Urethral Stricture - Symptoms, Causes, Types, Treatment
Imagine a simple bodily function becoming a daily struggle, a routine task transformed into a painful ordeal. Urethral stricture—a silent menace—threatens to disrupt the rhythm of life for many, particularly men. From the mundane to the intimate, its effects ripple through daily existence, reminding us of the fragility of our bodies and the importance of understanding this often-overlooked condition.
A urethral stricture is the constriction of urethra, thereby causing symptoms of urine passage obstruction. Mostly, this stricture occurs due to the rupture of urethral mucosa and surrounded tissue. Though these urethral strictures can happen in both the genders, Men are more prone to it.
The causative factors of Urethral strictures differ based on the regional discrepancies. Besides infection, the urethral strictures can also happen due to unknown reasons (Idiopathic) or even due to unintentional mistakes by physicians (Iatrogenic) with 41% and 35% probability respectively.
As haematological tests do not have any role in this disease’s diagnosis, the urologist initiates the diagnosis by physical examination, Urine Analysis and through symptoms. However, retrograde urethrography or cystoscopy diagnostic procedures are performed to confirm the disease.
The primary goal of therapy should be to alleviate the symptoms if there are no complications. The symptomatic relief can be achieved by choosing the therapy based on the severity of symptoms, stricture dimension and location. The symptoms like relapse of infections or abrupt retention requires therapy to avoid further complications and lower the damage to the lower urinary tract. If the diagnosis is not clear about the possibility of infection, antibiotics can be prescribed initially and checked for symptomatic relief. Urethral dilation, direct vision internal urethrotomy, Paclitaxel-coated urethral balloon dilation therapy are few therapeutic approaches in case of confirmed infection of urethral strictures.
Retrograde urethrograms, with or without voiding cystourethrograms, are the preferred diagnostic studies for male urethral strictures, while uroflowmetry is preferred for follow-up testing after treatment.
If the symptoms of this infection are ignored, complications like acute urinary retention, bladder diverticulum, erectile dysfunction etc. can occur. The incidence of urethral strictures can be minimized by educating the patient to avoid pelvic or penile trauma, self- catheterization having protected inter course etc.
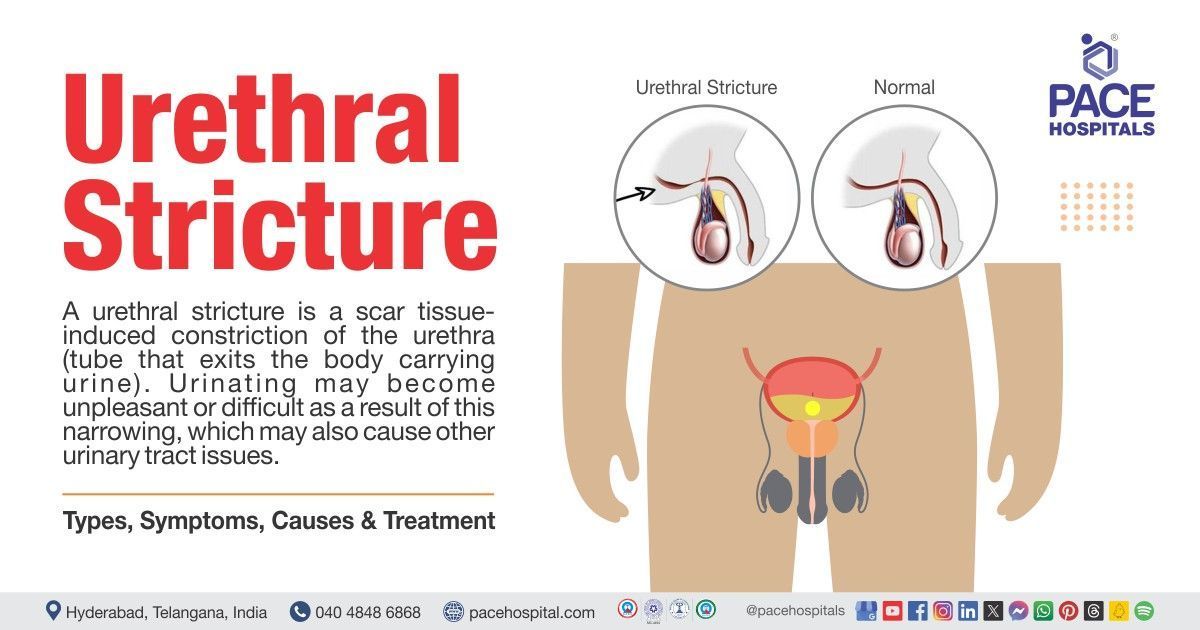
Urethral stricture definition
Urethral stricture is defined as a medical condition that is characterized by a narrowed urethra due to scarring of the tissue. This urethral constriction cause urine obstruction and may lead to urinary symptoms such as decreased urine flow, discomfort, incomplete bladder emptying, and higher risk of infection.
