Transurethral Resection of Bladder Tumour (TURBT)
This answers some of the questions you might have about this treatment. It explains the benefits, risks and alternatives to the procedure, as well as what you can expect when you come into hospital. If you have any questions, please speak to your doctor, who will be happy to help you.
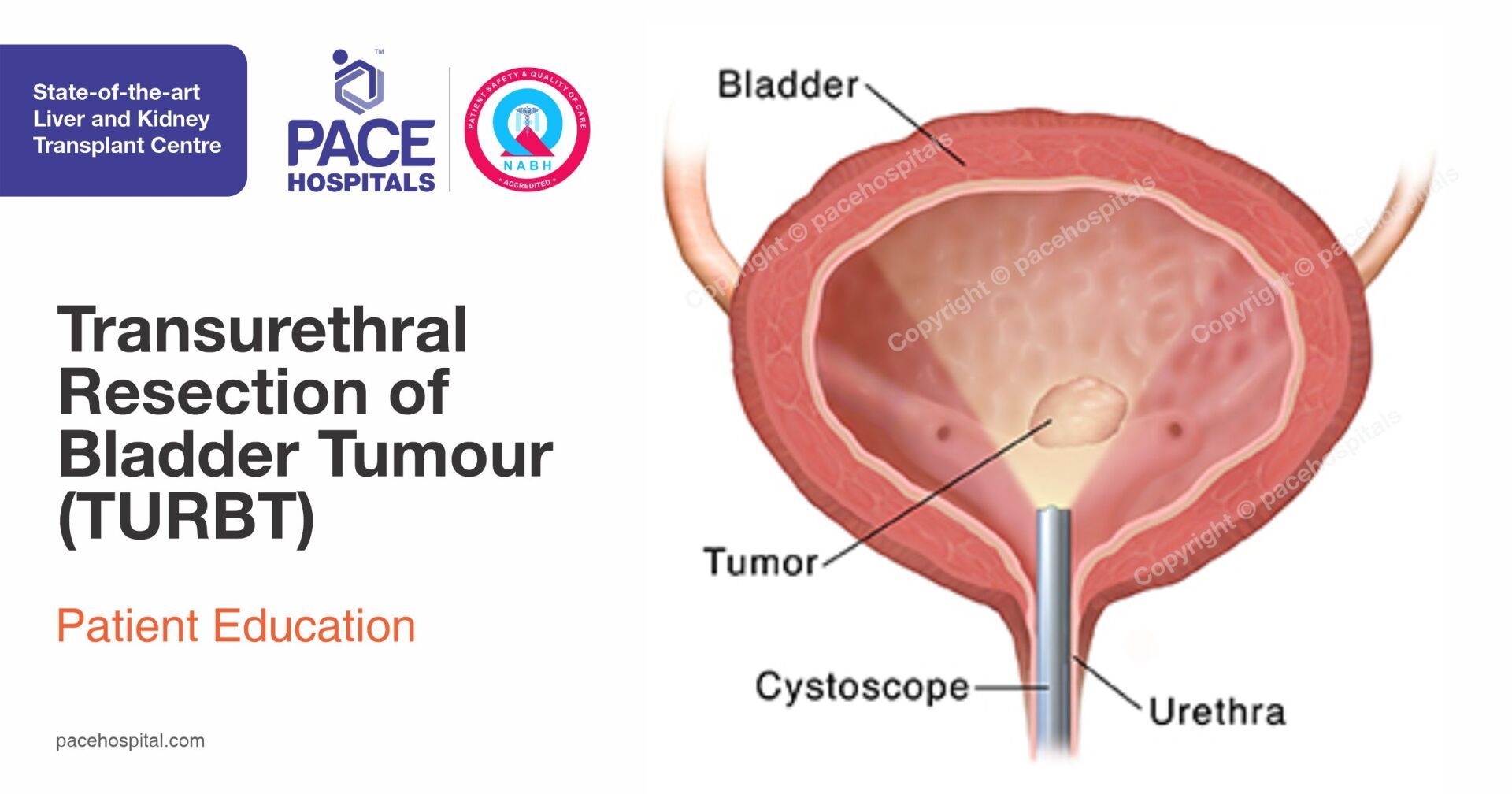
Your bladder is located in the lower part of your abdomen (tummy) and temporarily stores your urine. Urine is the waste fluid produced by your kidneys when they clean your blood. As the bladder fills with urine, its muscles allow it to expand, rather like a balloon. When your bladder is full, you get the urge to pass urine (urinate), which leaves the bladder and travels through your urethra, the tube that carries urine to the outside of your body. Pictured above: the urinary system.
