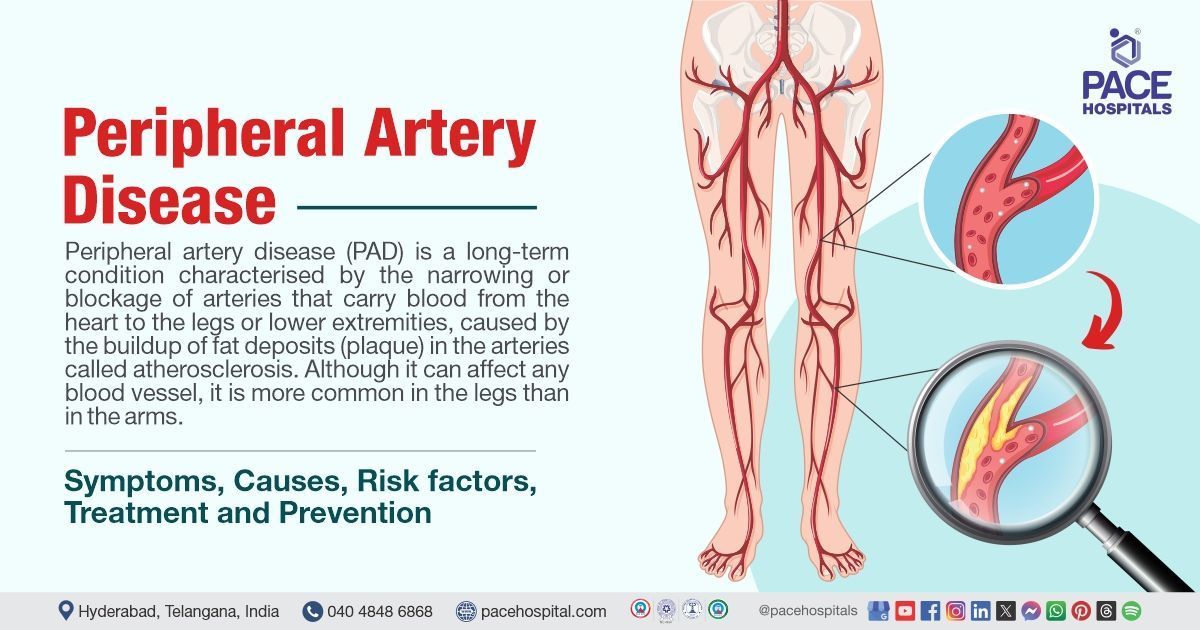
Peripheral Artery Disease – Symptoms, Causes, Diagnosis, Treatment & Prevention
Peripheral artery disease definition
Peripheral artery disease (PAD) is a long-term condition characterized by the narrowing or blockage of arteries that carry blood from the heart to the legs or lower extremities, caused by the buildup of fat deposits (plaque) in the arteries called atherosclerosis. Although it can affect any blood vessel, it is more common in the legs than in the arms.
Peripheral artery disease is also called peripheral vascular disease (PVD), a general term for a variety of circulatory diseases that can affect arteries, veins, and lymphatic vessels. PAD specifically affects the arteries in the legs, while PVD can affect any blood vessel outside of the heart and brain. Individuals with peripheral vascular disease are six times more likely to have a heart attack or stroke.
PAD is diagnosed and treated by a team of healthcare professionals including primary care physicians to educate patients,
cardiologists are involved because many people with PAD are at high risk of heart-related issues. Vascular surgeons and endovascular specialists provide treatment options for severe cases.
Peripheral artery disease meaning
Peripheral
The word "periphery" comes from Greek and Latin words that mean "around" or "to carry around." Originally, it referred to the outer boundary or surface of something,
Artery
The word "artery" comes from the Greek word "arteria," which originally meant "windpipe." Ancient people thought arteries carried air, not blood since they didn't have blood in them after death. Over time, the meaning of "artery" shifted to the blood vessels that carry oxygenated blood from the heart to the rest of the body.
Disease
The word "disease" comes from the Old French word "disease, " meaning discomfort, trouble, or distress.
It's made up of two parts:
- "des-" (meaning "without" or "away")
- "aise" (meaning "ease" or comfort).
