Cardiac Arrest: Symptoms, Causes, Types, Complications, Treatment & Prevention
Cardiac arrest definition
As defined by the American College of Cardiology and the American Heart Association, "sudden cardiac arrest is the sudden cessation of heart activity, where the patient (or victim) becomes unresponsive, with no signs of circulation and no normal breathing. If the victim doesn't get timely treatment, this condition progresses to sudden death.”
The cause of cardiac arrest varies by age and population, most commonly occurring in those with a history of cardiac disease. In most of the cases, cardiac arrests are sudden and usually unexpected, which is fatal. However, cardiopulmonary resuscitation (CPR) by bystanders and advances within emergency medical services may help save the life of the victim.
Cardiac arrest meaning
"Cardiac" is derived from the French word "cardiaque" or directly from the Latin word "cardiacus, from the Greek “kardiakos”, which means "heart" or "pertaining to the heart," while the arrest word came from Anglo-French "arrest" or Old French "areste," which means "stoppage, delay" or "state of being stopped, the act of stopping." Both words refer to the stoppage of the heart.
Prevalence of Cardiac Arrest
Globally, around 11 crore men and 8 crore women are suffering from coronary artery disease (CAD), which is a leading cause of death, taking an estimated 17.9 crore lives each year.
Sudden cardiac arrest (SCA) is a global public health issue with a mortality rate of more than 90%. The occurrence of death due to cardiac arrest is higher in males compared to women at a younger age.
The global occurrence of out-of-hospital cardiac arrest (OHCA) is estimated to be 55 cases per 100,000 person-years, making it a significant public health challenge.
According to a study, SCD accounted for 10.3% of the total deaths in the population residing in Southern India.
SCD in CAD patients is more prone to death in the western hemisphere when compared to the Indian subcontinent by at least 5-8 years.
"The incidence of SCA during sports is 0.7 to 3 cases per 100,000 sports players in all age groups". These events predominantly affect men, with 90% occurring during recreational sports.
Ischemic (occlusive) coronary disease is the leading cause of cardiac arrest and sudden cardiac death. Due to sudden infant death syndrome, the Initial peak of sudden death may occur from birth to 6 months of age. Incidence (occurrence) is usually low until reaching a second peak between ages 45 and 75. Interestingly, the common cause of cardiac death observed in adolescents and young adults mirrors that of middle-aged and older adults.
Types of Cardiac Arrest
Cardiac arrest is primarily classified based on the underlying rhythm detected on an electrocardiogram (ECG), with the main categories being:
- Ventricular fibrillation (VF): The most common rhythm associated with cardiac arrest, characterized by chaotic electrical activity in the ventricles, causing ineffective pumping action.
- Pulseless ventricular tachycardia (VT): Rapid, abnormal heart rhythm originating in the ventricles, which doesn't effectively pump blood.
- Pulseless electrical activity (PEA): Electrical activity is present on the ECG, but no palpable pulse, indicating a problem with mechanical contraction.
- Asystole: Complete absence of electrical activity on the ECG, signifying a flatline.