What is cancer of the bladder?
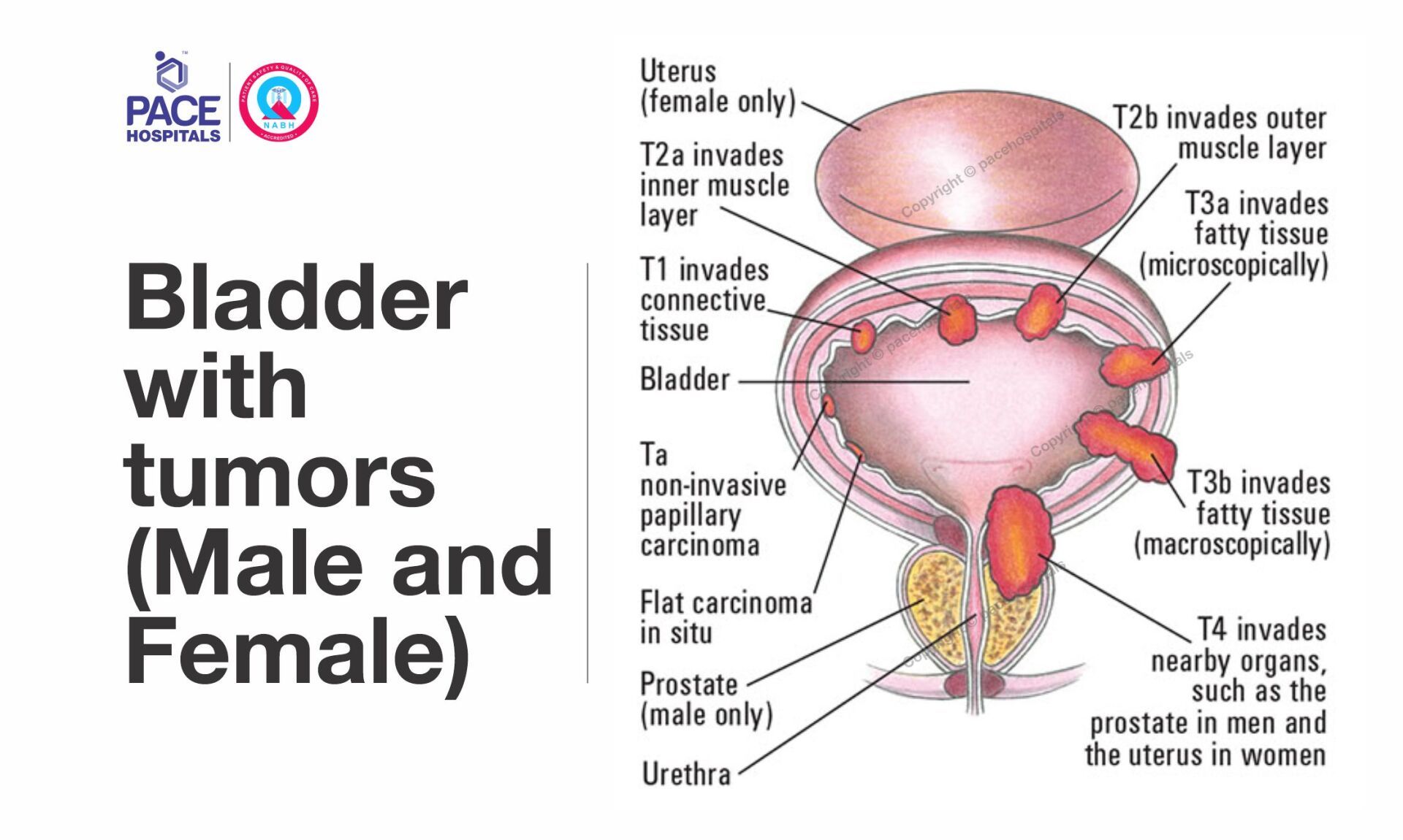
Bladder cancers grow and look like warts or mushrooms on the lining of the bladder. As they develop, they can put down deeper roots into the muscle wall of the bladder (this is called an invasive tumour). The majority of bladder cancers are called superficial (or non-muscle invasive) bladder cancers and are confined to the inner lining of the bladder only.
