Angina Pectoris – Symptoms, Types, Causes, Treatment & Prevention
Angina pectoris definition
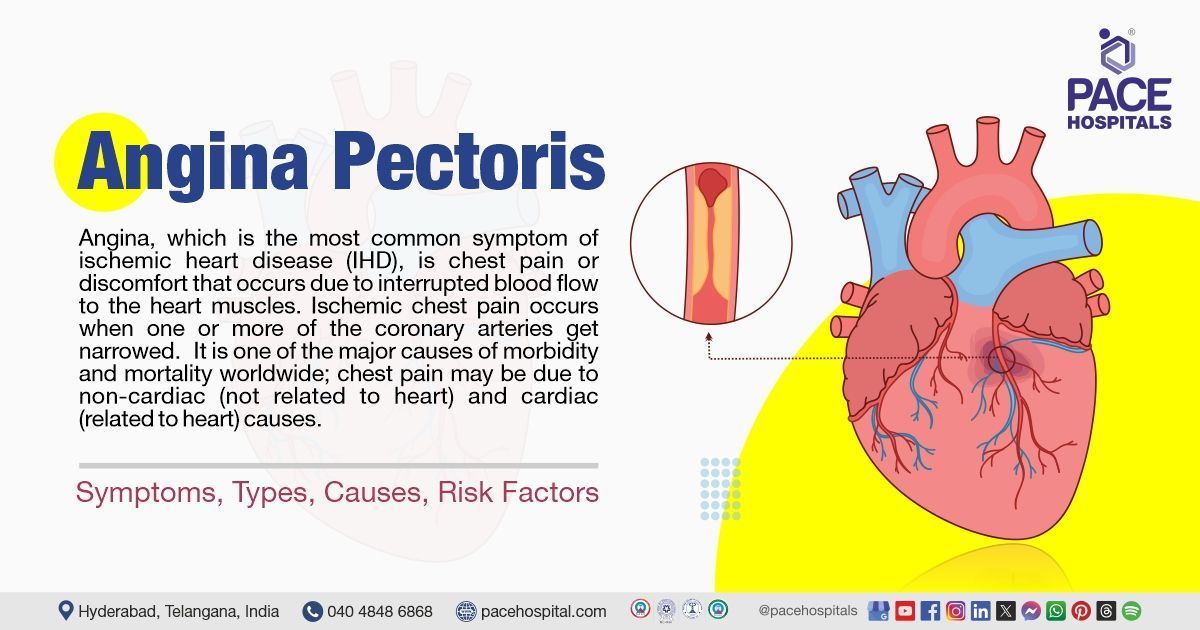
Angina, which is the most common symptom of ischemic heart disease (IHD), is chest pain or discomfort that occurs due to reduced blood flow to the heart muscles. Ischemic chest pain occurs when one or more of the coronary arteries gets narrowed. It is one of the major causes of morbidity and mortality worldwide; chest pain may be due to non-cardiac (not related to heart) and cardiac (related to heart) causes. Stable angina, unstable angina, microvascular angina, and vasospastic or variant angina are the four different types of angins.
The treatment of angina is aimed at managing symptoms and preventing the progression of cardiac events. Management is multifactorial and requires a few lifestyle modifications to prevent further complications. A
cardiologist can treat angina.
Angina pectoris meaning
The term angina pectoris is derived from Latin, the term “angere” means to strangle and “pectoris” means chest; together it means strangling (pressure) feeling in the chest.
Prevalence of angina pectoris
Prevalence of angina worldwide
Angina is one of the most common symptoms of ischemic heart disease. Symptoms of angina are seen in approximately 90 lakhs of patients in the US. The prevalence of angina increases with age in both men and women. In Western countries stable angina affects approximately 30000 to 40000 people per 10 lakh people. The estimated prevalence for men and women aged 45 to 64 years are 4 to 7 percent and 5 to 7 percent respectively. In men and women aged 65 to 84 years, the prevalence is 14 to 15 percent and 10 to 12 percent, respectively.