Urethral stricture meaning
Urethral stricture has two words in which
- ‘Urethral’ is derived from a Greek word ‘ourethra’ which means ‘a canal through which urine is discharged from the bladder’.
- ‘Stricture’ is derived from a Latin word ‘strictura’ that is used to describe ‘abnormal narrowing in a body part’
Prevalence of urethral stricture
Urethral stricture illness is a frequent and difficult urologic ailment that affects people of all ages, primarily men with a corresponding incidence of 229–627 per 100,000 men. This condition is seen rare in female genders with prevalence of 3-8 % world-wide and 4–13% in women who are already with a medical condition known as bladder outlet obstruction.
The yearly incidence rate of urethral constriction is estimated to be 200 to 1200 instances per 100,000 people, with much higher rates among those over the age of 55 years. The frequency of urethral stricture in industrialised countries is believed to be around 0.9%.
Prevalence of urethral stricture in India
Urinary strictures affect 4–10 persons out of every 1,000 in India, with males over 50 years of age having the highest prevalence of the illness. A study conducted in Indian population demonstrated that iatrogenic and idiopathic strictures are more prevalent.
Types of urethral stricture
The Urethral strictures are primarily classified based on their location and its tightness in male and female patients.
According to location:.
Urethral strictures in males are distinguished based on anterior and posterior urethra.
Anterior urethra
The Anterior urethra extends from meatus till urogenital diaphragm. Corpus spongiosum surrounds the anterior urethra throughout its length and in turn subdivided in different locations like:
- Meatal strictures
- Penile strictures
- Bulbar strictures
- Penobulbar strictures
- Meatal urethral Strictures: The Meatal strictures are situated at the external urethral meatus and might stretch into fossa navicularis of the glans.
- Penile urethral stricture: These are observed in a zone between fossa navicularis and bulbar urethra. Balanopreputial sulcus is the origin point of penile urethra externally and extends upto penosctoal junction. Carpora vernosa is the ventral groove having whole penile urethral segment which is surrounded by a lean layer of Corpus spongiosum.
- Bulbar urethral strictures: Bulbospongious muscle surrounds the penoscrotal junction. This junction is the starting point of Bulbospongious muscle and ends in the urethra membranous at the urogenital diaphragm level proximally. The bulbar urethra can be differentiated into proximal and distal parts. If the segment is within 5 cm of urethral membrane, it is called proximal bulbar urethra. The adjoining segment extending to the penoscrotal junction is distal bulbar urethra.
- Penobulbar urethral strictures: These strictures lie between penile urethra and bulbar segment, possessing long urethral segments.
Posterior urethra:
It is approximately 5cm long, bearing three different segments.
- The section of the urethra that passes through the urogenital diaphragm between the distal verumontanum and the proximal bulbar is known as the membranous urethra.
- Originating at the proximal membranous urethra and extending to the bladder neck, the prostatic urethra passes through the prostatic gland.