So, it means "without ease" or "discomfort.
Prevalence of peripheral arterial disease
Peripheral arterial disease prevalence in the world
Peripheral arterial disease (PAD) affects around 20 crore people worldwide, with symptoms ranging from none to severe, and its prevalence increases with age, affecting more than 20% of those over the age of 80. However, this condition is rare among young people.
Peripheral arterial disease prevalence in India
The prevalence of PAD in India is likely misleading due to underdiagnosis. However, multiple studies suggest rates between 7.6% and 36%, making it a major public health concern.
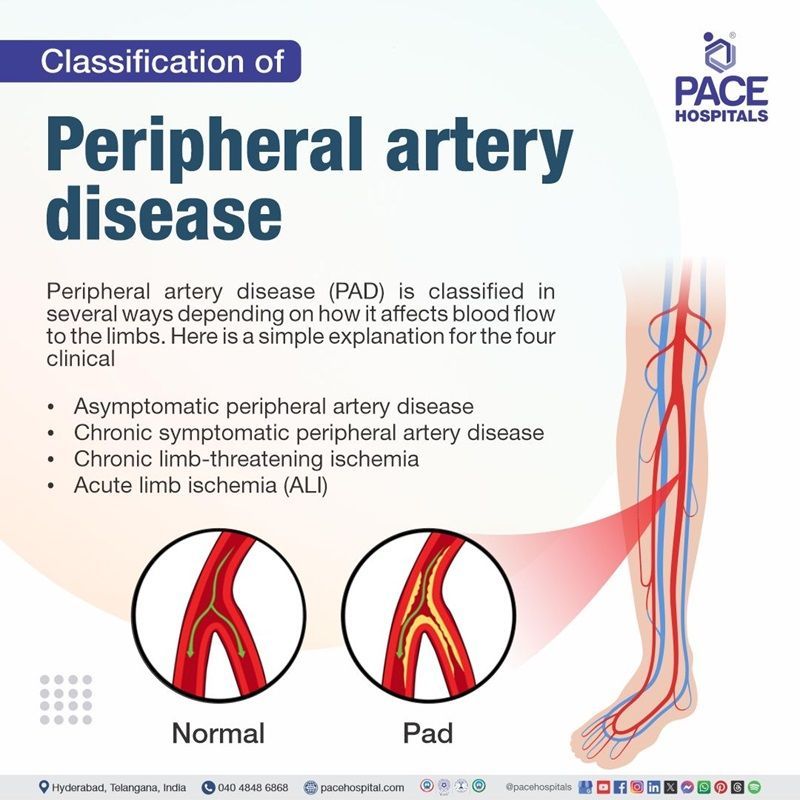
Peripheral artery disease classification
Peripheral artery disease (PAD) is classified in several ways depending on how it affects blood flow to the limbs. The symptoms may change over time due to disease progression or therapy. Here is a simple explanation for the four clinical categories:
- Asymptomatic peripheral artery disease
- Chronic symptomatic peripheral artery disease
- Chronic limb-threatening ischemia
- Acute limb ischemia (ALI)
Asymptomatic peripheral artery disease: It refers to patients who have objectively proven PAD but do not report leg pain or other symptoms. However, they may have functional impairments such as slower walking speeds or difficulty with tasks. Even though they do not experience symptoms, asymptomatic PAD is linked to a higher risk of major adverse cardiovascular events (MACE), including mortality
Chronic symptomatic peripheral artery disease: It is the most common type of the condition that reduces blood flow due to blocked arteries causing pain, cramping, or fatigue in the legs during walking, exercise or any physical activity. These symptoms worsen with effort and typically ease within 10 minutes of rest.
Chronic limb-threatening ischemia (CLTI): It is the most severe manifestation of Peripheral Artery Disease (PAD), characterized by persistent foot pain at rest, non-healing ulcers, or gangrene resulting from critically reduced blood flow to the limbs.
Acute limb ischemia (ALI): A sudden reduction in blood flow due to a clot blocking an artery result in the onset of pain, pallor, pulselessness, paralysis, paresthesia, and coldness in the affected area. This condition requires immediate medical attention.
