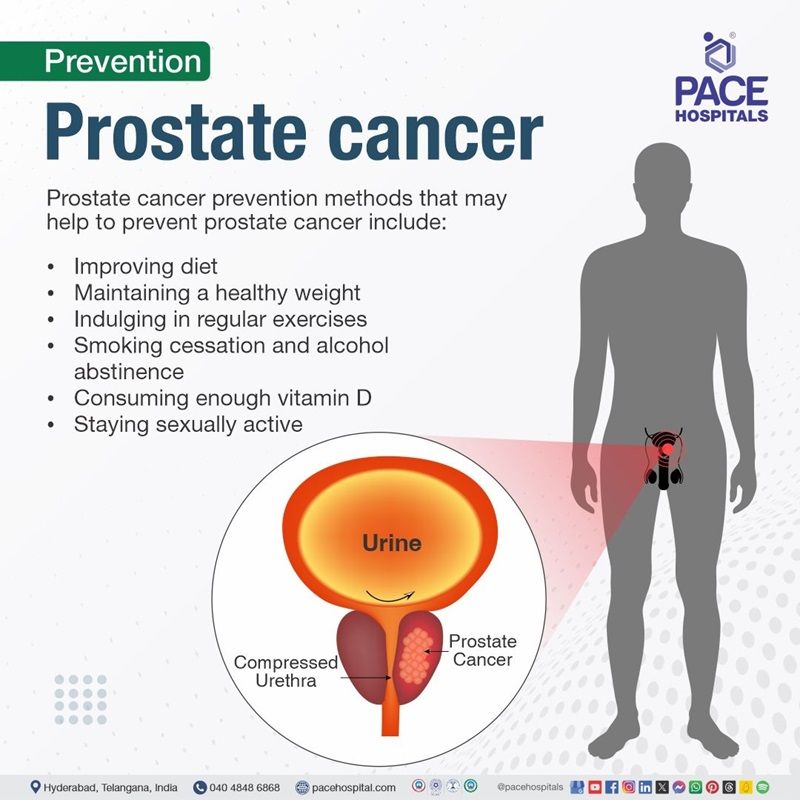
Prostate cancer prevention
While many people question preventive methods against prostate cancer, as there is no single preventive strategy to prevent it. Staying healthy as men age, or trying to deal with existing health issues, can help reduce the risk. However, like all cancers, prostate cancer has some risk factors that must be prevented. prostate cancer prevention methods that may help to prevent prostate cancer include:
- Improving diet
- Maintaining a healthy weight
- Indulging in regular exercises
- Smoking cessation and alcohol abstinence
- Consuming enough vitamin D
- Staying sexually active
Improving diet: Researchers may not fully understand the association between nutrition and prostate cancer prevention, although studies indicate that some eating patterns may be beneficial, such as:
- Reducing fat intake
- Eating more vegetables and fruits
- Avoiding charred meat (meat that is burnt partially)
Maintaining a healthy weight: Obesity increases the risk of getting more aggressive prostate cancer. In general, losing weight and keeping a healthy weight as men become older will help lower their risk of cancer and other health concerns.
Indulging in regular exercises: Exercise can help people to achieve a healthy weight, lower inflammation, boost immunological function, and counteract some of the negative health effects of a sedentary lifestyle—all of which can help to avoid cancer.
Smoking cessation and alcohol abstinence: Quitting smoking has several health benefits, including lowering the risk of cancer. If men have a habit of consuming alcohol, keeping it in moderate may help. Some research suggest that red wine contains antioxidants that may be beneficial to health.
Consuming enough vitamin D: Most people do not consume enough vitamin D. Vitamin D can help prevent prostate cancer and other problems. Cod liver oil, wild salmon, and dried shitake mushrooms are all good sources of vitamin D. As the sun is a superior, more easily available source of vitamin D, many experts advise obtaining 10 minutes of sun exposure (without sunscreen) every day.