- The internal urinary sphincter, which connects the bladder to the prostatic urethra, encircles the neck of the bladder. A prostate in situ is implied by stenosis (or contracture) of the bladder neck (i.e., following TURP or simple prostatectomies). The proper name is VUAS if the narrowing or obliteration occurs at this level but following an RP.
In Female, the urethra is randomly divided into an upper, middle and lower section and is around 4cm long.
According to stricture tightness
Over the years, various systems of classification have been put forth. There is disagreement over the distinction between low-grade and high-grade strictures.
A high-grade or tight structure is defined as a urethral plate measuring less than 3 mm. It has been shown that the flow rate will not decrease in a bladder that has been functioning properly until the urethral lumen reaches a diameter of less than 10 Fr.
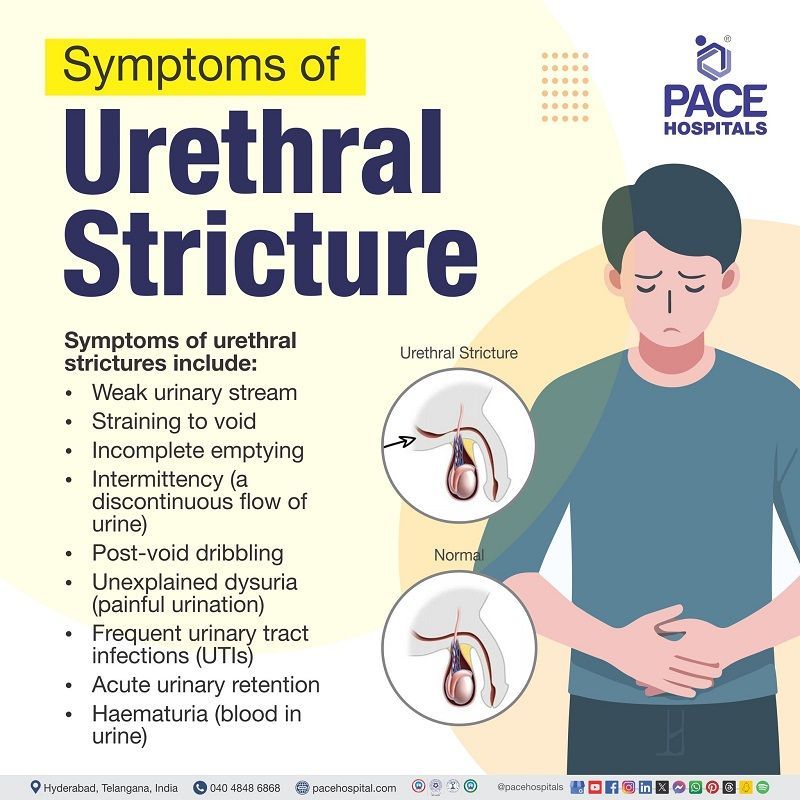
Urethral stricture symptoms
Patients, particularly those who have a discrete or slowly developing stricture, can have a wide range of symptom intensity. There are others who may not exhibit any of the symptoms. The symptoms of this condition may resemble with those commonly linked to obstruction of the bladder outflow caused by benign prostatic hyperplasia (BPH).
Symptoms of urethral stricture may include:
- Weak urinary stream
- Straining to void
- Incomplete emptying
- Intermittency (a discontinuous flow of urine)
- Post-void dribbling
- Unexplained dysuria (painful urination)
- Frequent urinary tract infections (UTIs)
- Acute urinary retention
- Hematuria (blood in urine)
One symptom that distinguishes urethral stricture disease from benign prostatic hyperplasia is obstructed ejaculation.