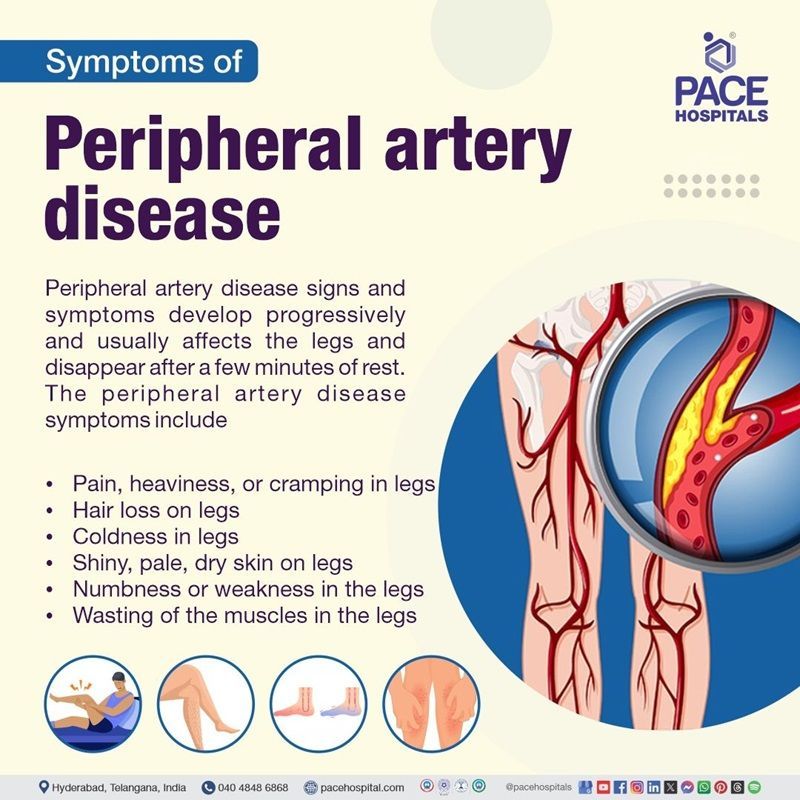
Peripheral artery disease symptoms
Peripheral artery disease signs and symptoms develop progressively. They usually affect the legs, causing discomfort during walking or exercise. They disappear after a few minutes of rest and are called peripheral artery disease claudication (intermittent claudication). The peripheral artery disease symptoms include:
Peripheral artery disease symptoms in legs
Peripheral artery disease symptoms in arms are rare compared to symptoms in legs. The following are the peripheral artery disease symptoms that are commonly seen in the legs:
- Pain, heaviness, or cramping in the legs
- Hair loss on the legs
- Coldness in the legs
- Shiny, pale, dry skin on the legs
- Numbness or weakness in the legs
- Wasting of the muscles in the legs
- Wounds and ulcers (open sores) on the legs, which don’t heal
Peripheral artery disease feet symptoms
Here are some common symptoms observed in the feet of PAD patients:
- One foot may feel colder than the other
- Foot may become pale, discoloured or blue
- Pain or a feeling of pins and needles in the foot
- Sores or wounds on feet which may heal slowly or may not heal at all.
Other peripheral artery disease (PAD) symptoms
In addition to the symptoms mentioned above, patients with peripheral artery disease (PAD) may experience other symptoms, including:
- Thigh or buttock muscles can sometimes be affected, ranging from mild to severe.