Staying sexually active: Research studies demonstrate that men who ejaculate more frequently (with or without a sexual partner) are up to two-thirds less likely to develop prostate cancer. Although research is ongoing, some experts believe that ejaculation helps the body to get rid of toxins and other compounds that can cause inflammation.
Medicine to prevent prostate cancer
Men with
benign prostatic hyperplasia (BPH) are frequently treated with dihydrotestosterone (DHT) lowering medications. These medications have been carefully tested to see if they might prevent prostate cancer, and the results indicate that they could cut cancer risk by approximately 25%.
Difference between BPH and Prostate cancer
BPH vs prostate cancer
The predominant difference between an enlarged prostate and prostate cancer is that benign prostatic hyperplasia (enlarged prostate) is the non-cancerous increase in size of the prostate, whereas the prostate cancer refers to the cancerous (malignant) growth of prostate gland. The major difference between enlarged prostate and prostate cancer are listed below:
| Elements | Benign prostatic hyperplasia (BPH)/ enlarged prostate | Prostate cancer |
|---|---|---|
| Nature of condition | Non-cancerous enlargement of the prostate | Malignant (cancerous) growth of prostate cells |
| Cell growth | Overgrowth of normal prostate cells | Uncontrolled growth of cancerous cells |
| Symptoms | Frequent urination, weak urine stream, difficulty starting urination, nocturia | Often asymptomatic in early stages; advanced stages may include blood in urine, pain in back/hips, difficulty urinating |
| Risk factors | Aging, family history, hormonal changes | Aging, family history, race (higher risk in Black men), unhealthy diet, physical inactivity |
| Disease progression | Generally slow and non-life-threatening | Can be slow growing but may spread (metastasize) to other parts of the body if untreated |
| Diagnosis | Digital rectal exam (DRE), urine tests, PSA blood test | PSA (prostate specific antigen) blood test, biopsy, imaging tests (MRI, CT scans) |
| Treatment | Medications, lifestyle changes, surgery (TURP) | Surgery, radiation therapy, hormone therapy, chemotherapy |
| Impact on life expectancy | Typically, does not affect life expectancy | Can be life-threatening if not treated early |
Frequently Asked Questions (FAQs) on Prostate cancer
Is prostate cancer curable?
Yes, prostate cancer is usually curable and often treatable with early detection. Prostate cancer has one of the greatest survival rates of any cancer, and it is typically treatable if detected early. Physicians normally consider a patient is cured if he has no indications of cancer for at least 5 years.
What are the 5 warning signs of prostate cancer?
The early warning signs of prostate cancer in men requires immediate attention include, dysuria (pain or burning during urination), nocturia (frequent urination at nighttime), difficulty starting or stopping urination, haematuria (blood in the urine), haematospermia (blood in semen) and sudden erectile dysfunction.
What is the most accurate test for prostate cancer?
A biopsy is the primary technique for diagnosing prostate cancer, but a healthcare clinician might use other tools to ensure that the sample is taken in the correct location. For example, health care experts may employ transrectal ultrasound or magnetic resonance imaging (MRI) to guide the biopsy.
Will there, loss of libido with prostate cancer?
Yes, there will be loss of libido with prostate cancer because prostate cancer becomes increasingly common with age, at least one-third of men experience sexual issues at the time of diagnosis. All localized prostate cancer treatments increase the likelihood of sexual dysfunction, including loss of desire, erectile dysfunction, and alterations in orgasm. Even men on active surveillance had a higher incidence of issues than their contemporaries who do not have prostate cancer. Men who undergo androgen deprivation therapy (ADT) have the highest rates of sexual dysfunction.
What is the lifespan of someone with prostate cancer?
For most men who are diagnosed with prostate cancer, the lifespan is very similar to that of a man without prostate cancer, with a 5-year survival rate of nearly 100% and a 10-year survival rate of around 98%, which means the majority of men diagnosed with prostate cancer will live a normal lifespan; however, this largely depends on the stage of the cancer at diagnosis and individual health factors.
How to avoid prostate cancer?