Prevalence of angina in India
As per the CLARIFY study, which is an international, prospective-observational, longitudinal cohort study in stable coronary artery disease outpatients the prevalence of angina in India decreased from 27.8% to 11.2% over a 5-year period. From recent studies it is estimated that the proportion of symptom-based angina is 4.69% in older males and 7.02% in older females.

Types of angina pectoris
Angina is not a disease itself, but it is a symptom of an underlying condition, usually coronary artery disease. There are five main types of anginas which include stable angina, unstable angina, microvascular, vasospastic or variant angina, and refractory angina. Based on the type of angina, many factors can trigger pain. The 5 types of anginas are described below:
- Stable angina: Angina pectoris, also called stable angina, is a chest pain that occurs due to interrupted blood supply to heart muscles because of the narrowing of coronary arteries. It usually causes uncomfortable pressure, fullness, squeezing, or pain in the center of the chest.
- Unstable angina: It is one of the several acute coronary syndromes that occur while resting and causes unexpected chest pain. It does not go away with rest and should be treated as an emergency as it may be a sign of a heart attack and can even lead to cardiac arrest.
- Variant angina: It is also called Prinzmetal angina; it does not occur with physical exertion or emotional stress. The pain is very painful and occurs when the individual is resting, usually between midnight and early morning.
- Microvascular angina: This type of angina is usually a symptom of coronary microvascular disease which is a heart disease affecting the smallest coronary artery blood vessel.
- Refractory angina: It is a chronic and persistent form of angina that occurs when the heart's demand for oxygen exceeds its supply, despite optimal medical therapy. It is characterized by frequent episodes of chest pain that cannot be controlled adequately by medications and revascularization therapy.
Angina pectoris symptoms
Symptoms of angina vary based on the type and they may differ in severity, location, timing, and degree of relief. The primary symptom of angina is chest pain or discomfort. The pain in angina can feel like pressure, tightness, discomfort, squeezing, heaviness, or burning sensation in the chest. The common symptoms of angina include:
- Shortness of breath (SOB)
- Extreme fatigue (tiredness)
- Fainting or light headedness
- Nausea
- Heartburn
- Weakness
- Sweating
Stable angina symptoms
The pain in stable angina:
- Occurs usually during physical exertion
- Lasts for a short period
- Pain can be relieved by taking rest and with the use of medications
- The pain feels like a gas or indigestion
- It may feel like the pain is spreading to the arms and back.
Unstable angina symptoms
The pain in unstable angina:
- Usually occurs during physical exertion or while resting or sleeping
- It can be sudden
- Lasts longer than stable angina
- Does not get relieved by rest or with medicines
- Worsens over time, it can lead to heart attack
Variant angina symptoms
The pain:
- Develops while resting usually between midnight or early morning
- Is severe
- Gets relieved with the use of medications
Microvascular angina symptoms
The pain:
- Is more severe and lasts longer than all the other types of anginas
- Accompanies shortness of breath
- It is first noticed with routine physical activities
Refractory angina symptoms
The pain:
- Is severe and the symptoms last for more than 3 months
- Pain cannot be managed with medicines or other treatments.
Angina symptoms in women
Symptoms of angina can be different in men and women. Women can feel pain in the areas far from the source of pain such as arms, neck, back, and jaw. They can also present symptoms like shortness of breath, nausea, and lightheadedness.