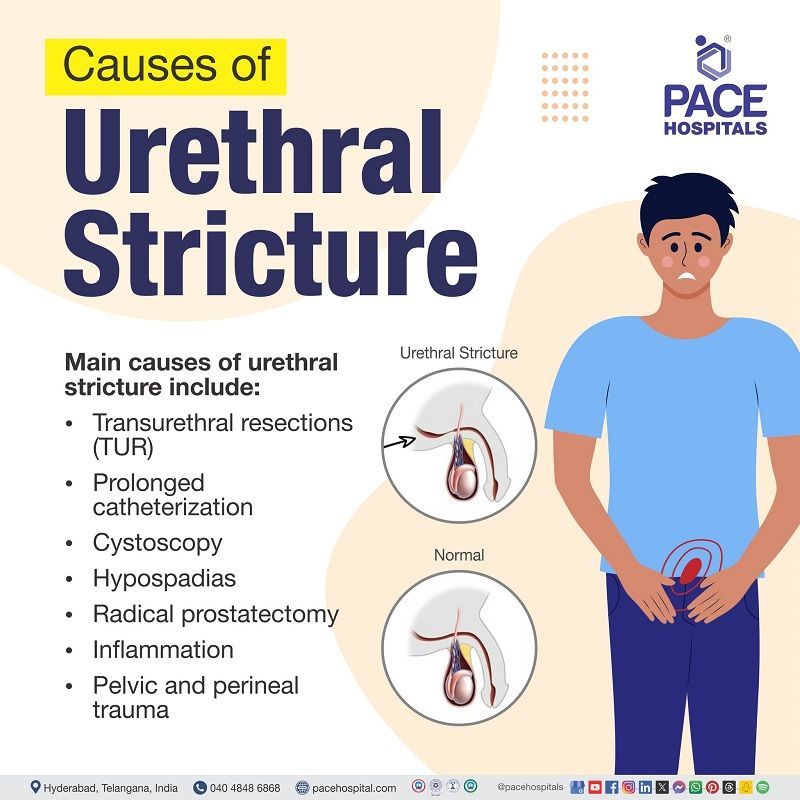
Urethral stricture causes
The four main causes of urethral strictures are idiopathic (unknown cause), iatrogenic disease caused by a medical examination or treatment), inflammatory, and traumatic, with idiopathic and iatrogenic accounting for 33% of cases. The traumatic causes follow next, making up 19%, and the inflammatory causes, making up 15%.
Iatrogenic Causes
There are five types for iatrogenic causes which include:
- Transurethral resections (TUR): About 41% of all iatrogenic strictures are transurethral resections. Urethral stretching and dilatation during these procedures results in variable degrees of epithelial damage due to the frequent passing of relatively large tools in and out of the urethra. A stricture eventually forms because of this urethral mucosal damage.
- Prolonged catheterization: A prolonged catheterization which accounts for 36% might cause pressure necrosis of the urothelium and rubbing or frictional irritation to the urethral mucosa due to the motion of the catheter. Strictures may occur due to prolonged periods of intermittent catheterization.
- Cystoscopy: improper and disorganized removal of foley catheters that are used in cystoscopy procedure can cause stricture formation due to injury to the urethral epithelial tissue.
- Hypospadias: 6.3% of iatrogenic strictures result with hypospadias repair. Urethral stricture development is 10% more likely in children who have this type of treatment.
- Radical prostatectomy: it is said that 8.4% of men receiving treatment for prostate cancer, such as surgery, radiation, and chemotherapy, experience urethral strictures complication in the posterior or bulbar urethra and bladder neck.
Inflammation
It is demonstrated that urethral strictures can arise due to post infectious inflammation resulting in the lumen's narrowing and the epithelium's deterioration. There are indications that schistosomiasis, chlamydia, and tuberculosis may induce postinfectious inflammation and cause urethral stricture development.
Pelvic and perineal trauma
Straddle injuries (injuries to the groin area) are a common cause of trauma to the anterior urethra. If the perineum is hit sharply, this can happen. The urethra may become scarred and eventually lead to urethral strictures by this kind of trauma.