- Severe blockages can cause leg pain at rest, often burning and worse at night
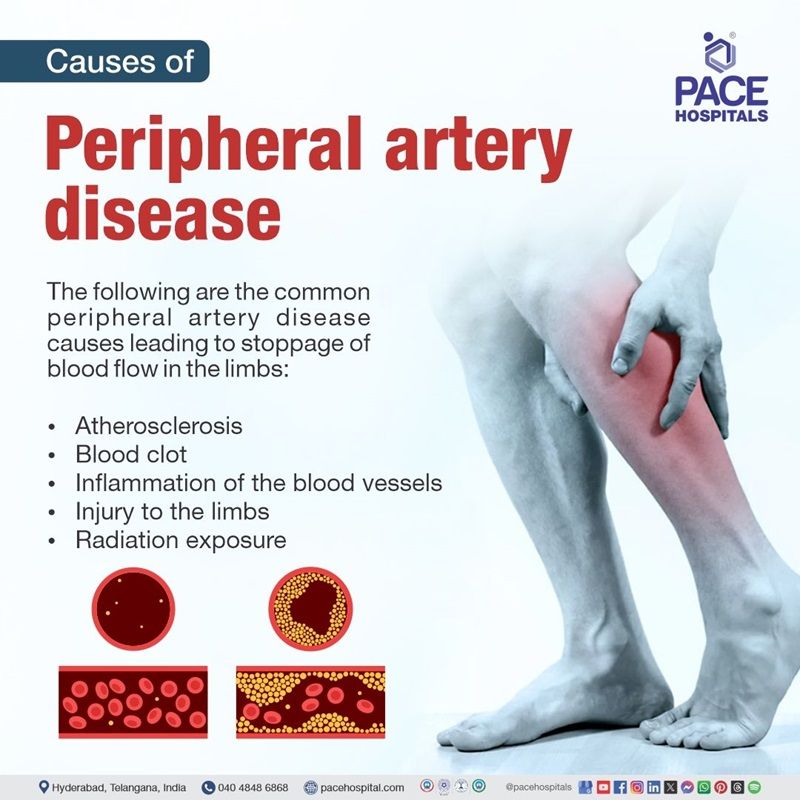
Peripheral artery disease causes
The following are the common peripheral artery disease causes leading to the stoppage of blood flow in the limbs:
- Atherosclerosis: It is the main etiology (cause) of peripheral artery disease, a progressive build-up of fatty substances in the inner walls of arteries, forming plaque that causes the arteries to narrow and reduce blood flow to the legs and lower extremities.
- Blood clot: Sometimes, a blood clot can suddenly block an artery, completely stopping the blood flow and leading to PAD by restricting oxygen and nutrients to the limbs.
Other causes of peripheral artery disease include:
- Inflammation of the blood vessels: This causes the arteries to tighten and harden, which reduces the blood flow to the limbs.
- Injury to the limbs: Injury to the limbs may damage the arteries, leading to constriction or blockage of an artery, which decreases or stops blood flow to the legs.
- Radiation exposure: This is a rare cause of PAD because a small number of people develop PAD due to radiation. When a person receives high radiation, the arteries located in that area become narrow and restrict blood flow (arteriopathy), causing radiation-induced peripheral artery disease (RIPAD).
Peripheral artery disease risk factors
Risk factors of peripheral artery disease include modifiable and non-modifiable factors that damage the blood vessels and promote plaque buildup, which are listed below:
Non-modifiable risk factors for peripheral artery disease
These are certain characteristics or conditions that increase the risk of developing PAD but cannot be changed or controlled which are
- Age: The risk of peripheral artery disease increases with age because arteries naturally become stiffer and less flexible as part of the aging process, reducing blood flow, especially to the limbs. However, PAD can develop at any age, but it is more common in older adults.
- Family history and genetics: Having a family history of PAD, heart disease, stroke, or vascular conditions like vasculitis (inflammation of the blood vessels) can raise the risk of developing PAD. Specific genetic factors (genetic conditions) such as blood clotting disorders like Factor V Leiden, may also contribute to the development and progression of PAD.
- Sex: Men and women have the same chance of getting PAD; however, women are more likely to have asymptomatic disease and experience more severe symptoms, such as difficulty in walking and restricted movement.
Modifiable risk factors for peripheral artery disease
Modifiable risk factors are lifestyle behaviours or health conditions that can be changed or controlled to reduce the risk of developing PAD:
- Smoking and second-hand smoke: Smoking or frequently inhaling second-hand smoke harms blood vessels, elevates blood pressure, and causes high cholesterol levels. Nicotine in tobacco also tightens blood arteries, reducing blood flow to the legs. Hence, many healthcare professionals recommend the stoppage of smoking to lower the risk of many circulatory diseases.
- Physical inactivity: A lack of physical exercise may worsen risk factors of PAD, such as high cholesterol, high blood pressure, and poor circulation.