What is transurethral resection of a bladder tumour (TURBT)?
A transurethral resection of a bladder tumour or TURBT is a treatment for bladder tumours. This is an operation performed by a surgeon passing a camera (cystoscope) into your bladder through the water pipe (urethra). The bladder tumour can be visualised and removed via this camera and then sent for examination. From this, your consultant will be able to find out whether the tumour cells are cancerous and, if they are, the grade and stage the cancer has reached. This information can then be used to help decide any future treatment needed.
What are the benefits?
By removing the tumour we can help prevent any cancer spreading to other parts of your body. At the same time, we can also take a tissue sample (biopsy). By looking at this under a microscope, we can find out more about your condition and plan any further treatment you need.
What are the risks of surgery?
Although serious complications are rare, every surgical procedure has risks.Your doctor will discuss the specific risks for this procedure with you in more detail before asking you to sign the consent form.
Common side effects (greater than 1 in 10) which will ease over the first 10 – 14 days, include:
- Mild burning or bleeding. This is normal – one in ten patients do experience this. You will be encouraged to drink plenty of water to keep hydrated and flush your system.
- Blood clots in your bladder and urethra. This is normal and you may need a temporary catheter to flush out your bladder.
- Occasional side effects (between 1 in 10 and 1 in 50)
- Infection - this happens occasionally (in between one in 10 and one in 50 people). You will be given antibiotics to treat the infection if this occurs.
Rare (less than 1 in 50)
- Delayed bleeding needing removal of clots or further surgery
- An injured urethra (damage to the water pipe) causing scar formation
- Injury to the ureters (tubes that drain the kidneys)
- Perforation of the bladder(in less than one in 50 people) needing a longer time period with a catheter or open repair.
- Difficulty in passing urine directly after the operation – this is rare as most patients have a catheter for the first 48 hours after surgery.
- The surgeon will discuss this with you in detail before your operation, as part of the consent process.
Why do I need this procedure?
Benign bladder tumours usually grow very slowly. However, if they are not treated, they could become very large and cause problems by taking up too much space in your bladder or pressing on other organs in your body. Malignant tumours continue to grow unless they are removed. They can invade surrounding issue and spread to other areas of the body causing further problems. Cancerous tumours Bladder cancer occurs most commonly in people between 50 and 70 years of age. It is the fourth most common cancer in men and 13th most common in women. The most common symptom of bladder cancer is blood in the urine (haematuria). You may also have similar symptoms to having a urine infection, for example pain when you pass urine and the urge to pass urine frequently. The exact causes of bladder cancer are not known. However, you are more likely to develop bladder cancer if you:
- Smoke, as chemicals in tobacco enter the blood stream and are then filtered out by the kidneys. It is thought that these can cause damage to the bladder lining, which can lead to bladder cancer
- Have a history of bladder cancer in your family
- Previously worked in the dye chemical or print industry - certain chemicals that were used in these industries have been banned as they are now known to cause cancer
- Repeated bladder infections, for example cystitis
- Previously had bladder cancer.
Are there any alternatives?
Removing the tumour is the only reliable way to find out the type of tumour you have. If you do not have the operation and the tumour is superficial (just on the surface of your bladder), there is a risk that it will change into an invasive cancer. If the tumour is an invasive cancer, there is a risk that it will grow deeper into the tissues of your bladder and the cancer may spread to other parts of your body. Sometimes alternatives might include complete removal of your bladder (cystectomy), chemotherapy or radiation therapy.
What happens before the operation?