Urethral stricture risk factors
Common risk factors for developing a urethral stricture may include:
- Transurethral surgery:
After transurethral resection of the prostate, urethral strictures are one of the most common late consequences and the main source of iatrogenic urethral strictures in patients over 45 years of age who had urethroplasty.
- Urethral catheterization:
An inflammatory response resulting in stricture formation of the urethral mucosa is another danger associated with the use of indwelling catheters.
- Prostate cancer treatment: Due to the near proximity to the urethral sphincter and the reduced capacity for tissue repair, urethral stricture following radiation therapy for localized prostate cancer is a delicate issue that makes any surgical approach more difficult. Furthermore, the management of radiation-induced urethral strictures is difficult and requires certain surgical expertise because of its unique pathophysiology. Hence patients who undergo prostate cancer treatment are at risk of developing urinary strictures.
- History of hypospadias repair:
It is demonstrated that for men under 45, urethral stricture illness is frequently caused by hypospadias repair. Up to 72% of people who have trouble urinating after having their hypopadias repaired as children may experience it.
- Lichen sclerosus (LS):
Both men and women may experience urethral stricture because of lichen sclerosus (LS), particularly in the anogenital area. Urethral stricture illness can result from inflammation and scarring caused by lichen sclerosis in the genitals and urethra.
Urethral stricture complications
In case of untreated urethral strictures, it can eventually cause complications such as:
- Urinary retention
- Bilateral and unilateral vesicoureteral reflux (back flow of urine)
- Bladder diverticulum (protruded bladder out of the bladder wall)
- Erectile dysfunction
- Penile curvature or shortening
- Recurrent urinary tract infections (UTIs)
- Voiding dysfunction (inability to empty bladder fully)
- Urethrocutaneous fistula undesired holes between the perineum (the skin in the groin area) and the urethra (where a person's urine exits).
Urethral stricture prevention
Although it is not possible to prevent every cause, there are activities that can be taken to lower the risk which may include:
- Avoiding injuries to urethra and pelvic region: In case of an unrecognized urethral or pelvic injury, issues arise, and urethra may be damaged further due to blind catheterization. Recurrent stricture rates increase in those cases and future reconstruction may be affected.
- Being cautious during self-catheterization: There is a significant risk of developing inflammation in the urethra and eventually lead to formation of scar tissue due to improper self-catheterization. Hence using a lubricating jelly and using a shortest catheter may help in preventing urethral strictures.
- Avoiding sexually transmitted diseases:
Sexually transmitted infections, such as gonorrhoea etc, can inflame and infect urethra, resulting in stricture and scarring eventually.
Urethral stricture diagnosis
When diagnosing urethral strictures, blood tests are irrelevant. Firstly, the urethral stricture diagnosis is suggested by the past medical history and physical examination, The diagnosis is established by:
- Uroflowmetry
- Urinalysis
- Post-void residual urine volume
- Cystoscopy
- Retrograde urethrography
- Ultrasonography
- Magnetic resonance imaging (MRI)
- Computed tomography
- Intravenous pyelography (IVP)
Urethral stricture treatment
Presently there are no approved medical managements available for this condition. This can only be managed by surgical interventions which are generally classified as endoscopic and open surgical procedures.