- Stress: Being stressed for a long time increases levels of stress hormones that affect blood flow and pressure, causing damage to the blood vessel lining and promoting blood clot formation.
Medical conditions of PAD
The following are some of the medical conditions that can increase the risk of PAD if the patient suffers for an extended time from those conditions:
- Chronic kidney disease: In CKD patients, the buildup of waste products leads to systemic inflammation, which decreases albumin levels (hypoalbuminemia) and increases the risk of developing PAD, where blood vessels become narrowed and reduce blood flow.
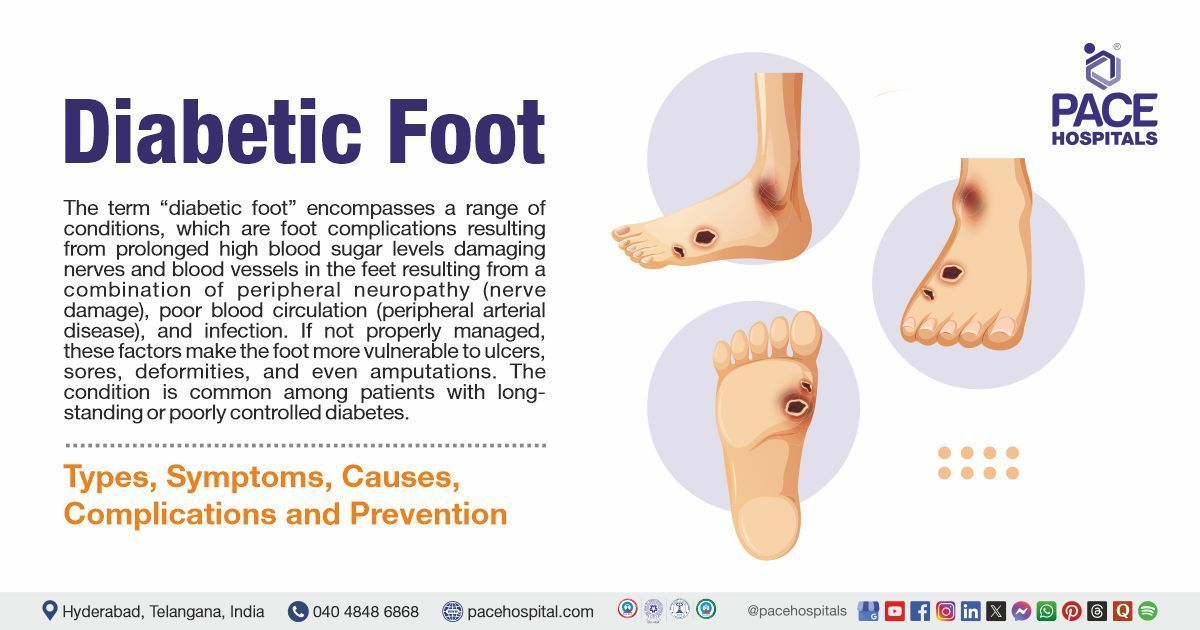
- Diabetes: It is a common condition characterised by high blood sugar levels, associated with the increased risk of atherosclerosis, which contributes to the development and worsening of peripheral artery disease (PAD)
- Blood clot disorders: Below mentioned are the certain disorders that cause blood clots, increasing the risk of developing peripheral artery disease (PAD):
- Thrombocytosis (high platelet count): A high number of platelets can lead to excessive clotting, increasing the risk of blockages in blood vessels, which can reduce blood flow to the limbs and contribute to PAD
- Antiphospholipid (autoimmune disorder that causes blood clot) syndrome: The body produces antibodies that cause blood to clot, forming blood clots that can block blood vessels and raise the risk of developing peripheral artery disease (PAD).
- Fibromuscular dysplasia: FMD increases the risk of peripheral arterial disease (PAD) by abnormally thickening artery walls, leading to narrowing and reduced blood flow, especially in the legs, which is a key characteristic of PAD.
- High blood pressure (Hypertension): It is a risk factor for peripheral artery disease (PAD) because it promotes plaque buildup in the arteries, narrowing them and reducing blood flow to the extremities.
- Obesity or overweight: Being overweight can significantly increase the chance of developing PAD; this is because excess body fat contributes to inflammation in the arteries, which can lead to plaque buildup and narrowed blood vessels in the legs.