Cardiac Arrest Symptoms
In most cases, cardiac arrest occurs without any warning signs. However, some individuals may experience some warning signs before a cardiac arrest. These can include:
- Palpitations
- Fainting
- Chest pain
- Breathlessness
- Dizziness
However, sudden cardiac arrest (the unexpected stoppage of circulation without any warning) in children and adolescents is most commonly due to an underlying structural cardiac abnormality or arrhythmia resulting from a channelopathy. In sudden cardiac arrest, the patient may experience the following signs and symptoms:
- Rapid, shallow breathing
- Arterial hypotension
- Progressive decrease in mental alertness
- Collapse without warning
- Myoclonic jerks or seizure-like activity (rarely)
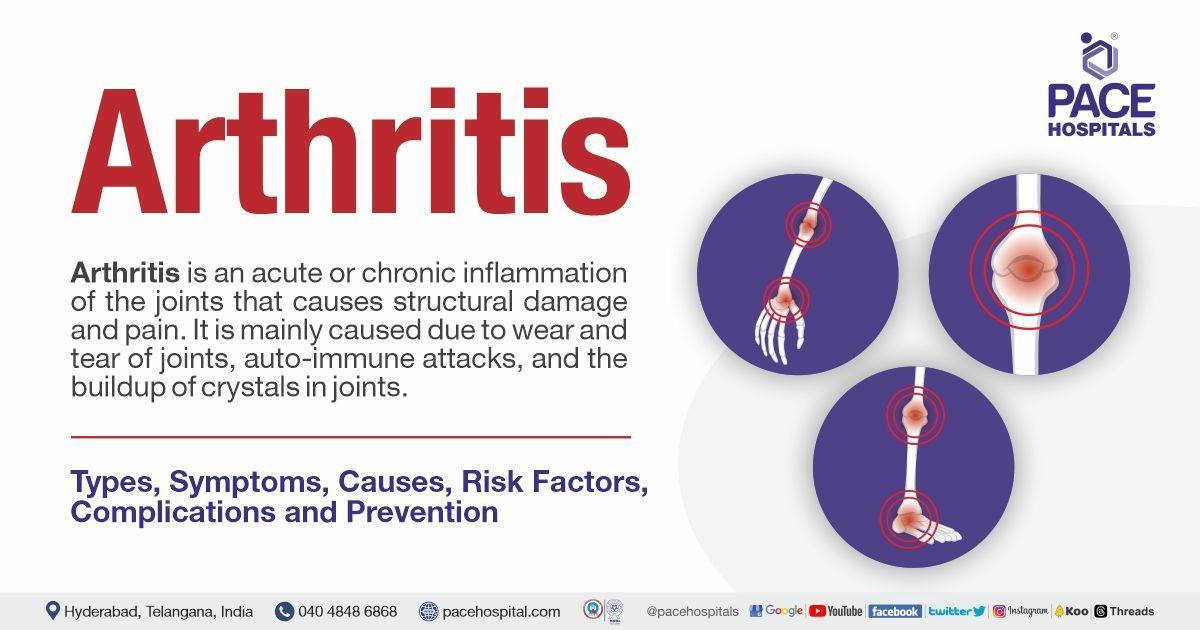
Cardiac Arrest Causes
Cardiac arrest can occur due to various heart conditions that are known. The majority of cases arise when there is a malfunction of the diseased heart's electrical system. The following are the reasons for sudden cardiac arrest:
Ischemic coronary disease: Cardiac arrest may occur due to underlying structural heart disease. 70% of cardiac arrest cases are thought to be due to ischemic coronary disease, which is the major cause of cardiac arrest, but in 15% of patients, the cause is pulmonary. Other structural causes of cardiac arrest include:
- Congestive heart failure: It is a situation where the heart doesn't pump blood as efficiently as it can. Patients with CHF have a high occurrence of sudden cardiac death (SCD), which is caused by ventricular arrhythmias. The mortality rate is high (40% per year) in patients with condition of class III and IV heart failure, and half of the deaths are sudden.
- Left ventricular hypertrophy: Significant left ventricular hypertrophy (LVH) (thickening of the wall of the heart's main pumping chamber) causes sudden cardiac arrest and raises the risk of SCD 6- to 8-fold in men and 3-fold in females.
- Congenital coronary artery abnormalities: Congenital coronary artery anomalies represent an uncommon cause of cardiac arrest in children and adults. Importantly, in the absence of additional heart abnormalities, these are a cause of sudden death in young athletes.
- Arrhythmogenic right ventricular dysplasia: It is a rare disorder that may cause a type of arrhythmia called ventricular tachycardia and SCD in young, apparently healthy individuals.