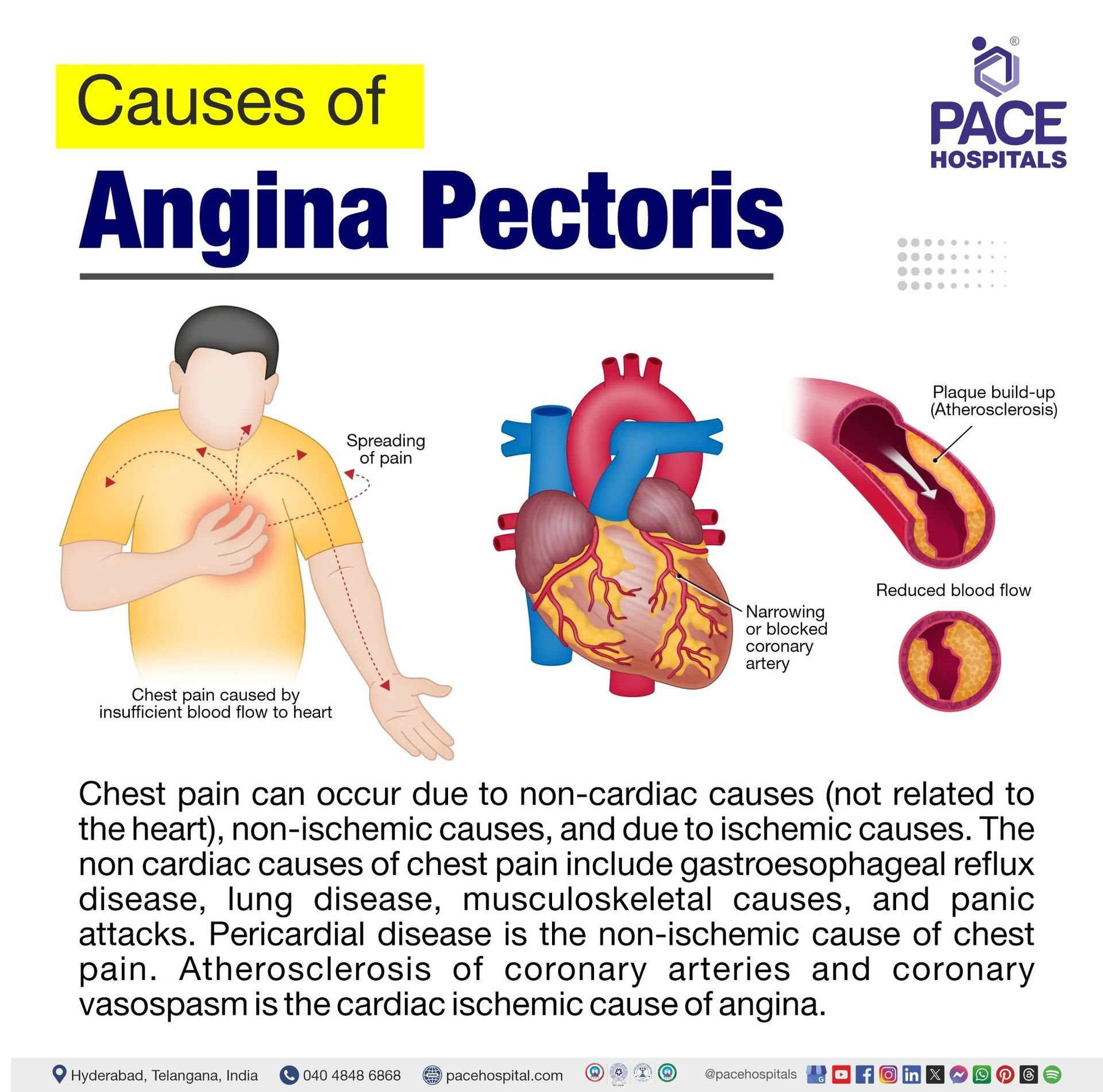
Angina pectoris causes
Chest pain can occur due to non-cardiac causes (not related to the heart), non-ischemic causes, and due to ischemic causes. The non cardiac causes of chest pain include
gastroesophageal reflux disease (GERD), lung disease, musculoskeletal causes, and panic attacks. Pericardial disease is the non-ischemic cause of chest pain. Atherosclerosis of coronary arteries and coronary vasospasm is the cardiac ischemic cause of angina.