- High cholesterol levels: High cholesterol, particularly elevated LDL levels, causes plaque buildup in the arteries, resulting in narrowing them and restricting blood flow, which increases the risk of peripheral arterial disease (PAD).
Peripheral artery disease complications
Peripheral artery disease (PVD) can lead to severe complications because of reduced blood flow, as blood flow is essential for delivering oxygen, affecting various organs and tissues in the lower extremities. The peripheral artery disease complications include:
- Gangrene: It is a serious complication of peripheral artery disease that causes finger and toe gangrene (death of body tissue) due to bacterial infection caused by insufficient blood flow.
- Nonhealing ulcer: Peripheral artery disease (PAD) restricts oxygen-rich blood flow to the affected tissue leading to tissue damage causing painful and poor wound healing, this often results to chronic sores that can't heal on their own, particularly on the legs and feet.
- Amputation: PAD restricts blood flow to the extremities and can cause tissue damage and gangrene, requiring surgical removal of the affected limb (peripheral artery disease (PAD) amputation) to avoid further complications.
- Erectile dysfunction: PAD can cause erectile dysfunction by lowering blood flow to the penis as a result of atherosclerosis, which occurs when plaque formation narrows and hardens the arteries in the penis, making it difficult to maintain an erection.
- Heart attack: Atherosclerosis, Atherosclerosis, which is the primary cause of peripheral artery disease (PAD), can also affect other arteries, including the coronary arteries, increasing the risk of heart attacks and other heart problems.
- Stroke: It is a complication of peripheral artery disease (PAD) because people with PAD have a major risk of experiencing a
stroke due to the shared underlying cause of plaque buildup in arteries (atherosclerosis), which can also affect blood vessels in the brain, mainly the carotid arteries, leading to a stroke.
Peripheral artery disease diagnosis
Peripheral artery disease diagnosis involves a thorough evaluation including patient’s medical history, physical examination, and key diagnostic tests. Following the below mentioned steps helps in identifying the presence and severity of PVD for the better treatment.
- Medical history
- Family history
- Physical examination
- Calculating ABPI (Ankle-Brachial Pressure Index) test score
- Other peripheral artery disease diagnostic tests include
- Exercise ankle-brachial index test for peripheral artery disease
- Blood test:
- Cholesterol levels.
- Blood sugar levels (to screen for diabetes)
- C-reactive protein (CRP) for inflammation
- Doppler Ultrasound
- 6-minute walking test
- Segmental Doppler pressure testing
- CT angiography of peripheral arterial disease
- Magnetic resonance angiography (MRA)
- Catheter-based angiography
Peripheral artery disease treatment
There is no cure for peripheral artery disease, but making lifestyle changes and taking medications are some of the peripheral artery disease treatment options that help to manage the symptoms, which include:
Peripheral artery disease lifestyle changes
Some of the lifestyle changes for peripheral arterial disease include
- Exercising regularly
- Quitting smoking
- Eating a balanced diet
- Managing weight
- Cutting down on alcohol
- Mental wellbeing
- Managing diabetes
Peripheral artery disease exercise programs
Some of the best exercises for peripheral artery disease include:
- Supervised exercise
- Home exercise programs
Peripheral artery disease drugs
Here are common classes of medication prescribed by healthcare professional based on PAD patient’s condition:
- Statins
- Antihypertensives
- Antiplatelet
- Blood-thinning medicines or anti-coagulants
- Vasodilator or peripheral artery disease vasodilator
Peripheral artery disease surgery
There are two main types of surgical revascularization peripheral arterial disease treatment options, such as:
- Angioplasty
- Artery bypass graft
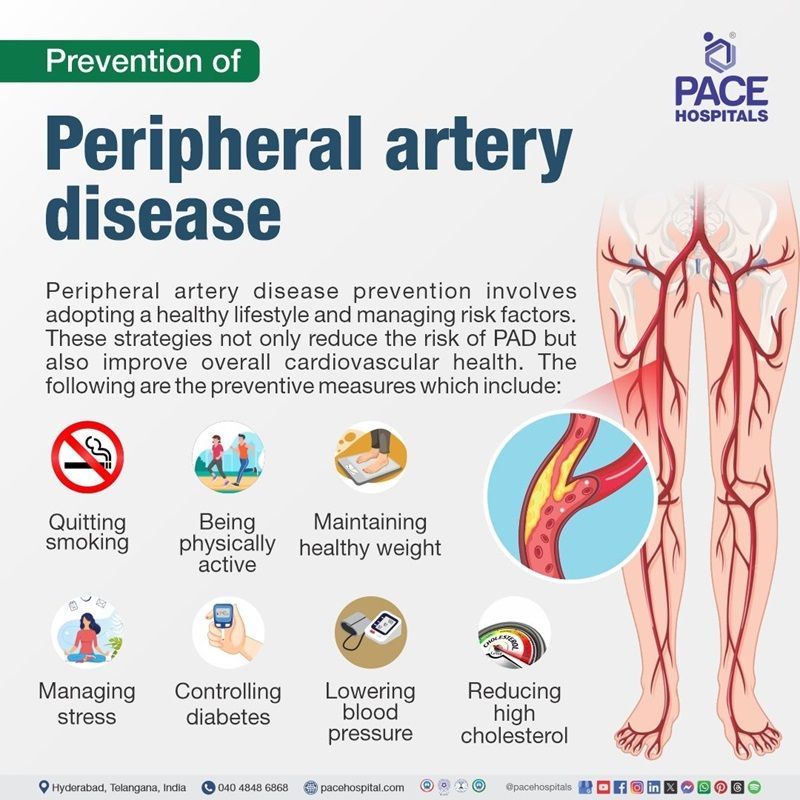
Peripheral artery disease prevention
Peripheral artery disease prevention involves adopting a healthy lifestyle and managing risk factors. These strategies not only reduce the risk of PAD but also improve overall cardiovascular health. The following are the preventive measures that include:
- Quitting smoking: It is the most effective method to reduce the possibility of PAD because it protects blood vessels and prevents plaque accumulation.
- Adopting a healthy eating pattern: Adopting a healthy eating pattern, like the DASH (Dietary Approaches to Stop Hypertension) or vegetarian diet, helps in the prevention of peripheral artery disease (PAD) by supporting vascular health through nutrient-rich foods, lean proteins, healthy fats, and reducing intake of harmful fats, sodium, and added sugars.
- Being physically active: Regular physical activity, such as moderate-intensity aerobic exercise for 150 minutes per week or exercise therapy for individuals suffering from claudication (leg discomfort while walking), can improve circulation and prevent peripheral artery disease (PAD).
- Maintaining healthy weight: A normal body weight puts less strain on the cardiovascular system, and losing excess weight helps in managing cholesterol levels, blood sugar levels, and blood pressure, which lowers the risk of peripheral artery disease (PAD).
- Managing stress: Practising stress-reducing activities such as yoga or deep breathing, as well as avoiding excessive alcohol and unhealthy habits, can support cardiovascular health and reduce the risk of peripheral artery disease (PAD).
Managing risk factors such as
- Controlling diabetes: Diabetes must be controlled by keeping blood sugar levels within normal ranges by diet, medication, and regular monitoring to prevent peripheral artery disease.
- Lowering blood pressure: Lowering high blood pressure to the normal range of 120/80 mmHg by following healthcare professional recommendations, taking prescribed medications, and monitoring regularly can reduce the risk of peripheral artery disease (PAD).
- Reducing high cholesterol: Maintaining healthy LDL levels with a balanced diet and, if necessary, taking statins can help in preventing peripheral artery disease (PVD).