- Hypertrophic obstructive cardiomyopathy: It is a common genetic cardiovascular disease (CVD) that affects the left ventricle and can occur at any age, causing sudden cardiac death (SCD) mainly due to ventricular tachyarrhythmia or ventricular tachycardia.
- Cardiac tamponade: It is a traumatic or medical emergency that occurs when fluid enough fluid accumulates in the pericardial sac, compressing the heart and decreasing cardiac output and leading to shock.
Non-structural causes include:
- Brugada syndrome: Brugada syndrome is a dangerous genetic disorder that causes an irregular heartbeat, especially during sleep or at rest, which accounts for sudden death or cardiac arrest.
- Wolf-Parkinson-white syndrome: Wolff-Parkinson-White syndrome is characterized by abnormal electrical pathways in the heart that disrupt the heart's normal rhythm (arrhythmia), which rarely leads to cardiac arrest and sudden death.
- Congenital long QT syndrome: LQTS is a genetic heart condition causing prolonged QT interval on ECG and a high risk of life-threatening arrhythmias, which is one of the important risk factors for cardiac arrest.
Other non-cardiac causes
- Pulmonary embolism: Pulmonary embolism is characterized by blocking a pulmonary artery of the lung by the embolus (usually a blood clot). Sometimes, large emboli cause so much blockage that the right side of the heart cannot pump adequate blood through the pulmonary arteries, oxygen-rich blood to the brain, and other vital organs, leading to decreased blood pressure. If too little blood is pumped by the heart, resulting in excessive strain, the person can go into cardiac arrest, shock and die.
- Pneumothorax
- Primary respiratory arrest
- Toxic ingestions
- Intracranial haemorrhage, including drug overdose, severe infection (sepsis), electrolyte abnormalities, hypothermia, or trauma.
Risk factors for Cardiac Arrest
Several lifestyle and hereditary factors may raise the risk of cardiac arrest. They include the following:
- Heart disease: Having a history of heart problems is a major risk factor for cardiac arrest.
- Coronary heart disease: Cardiac artery disease is the primary risk factor for cardiac arrest in adults, which is caused by cholesterol.
- Arrhythmias: Atrial fibrillation and long QT syndrome are the common types of arrhythmias that increase the risk of cardiac arrest.
- Problems with the heart structure: A congenital heart defect (present at birth) may damage the heart. Other structural issues, including cardiomyopathy and heart valve disease, also increase the risk of developing cardiac arrest.
- Heart failure: It is a condition that occurs when the heart doesn't pump adequate blood for the needs of the body. Cardiac arrest is one of the complications of heart failure.
- Damage to the heart: Heart inflammation is caused by a medical condition or infection.
- Family history of heart disease or cardiac arrest: Some conditions that increase the cardiac arrest risk run in families. Suppose the patient's blood relatives have conditions such as arrhythmias or cardiac conduction disorders, or had a cardiac arrest. In case of any early, unexpected, or unexplained deaths of blood relatives or SIDS, it is better to inform healthcare professionals.
- Conditions such as dangerous arrhythmias are linked with specific genes. These rare conditions cause problems with the heart's electrical system. If the person has a cardiac arrest, the risk for another one is very high. One in 5 survivors may have another life-threatening arrhythmia within the following year.
Sometimes, behavior or activity triggers a cardiac arrest. Triggering events are common in people who have a history of heart conditions or other risk factors.
- Physical exertion or physical stress, including competitive sports: One out of three cardiac arrest events occurs in athletes during their sleep or resting after activity. In general, the risk of (SCD) doubles during physical activity. In athletes, it is 2—to 3-fold higher than in non-athletes. Some types of cardiomyopathy and occasionally conduction disorders, including long QT syndrome, also cause cardiac arrest during sleep or exercise. However, moderate physical activity is recommended, which is helpful to lower the risk of cardiac arrest.
- Age: The risk of cardiac arrest rises with age. However, it is rare in people younger than 30. In younger people, the primary risk factors are genetic arrhythmias, structural problems with heart or coronary arteries, heart inflammation, and substance use.