You will come into hospital either the evening before or the morning of your surgery. Most patients can leave hospital within 48 hours of their procedure. If you are taking any medication, these may need to be temporarily stopped or adjusted around the time of your surgery or treatment, you will be given information on how to do this at your pre-anesthesia check up. Do not make any changes to your usual medicines and continue to take them unless you have been advised to do so. Please remember to bring them into hospital with you. If you are taking any medicines that thin your blood, such as antiplatelet medicines (for example aspirin or clopidogrel) or anticoagulant medicines (for examples warfarin or rivaroxaban), please tell your doctor or the nurse as you may need to stop them temporarily before your procedure. Also tell your doctor or nurse if you have diabetes as you may need to alter the dose of your diabetes medicines, as you will need to fast before the procedure. Please let us know if you are taking any regular medicines (including anything you buy yourself over the counter or any herbal or homeopathic medicines) and if you have any allergies to any medicines. Further information on stopping any medicines will be given to you when you come for pre-assessment. Please ask us if you have any questions. Your consultant or registrar will see you on the night before or morning of your operation to discuss the surgery and answer any questions that you may still have. Please do not eat or drink anything for six hours before your appointment. This is because you should not have food or drink in your stomach when you are given the anaesthetic. If you do, you are more likely to be sick while you are unconscious, which can lead to complications. The nursing staff will tell you when you will need to stop eating and drinking. A member of the staff will then take you to the theatre.
Having an anaesthetic
TURBT is carried out under a general or spinal anaesthetic. A general anaesthetic will make you unconscious (asleep) during your operation, so you will not feel any pain. Anaesthetist will stay with you and monitor you during your surgery. A spinal anaesthetic is where a special needle is inserted into your back and anaesthetic medication is injected around the spinal nerves. This makes the lower part of your body completely numb, so you are unable to feel anything but you remain awake. You can also have sedation with this, which does not put you to sleep, but makes you feel drowsy. Your doctor will discuss the options with you before the operation.
During the operation
When you are anaesthetised your doctor will place a telescope (cystoscope or resectoscope) up your urethra and into your bladder. This is a special tube that allows your doctor to see your bladder lining. The visible tumour(s) will be cut away from the lining of your bladder wall using instruments inserted down the side-channels of the resectoscope. This can cause some bleeding. Once a tumour has been removed, any bleeding is prevented or reduced by using a mild electric current to cauterise (burn) the area where the tumour was. You will have a fine tube (catheter) inserted into your bladder to allow your bladder to empty and to remove any debris. Occasionally the catheter needs to be kept in for several days if the bleeding is persistent. It will be removed when your urine becomes rose-coloured or clear, before you leave hospital. Depending on the size of your tumour(s), the operation may take between 45 minutes and an hour. The tumour(s) will then be sent for examination.You may have a urinary catheter left in your bladder after your operation. This is a flexible tube that drains your urine into a bag outside your body. The catheter may also be used to flush out your bladder and wash away any blood clots after surgery. This means you may have a bag of sterile salt solution connected to the catheter which will flow into your bladder (called irrigation). This irrigation will be stopped once your urine runs clear.
- Once the operation is over, you will be taken to the recovery room to allow the anaesthetic to wear off. You will be taken back to the ward when you are fully awake and the nurses will encourage you to drink plenty of water.
- You may need to have the catheter in anywhere from 2-10 days, depending on what happens during the operation. For most people this is 5 days. Before you leave hospital, you will be given a date to return to hospital for the removal of your catheter. Our nurses will explain how to care for it and when and where to return to have it removed.
When can I go back to my normal activities?
You will usually be able to go home within 48-72 hours of your procedure. We advise you:
- To speak to your doctor about how much time you will need off work after your operation. This will depend on your recovery and the type of work that you do. Usually you will need to take about two weeks off, but if your job involves lifting or heavy work, you may need to take three to four weeks off work.
- To start gentle exercises about a week after your surgery, but please do not do anything too energetic, such as playing contact sports for a month.
- Not to drive again until you feel comfortable and are able to perform an emergency stop. Please check with your insurance provider before starting to drive again.
What if I have problems at home?
Some people experience a mild burning sensation on passing urine after their surgery. This usually settles after a few days. However, please contact the emergency, urology department if you:
- Develop a temperature (over 38°C), have pain and persistent burning when you pass urine
- Do not pass urine for six hours (unless you are asleep)
- Pass large clots of blood
- If you have persistent bleeding.
Your results
Your results should be available 5-7 days later. You will have to take an appointment for review, where your doctor will be able to review your results and discuss your future care. If you have bladder cancer and do not need any further invasive treatment you will need to have regular cystoscopies to check the cancer has not returned. These will initially be at three monthly intervals and then progressively less often if your bladder remains cancer free. If you need further treatment or your tumour(s) return, your doctor will discuss this with you at your follow-up appointment.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868