Difference between peripheral artery disease and peripheral vascular disease
Peripheral artery disease vs Peripheral vascular disease
Peripheral artery disease significantly affects the arteries in the legs, whereas peripheral vascular disease affects any blood vessel located outside of the brain and heart. Peripheral artery disease is a type of peripheral vascular disease PVD. Some of the key differences are listed below:
| Elements | Peripheral artery disease | Peripheral vascular disease |
|---|---|---|
| Affected blood vessels | Peripheral artery disease affects arteries. | Peripheral vascular disease affects both arteries and veins. |
| Common causes | Causes of peripheral artery disease is atherosclerosis (deposition of fat substances called plaque), inflammation of blood vessels, injury and radiation exposure. | Peripheral vascular disease is caused by atherosclerosis, blood clots and infections. |
| Common symptoms | Pain, numbness, cramping, and tingling in the legs and feet, nonhealing ulcers, changes in the colour of skin and changes in the temperature of affected limbs. | Pain, heaviness and swelling in the legs, change in the colour of skin on legs or feet, varicose veins and leg ulcers. |
Frequently Asked Questions (FAQs) on Peripheral artery disease (PAD)
What causes peripheral artery disease?
The cause (etiology) of peripheral artery disease (PVD) is atherosclerosis, which occurs when the fatty deposits develop in the arteries and block blood flow. However, it can also be caused by blood clots, inflammation, injuries, and radiation exposure.
What is the best treatment for peripheral artery disease?
The best treatment for peripheral artery disease involves lifestyle adjustments such as quitting smoking, eating healthy food, and participating in regular physical activity to improve blood circulation and vascular function. To reduce symptoms and prevent complications, patients should also take medications recommended by healthcare professionals, such as antiplatelet drugs and statins.
How is peripheral vascular disease diagnosed?
Peripheral vascular disease (PVD) is diagnosed by evaluating the patient's medical and family history and conducting specific tests, including the ankle-brachial index (ABI), Doppler ultrasound, angiography, MRI, and CT scan.
What is peripheral artery disease?
Peripheral artery disease (PVD) is a long-term condition resulting from the narrowing or blocking of arteries that carry blood from the heart to the legs or lower extremities. The primary cause of PAD is atherosclerosis, the buildup of fat deposits (plaque) in the arteries.
How to treat peripheral artery disease?
Peripheral artery disease (PAD) is primarily treated through lifestyle modifications such as eating a balanced diet, regular exercise and stopping smoking, medications like antiplatelet agents and statins to prevent blood clots, and, in many cases, surgical interventions to restore proper blood flow.
Why beta blockers are contraindicated in peripheral vascular disease?
Beta-blockers are generally avoided in peripheral vascular disease (PVD) because they have been reported to worsen symptoms of intermittent claudication (pain, fatigue, or cramping in the legs that occurs during physical activity) by reducing blood flow to the limbs.
How to cure peripheral artery disease?
Peripheral artery disease (PAD) cannot be cured, but treatments like lifestyle changes, medications, exercise, and sometimes surgery can help manage symptoms and slow disease progression.
Is peripheral vascular disease the same as peripheral arterial disease?
Peripheral Artery Disease (PAD) is sometimes referred to as Peripheral Vascular Disease (PVD) because both describe conditions that affect the blood vessels outside the brain and heart, primarily in the limbs. Peripheral vascular disease also deals with veins and lymphatic vessels.
Peripheral vascular occlusive disease is the blockage or narrowing of blood vessels, typically in the legs but rarely in the arms. It is often caused by atherosclerosis and leads to reduced blood flow.
Can peripheral artery disease cause peripheral neuropathy?
Yes, peripheral artery disease (PAD) can lead to peripheral neuropathy by reducing blood flow to the legs and feet, resulting in nerve and tissue damage. The risk of nerve damage is especially high in individuals with diabetes.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations – Find the Best Hospital Near You
Metro Pillar Number C1772, Beside Avasa Hotel, Hitech City Road, Near HITEC City Metro Station, Hyderabad, Telangana, India.
Mythri Nagar, Beside South India Shopping Mall, Hafeezpet, Madeenaguda, Hyderabad, Telangana, India.
040 4848 6868
Payment in advance for treatment at PACE Hospitals, Hyderabad, Telangana, India (Pay in INR ₹)
For Bank Transfer:-
- Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545 - Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc).

CONTACT US
Call: +914048486868
WhatsApp: +918977889778
Email: info@pacehospitals.in
FOLLOW US
SUBSCRIBE
Subscribe to our newsletter and stay updated with the latest health information.
Subscribe to PACE Hospitals' Public Newsletter
Thank you for subscribing to PACE Hospitals' Newsletter. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
ABOUT US
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals – your trusted hospital near me.