- Sex: Men will more likely have a high risk of cardiac arrest. After menopause, the risk of cardiac arrest will increase in women.
- Alcohol or drug abuse: The use of toxic substances is one of the important risk factors for sudden cardiac death. The most relevant toxic substances are the illegal drugs. Additionally, several therapeutic drugs can increase the risk of sudden cardiac death. Too much alcohol raises the weight and blood pressure of a person, increasing the risk of stroke, heart attack, and type 2 diabetes.
- Low potassium or magnesium: Magnesium is also known for its role in heart muscle cells' electrical stability and energy balance (cardiomyocytes). Hypomagnesemia has been linked with atrial and ventricular arrhythmias and low serum magnesium, which could be accountable as a risk factor for sudden cardiac death (SCD). Hypokalaemia is linked with a raised risk of arrhythmia in patients with cardiovascular disease. Since the heart muscle needs potassium in order to contract, not having enough potassium may cause the heart to stop contracting, which is cardiac arrest.
- Obesity: Obesity contributes directly to incident cardiovascular risk factors, including dyslipidemia, type 2 diabetes, and high blood pressure (Hypertension). In obese persons, there will be an increase in total blood volume and cardiac output, causing greater cardiac workload.
- Smoking: Chemicals in cigarette smoking thicken the blood and form clots inside veins and arteries, resulting in a raised risk of heart disease, which is a major cause of cardiac arrest.
Other medical conditions and events
Some medical conditions, medicines, and injuries are also accountable for increasing the risk of cardiac arrest.
- Respiratory arrest: In the case of a person who stops breathing, cardiac arrest will occur unless they get immediate treatment. Choking, trauma, drug overdose, and poisoning can cause respiratory arrest. Some conditions, including pneumonia and seizure disorders, also lead to respiratory arrest.
- Diabetes and changes in the levels of electrolytes, including potassium, magnesium, and calcium in the blood increase the risk of cardiac arrest.
- High blood pressure: High blood pressure strains the heart muscle, leading to cardiovascular disease (CVD), increasing the risk of stroke and heart attack.
- Certain medicines: Some diuretics, antibiotics, and heart medicines can worsen arrhythmias. It is important to inform healthcare professionals about all prescription and over-the-counter medications.
- A hard blow to the chest: Getting struck on the left side of the chest directly over the heart may lead to cardiac arrest. Most often, these injuries are from a softball, baseball, hockey puck, soccer, football, or lacrosse ball. Children are at the highest risk for this type of injury.
- Some people may experience cardiac arrest without any risk factors at all.
- Severe emotional stress: Mental stress appears to give rise to sudden cardiac arrest (SCA), presumably by more directly impacting the cardiac ion channels that control the heart's electrical properties, leading to ventricular fibrillation, the arrhythmia that underlies SCA.
This is paragraph text. Click it or hit the Manage Text button to change the font, color, size, format, and more. To set up site-wide paragraph and title styles, go to Site Theme.