Angina causes
Angina is not a disease but a symptom of an underlying heart condition. Coronary artery disease which is a medical cardiac condition can cause angina. The type of angina depends on the condition causing it. Following are the types of anginas and their causes:
Stable angina causes
This type of chest pain occurs when the heart muscles do not get a sufficient amount of blood or when the heart requires more blood, such as during physical activity like climbing a hill or stairs or when experiencing strong emotions.
Unstable angina causes
Plaque builds up within the arteries thereby narrowing the blood vessel. This plague buildup causes damage to areas, making it easier for blood clots to form. Partial or total blockage from blood clots causes unstable angina.
Variant angina causes
The chest pain that develops in variant angina is caused by coronary artery spasm. The spasm in coronary arteries is caused by stress, exposure to cold weather, use of medications that narrow blood vessels, smoking, and consumption of cocaine.
Microvascular causes
Development of spasms in the very small arterial blood vessels causes microvascular angina. This spasm interrupts or blocks the supply of blood flow to the heart vessels causing pain.
Angina pectoris risk factors
A risk factor is a factor or a variable that increases the likelihood of developing a disease. There are several factors that increase the risk of angina development. Following are some of the risk factors of angina:
- Age: The risk of heart disease increases with age. With increasing age, the plague builds up in the arteries interrupting the blood supply to the heart muscle.
- Environment or occupation: Particle pollution that includes dust from roads, farms, dry riverbeds, construction sites, and mines is linked to angina. Professional life with inadequate sleep, stress, long periods of sitting or standing, or exposure to radiation can increase the risk of angina.
- Family history and genetics: Heart diseases run in families. Individuals with no lifestyle-related risk factors develop heart diseases due to the involvement of genes. Thus, genetics increases the risk of angina.
- Lifestyle habits: Lifestyle related risk factors include excessive alcohol consumption, lack of physical activity, smoking, stress, and unhealthy dietary habits.
- Medical conditions: Conditions like anemia, cardiomyopathy, heart valve diseases, hypertension, heart failure, and metabolic syndrome increase the risk of angina.
- Medical procedures: Past medical procedures like stent placement, and coronary artery bypass grafting trigger coronary spasms and angina.
- Race: Black or African American people with a past medical history of heart attack have a higher chance of developing angina compared to white people. People living in Japan have a higher risk of developing vasospastic angina.
- Sex: Angina affects both men and women. Heart diseases tend to rise in men aged above 45 years, women have a lower risk of heart disease below the age of 55 years. The risk of heart disease is equal when both men and women are aged 55.
Complications of angina pectoris
Though angina is not life threatening it is a major cause of morbidity and mortality as it causes some serious complications. There are several complications of angina pectoris. Cardiac events such as myocardial infarction and heart attack are the two main complications of angina.
The possible complications of angina include:
- Abnormal heart rhythms: In angina, the insufficient blood supply to the heart muscles disrupts the electrical activity of the heart thereby causing arrhythmias (abnormal heart rhythm).
- Heart attack: The insufficient blood supply to heart muscles due to the narrowing of coronary arteries causing the heart muscles to die thereby leading to heart attack.
- Heart failure: Repeated episodes of angina weaken the muscles of the heart and increase the risk of heart attack.
Angina pectoris diagnosis
Diagnosis of angina is clinical, and it is based on a detailed history of the characteristics of the pain, with an assessment of its quality, frequency, location, severity, duration, and associated symptoms to assess triggering and alleviating factors. Diagnosis of angina includes the following steps:
Initial evaluation
- Medical history
- Physical examination
Diagnostic tests
- Chest X-ray
- Electrocardiogram (ECG)
- Blood tests
- Complete blood count (CBC)
- Basic metabolic profile (BMP) that includes troponin levels
- Stress testing
- Exercise stress testing
- Pharmacological stress testing
- Other diagnostic studies
- Echocardiogram
- Cardiac magnetic resonance imaging
- Coronary computed tomography angiography (CCTA)
- Invasive coronary angiography
Angina pectoris treatment
Angina pectoris treatment approach is based on the type of angina, the presenting symptoms, the test results, and the risk of complications. Management of angina is multifactorial and involves lifestyle changes, risk factor modification, and medical therapy as essential components of treatment.