There is no certain way to avoid prostate cancer, but there are several things that men may adopt to reduce the risk of prostate cancer development. Preventive measures include, regular exercise, consuming a healthy diet, smoking cessation, staying sexually active.
Will treatment reduce the spread of prostate cancer?
Yes, prostate cancer treatment, especially when detected early, can significantly reduce the spread of the cancer, particularly through the use of hormone treatments which can slow down the cancer's growth and prevent further metastasis (spreading), especially in advanced stages where the cancer has spread to other parts of the body; however, it's important to note that treatment cannot always completely cure advanced prostate cancer, but can help manage its progression and symptoms.
Why do so many black men get prostate cancer?
One in every four black males develop prostate cancer in their lifetime. Black males are more likely than other men to develop prostate cancer, with a one-in-eight probability. Research demonstrates that genes may play a role in the development of prostate cancer in black males. However, the exact reason is still unknown.
When is radiation needed for prostate cancer?
Radiation therapy can treat prostate cancer in its early stages as well as in more advanced stages that has spread beyond the prostate. Radiation for prostate cancer can be used alone or in conjunction with other therapies, such as hormone deprivation. This therapy is also used to treat recurring prostate cancer after surgery.
How to detect prostate cancer without a biopsy?
There are several diagnostic modalities other than biopsy to detect prostate cancer, including digital rectal examination, PSA (prostate specific antigen) blood test, multiparametric MRI (mp-MRI) etc. Magnetic resonance imaging (MRI) has recently improved the pathway for the identification of clinically significant prostate cancer, leading up in a recommendation of prostate MRI before a prostate biopsy.
Is premature ejaculation a symptom of prostate cancer?
No. There is no link between premature ejaculation and prostate cancer and its treatment. In fact, chemotherapy and radiation treatment for prostate cancer may produce retrograde ejaculation (entry of semen into bladder) or dry orgasm (ejaculating with no semen).
How to boost immune system to fight prostate cancer?
Numerous techniques have been proposed to improve anticancer immunity in prostate cancer, including immune checkpoint inhibitors (ICIs), cancer vaccines, adoptive cell therapy, cytokine-based therapies, adjuvant therapy, nanoparticles, and targeting other particular molecules.
What are the 4 stages of prostate cancer?
The four prostate cancer stages include stage I, stage II, stage III and stage IV, explaining:
Stage 1 cancer is found in only half of one side of the prostate, or less. It is fully confined within the prostate gland.
Stage 2 cancer occurs on more than half of one side of the prostate. However, it is still entirely confined within the prostate gland.
Stage 3 indicates that the cancer has broken through the prostate gland's covering (capsule). It could have spread into the tubes that deliver sperm (seminal vesicles).
In
stage 4 prostate cancer (final stages) the cancer starts spreading to nearby lymph nodes eventually spreading to other organs.
Is prostate cancer hereditary?
Prostate cancer is exceptionally heritable. More than half of an individual's prostate cancer risk is inherited from their parents. Significant research has been conducted to discover and characterize inherited germline (describes the cells that give rise to sperm and eggs) variations that contribute to the genetic component of prostate cancer risk.
What is watchful waiting for prostate cancer?
Watchful waiting is intended for individuals who are too old or sick with other life-threatening conditions to benefit from local treatment. Rather than employing active surveillance to check normal test results, people just monitor their own symptoms and notify their physician if anything changes. The purpose of watchful waiting is to monitor prostate cancer until it has metastasized (spread to distant places) or begins to cause symptoms such as pain or urinary tract blockage. Patients can then choose to receive treatment.
Can PSA be normal in prostate cancer?
Yes. A normal PSA (prostate specific antigen) level can exist in males with prostate cancer. There is no exact normal or abnormal PSA level in the blood, and what is considered normal fluctuates with age. For men 60 and older, a normal PSA level is 4.0 mg/mL or below, whereas men 59 and younger have a normal PSA level of 2.5 mg/mL or less.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868