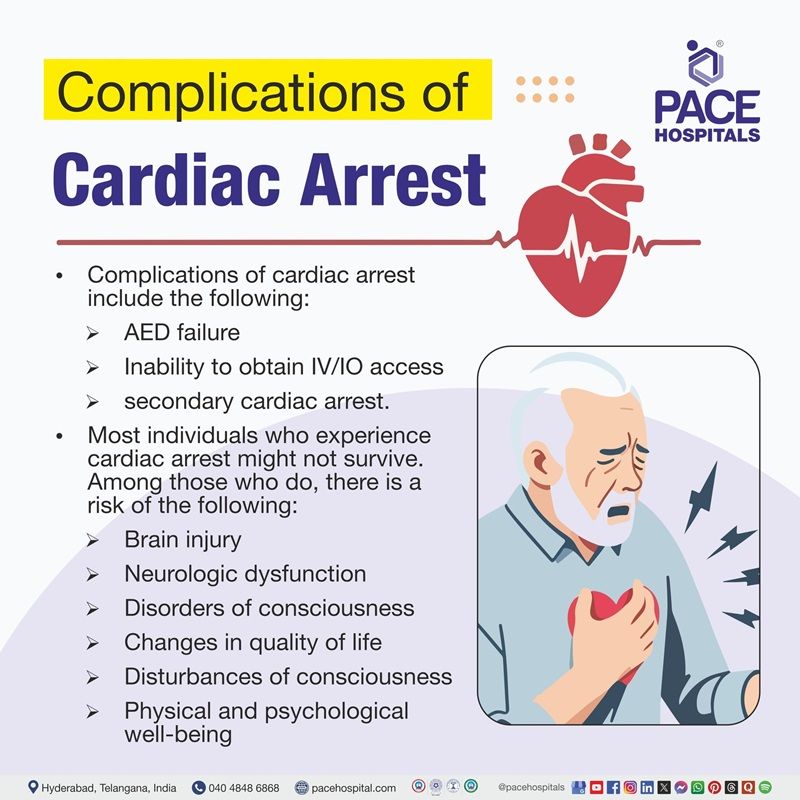
Complications of Cardiac Arrest
Complications of cardiac arrest may include the following:
- AED failure: It is not common, but it is the most detrimental complication for a patient
- Inability to obtain IV/IO access
- After ROSC, failing to secure and maintain a definitive airway device could lead to secondary cardiac arrest.
Cardiac arrest causes ischemia with consequences at the cellular level, affecting organ function even after cardiopulmonary resuscitation and restoration of perfusion. It mainly causes direct cellular damage and oedema formation, which is particularly harmful to the brain, which has a small room to expand. It often results in increased intracranial pressure and corresponding decreased cerebral perfusion post-resuscitation.
Blood flow and oxygen are diminished to the vital organs of the patient, causing potential damage to the brain or organ dysfunction in the case of cardiac arrest. Most individuals who experience cardiac arrest might not survive. Among those who do, there is a risk of the following:
- Brain injury
- Neurologic dysfunction
- Disorders of consciousness
- Changes in quality of life
- Disturbances of consciousness
- Physical and psychological well-being
Cardiac Arrest Diagnosis
The diagnosis of cardiac arrest is made by findings of pulselessness, apnea, and unconsciousness. Pupils dilate and become unreactive to light after several minutes. While treating a cardiac arrest patient, little to no blood or imaging testing is necessary. The following will be helpful in the diagnosis of cardiac arrest.
- Clinical evaluation
- Cardiac monitoring and electrocardiography (ECG)
- Sometimes, testing for the cause (e.g., echocardiography, chest imaging [X-ray, ultrasonography], electrolyte testing.
Medical history: History given by family or rescue people may suggest an overdose
Cardiac monitor: It will be applied to the patient to look for the following conditions
- Ventricular fibrillation (VF),
- Ventricular tachycardia (VT),
- Asystole
Sometimes, a perfusing rhythm (e.g., extreme bradycardia) is present; this type of rhythm may represent pulseless electrical activity (PEA) or extreme hypotension with failure to detect a pulse.
The patient is examined for potentially treatable causes, such as "Hs and Ts."
- Hs: Hypoxia, hypovolemia, acidosis, hyperkalaemia or hypokalaemia, hypothermia
- T: Tablet or toxin ingestion, cardiac tamponade, tension pneumothorax, thrombosis (coronary or pulmonary).
- In paediatric children, hypoglycaemia is another potentially treatable cause.
Cardiac ultrasonography: It is used to detect the following:
- Cardiac contractions
- Cardiac tamponade extreme hypovolemia (empty heart),
- Right ventricular overload suggestive of pulmonary embolism
- Focal wall motion abnormalities suggestive of myocardial infarction (MI)
Bedside blood tests: To detect abnormal levels of potassium to confirm the suspicion that cardiac arrest was caused by an arrhythmia secondary to hyperkalaemia.