Endoscopic surgical interventions may include:
- Urethral dilation
- Internal urethrotomy
Open surgical interventions may include:
- Stricture resection
- Anastomosis
- Urethroplasty
- Perineal urethrostomy
- Urethral stents
Difference between urethral strictures and benign prostatic hyperplasia (BPH)
Since urethral strictures and benign prostatic hyperplasia symptoms resembles closely, it is important to understand the basic differences between these two conditions:
| Parameter | Urethral strictures | Benign prostatic hyperplasia |
|---|---|---|
| Meaning | Unusual urethral narrowing is known as urethral stricture. | Benign prostatic hyperplasia also known as prostate enlargement is a non-cancerous increase in size od prostate gland |
| Symptoms | Weak urinary stream, Straining to void, Incomplete emptying, Intermittency (a discontinuous flow of urine) etc. | One symptom that distinguishes urethral stricture illness (present) from BPH (absent) is obstructed ejaculation. |
| Causes | Medical procedures, Urethral cancer, Sexually transmitted infections, Radiation, Pelvic trauma, Enlarged prostate | The exact cause of this condition is unknown. Nevertheless, some established causes include: Hormonal imbalance, Prolonged NSAID use, Increased age, Inflammation in the body |
| Treatment | There is no established medical management of urethral strictures. However, there are approved surgical interventions to treat this condition which may include: Urethral dilation, Internal urethrotomy, Stricture resection, Anastomosis , Urethroplasty, Perineal urethrostomy , Urethral stents. | Medical management: Alpha adrenergic antagonists, 5 alpha reductase inhibitors, Phosphodiesterase (PDE-5) inhibitors. Surgical management: Prostatectomy, Laser surgery, Aquablation, Prostatic urethral lift. |
Benign prostatic hyperplasia occurs only in men while urethral strictures may occur in both men and women.
Frequently Asked Questions (FAQs) on Urethral stricture
How to prevent urethral stricture recurrence?
The recurrence of this condition may be prevented by:
- Avoiding urethra and pelvis related injuries
- Careful self-catheterization.
- Using lubricating jelly
- Using smallest possible catheter
- Avoiding sexually transmitted diseases
Can urethral stricture effect testicles?
A urethral stricture can affect the testicles. Untreated urethral strictures can lead to conditions such as epididymitis and testicular infections.
Does urethral stricture affect ejaculation?
Yes. Individuals suffering with urethral stricture usually report inadequate ejaculation force, decreased ejaculatory volume, decreased pleasure, or no ejaculation at all. Pre-operative problems are more common in elderly patients and their severity varies with patient age.
Can urethral stricture cause erectile dysfunction?
Yes. compared to healthy men, patients with urethral stricture experience erectile dysfunction at a higher rate. Regardless of the length or location of the stricture, appropriate therapy shouldn't have a major detrimental effect on erectile function, while it might have some effect on the anatomy of the penis.
Does urethral stricture cause kidney damage?
Yes. There will be symptoms when a stricture is narrow enough to reduce urine flow. Urinary tract infections (UTIs), prostate enlargement, and infections are possible side effects. Long-lasting, severe obstruction may damage the kidneys.
what is urethral stricture?
Urethral stricture, is scarring of the urethra, the tube that drains urine from the body. Urination becomes challenging due to the urethra's blockage or narrowing caused by scarring. Urethral strictures can cause kidney stones, infections, and problems with the urinary tract if they are not treated.
How often do urethral strictures reoccur?
A study demonstrated that the recurrence rate of urethral strictures is between 2%-40%.
Can urethral strictures heal on their own?
Through understanding how to dilate the urethra at home, it might help to treat the stricture. Surgery can be necessary if urethral dilation is unable to treat the issue. The stricture's length and placement will determine the kind of surgery needed.
What is the pathophysiology of urethral strictures?
Urethral stricture pathophysiology involves inflammatory, ischemic, or traumatic processes. These procedures result in the development of scar tissue, which constricts and lowers the urethral lumen's calibre, preventing the urine from flowing in a forward direction.
Is urethral stricture painful?
Urethral stricture disease frequently causes lower urinary tract pain, particularly in younger men. It is linked to reduced voiding function and a lower quality of life. After urethral repair, lower urinary tract pain usually goes away in men.
Can someone urinate normally having a stricture?
No. Urethral strictures cause scarring of the urethra which narrows it making difficult to urinate. Urinating when having a stricture can cause pain during urination.
What is the gold standard treatment for urethral strictures?
Urethroplasty is regarded as the gold standard of urethral stricture treatments when carried out by a qualified specialist, with a long-term success rate ranging from 80% to 95% depending on the procedure.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Popular Articles