Nonpharmacological management of angina
When the symptoms are stable and not getting worse then angina can be managed with certain lifestyle modifications or changes. Below are some of the measures listed by following which angina can be managed:
- Choosing a diet that is heart healthy
- Maintaining an ideal body weight
- Staying physically active
- Managing stress
- Avoiding smoking
- Getting enough sleep
Pharmacological management of angina
Angina pectoris treatment usually involves two approaches; one is to increase the blood flow to the heart muscles and the other is to lower the workload of the heart. Following are the medications that are used in treating angina:
- Beta blockers
- Nitrates
- Calcium channel blockers
- Antiplatelets
- Anticoagulants
- Statins
- Antianginal
- Narcotic analgesic
Revascularization procedures
If angina is not managed through lifestyle modifications and with medications following medical procedures are recommended:
- Coronary artery bypass grafting (CABG)
- Percutaneous coronary intervention (PCI)
Angina pectoris prevention
Angina prevention usually involves lowering the risk of heart disease by adopting heart healthy lifestyle modifications. These heart-healthy lifestyle modifications include:
- Dietary modifications: Including a diet that is rich in fiber, including fruit and vegetables in the diet. Limiting alcohol consumption and avoiding high-fat content food.
- Exercise: Being physically active, exercising regularly for at least 30 minutes
- Maintaining ideal body weight: If overweight or obese, weight reduction becomes crucial.
- Quit smoking: Avoiding smoking or gradually decreasing alcohol consumption
- Managing stress: Avoiding situations that trigger stress
- Healthy sleeping habits: Getting enough sleep helps repair heart muscles.
- Adhering to medications: It is important to adhere to the medications prescribed to manage symptoms.
- Treating underlying medical conditions: Underlying medical conditions like hypertension, diabetes, and dyslipidemia can increase the risk of angina therefore they have to be treated.
Difference between stable angina and unstable angina
Stable angina v/s unstable angina
Stable and unstable angina are the two main types of angina pectoris. Though they have similarities there are some key differences that differentiate stable angina from unstable angina. Below are some parameters that differentiate between the two:
| Parameters | Stable angina | Unstable angina |
|---|---|---|
| Definition | Angina pectoris, also called stable angina, is a chest pain that occurs due to interrupted blood supply to heart muscles because of the narrowing of coronary arteries. | It is one of the several acute coronary syndromes which occur while resting and causes unexpected chest pain. |
| Causes | It occurs when the heart muscles do not get a sufficient amount of blood or in cases where the heart requires more amount of blood such as during physical activity like climbing a hill or stairs, or when having strong emotions | Plaque builds up within the arteries thereby narrowing the blood vessel. This plague buildup causes damage to areas, making it easier for blood clots to form. Partial or total blockage from blood clots causes unstable angina |
| Symptoms | Chest pain occurs usually during physical exertion which lasts for a short period. Pain can be relieved by taking rest and with the use of medications | The ischemic chest pain usually occurs during physical exertion or while resting or sleeping |
| Treatment | Pain can be relieved by taking rest and with the use of medications | The pain does not go away with rest, and it requires immediate medical action as it is a medical emergency |
Difference between angina and myocardial infarction
angina pectoris vs myocardial infarction
Angina and myocardial infarction are both related to the heart, but they have different characteristics. Following are some of the key parameters that differentiate angina from myocardial infarction
| Parameters | Angina | Myocardial infarction |
|---|---|---|
| Definition | Angina pectoris, also called is a chest pain that occurs due to interrupted blood supply to heart muscles because of the narrowing of coronary arteries. | Myocardial infarction also called a heart attack is a result of decreased or complete blockage of blood flow to a part of the myocardium . |
| Causes | It occurs when the heart muscles do not get a sufficient amount of blood or in cases where the heart requires more amount of blood such as during physical activity like climbing a hill or stairs, or when having strong emotions | Underlying coronary artery disease is the primary cause of myocardial infarction. |
| Symptoms | Chest pain occurs usually during physical exertion which lasts for a short period. Pain can be relieved by taking rest and with the use of medications | It can present chest pain, upper extremity pain, and epigastric discomfort that occurs during exertion or at rest. |
| Treatment | Treatment is multifactorial and involves lifestyle modifications, drug therapy, and revascularization procedures. | Treatment includes lifestyle modification, drug therapy, and medical procedures such as reperfusion therapy and primary percutaneous intervention. |
Frequently Asked Questions (FAQs) on Angina pectoris
Is angina a disease or a symptom?
Angina is not a disease itself; it is a symptom of an underlying condition. It occurs when muscles of the heart do not get sufficient oxygen-rich blood due to the narrowing of coronary arteries. The pain usually occurs during physical exercise and lasts for a shorter period.
Is angina curable?
No, angina is not curable, but it can be managed. It can be managed by lifestyle modifications, medical therapy, and revascularization procedures. Treatment is important to prevent angina attacks and reduces the further risks of heart attacks and infarctions.
Is angina pain constant?
No, angina pain is not constant. The pain can vary with each type of angina, and it typically stops and starts and can last from seconds to minutes. This pain usually occurs when the heart is working hard.
Can angina lead to myocardial infarction?
Yes, angina can lead to myocardial infarction. It is one of the primary symptoms of coronary artery disease; studies estimated that a 10-year risk of myocardial infarction exceeded 10 percent in women with stable angina.
How is angina treated?
The pharmacological treatment approach is based on the type of angina, the presenting symptoms, the test results, and the risk of complications. It involves two approaches; one is to increase the blood flow to the heart muscles and the other is to lower the workload of the heart. Drug classes such as beta blockers, nitrates, calcium channel blockers, antiplatelets, anticoagulants, and statins are used in treating angina.
Can ECG detect angina?
Yes, ECG can diagnose angina. It helps in recognizing the type of angina and other heart related conditions. Certain ECG patterns are signs of unstable and vasospastic angina. At certain times ECG may be normal even if the patient has angina.
Can ECG show stable angina?
Yes, ECG can show stable angina. ECG helps in identifying the type of angina and to detects other underlying conditions. The findings depend on the duration of ischemia, the extent of blockage, and the presence of other underlying conditions.
What is a stress test used in diagnosing angina?
Stress tests help to know how well the heart is working when it is pumping hard. This test is performed during exercise on a treadmill or stationary bicycle. These tests also take images of the heart at rest and when it's working hard thereby providing detail about how well the heart is working.
What is the difference between stable and unstable angina?
In stable angina, pain occurs during exercise or during emotional stress. It lasts for a few minutes and usually gets relieved with rest and medications.
In unstable angina, the pain can occur suddenly and lasts longer than stable angina. The pain is severe and requires immediate medical attention.
How is microvascular angina diagnosed?
Diagnosis of microvascular angina involves a medical history, physical examination, and certain diagnostic tests. These tests include stress tests, coronary angiography, and magnetic resonance imaging (MRI).
Diagnosis of angina involves a combination of physical exam, assessment of symptoms, and a group of diagnostic tests. Initial testing includes a 12-lead electrocardiogram (ECG), chest X-ray, and basic laboratory testing, including complete blood count (CBC), and basic metabolic profile (BMP), along with troponin levels.
What are the surgical treatment options available for angina?
Surgical procedures are recommended in situations where angina cannot be managed through lifestyle modifications and medications. Coronary artery bypass graft (CABG) and coronary angioplasty are the two main surgical procedures used in the treatment of angina.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Popular Articles