Cardiac Arrest Treatment
Treatment of cardiac arrest patients comes in multiple stages. Identification of a victim includes assuring a patient is unresponsive, without normal breathing and central pulses.
Once a victim is identified, prompt CPR and activation of the basic life support measures (emergency response) are the priority.
The interventions that have been proven to reverse cardiac arrest are early CPR and early defibrillation. If defibrillation access is available for the public, it should be activated and utilized if needed.
Advanced life support measures will be used, such as intravenous or intraosseous medication administration.
If the patient's return of spontaneous circulation (ROSC) is obtained, the health care team provides post-resuscitation with subsequent long-term management.
- Basic life support: Basic Life Support is the type of care, including cardiopulmonary resuscitation (CPR) and defibrillation with an automated external defibrillator (AED) by first responders, healthcare professionals, and public safety professionals to anyone who is experiencing cardiac arrest, heart attack, stroke, respiratory distress or an obstructed airway. Cardiac arrests and accidents are the most common types of emergencies with grave effects, but simple actions and skills can improve the outcome, and immediate cardiopulmonary resuscitation can double or triple the chances of survival. However, it requires basic knowledge and skills in CPR, using automated external defibrillators (AED), and relieving airway obstructions in patients of every age. BLS treatment includes the addition of ventilation during active CPR. Current guidelines recommend two breaths for every 30 compressions.
- Cardiopulmonary resuscitation: The first line of treatment for cardiac arrest is usually CPR, during which another person compresses the victim's chest to increase blood flow to the organs. CPR is helpful to treat cardiac arrest temporarily until more advanced emergency treatment is available to the victim experiencing cardiac arrest.
- Defibrillator: A defibrillator is a device that sends an electric charge or shock to the heart to help it restore its beat and function normally. It is needed to save the person's life immediately and reduce further organ damage from the deprivation of oxygen and blood. However, it will be used by trained first responders. In some public places, an automated external defibrillator (AED) is available, similar to the AED. AED helps to detect harmful arrhythmias and deliver an electric shock to the heart. This device is designed for nonmedical persons and can be used by anyone.
- Advanced Life Support: It includes BLS treatment with the addition of medications and advanced airways, such as supraglottic airway devices and endotracheal intubation. Advanced life support (ALS) providers benefit from cardiac rhythm interpretation, allowing for more immediate defibrillation if indicated.
Other treatments, such as certain medications and surgical procedures, may be done on the patient based on the underlying cause.
How to respond to a cardiac arrest situation?
If anyone thinks that the person may be suffering from cardiac arrest, it is recommended to do the following:
- Ensure scene safety
- Check for response
- Check for no breathing or only gasping
- Shout for help
- Call emergency services
If a bystander is trained:
- Begin CPR with compressions: Push down on the chest at least 2 inches in the center. Push at a rate of 100–120 compressions per minute. Then, allow the chest to return to its normal position after each push.
- Use an AED
- Continue CPR
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support

Cardiac Arrest Prevention
A person can reduce the risk of cardiac arrest and other acquired heart diseases by focusing on certain factors, such as:
- Eating heart-healthy meals: As mentioned above, heart problems make a person more vulnerable to cardiac arrest. Eating heart-healthy meals plays a major role in maintaining a healthy heart, resulting in a decreased risk of heart conditions. Heart-healthy eating involves choosing certain foods, including fruits and vegetables, while limiting others, such as added sugars and saturated fats.
- Exercising: Being physically active is most important because it can help to manage the overweight and reduce the risk of stress, clinical depression, and heart disease.
- Quitting smoking and drug use: A individual who smokes throughout their life are at high risk of developing a range of potentially lethal conditions. Quitting smoking increases circulation and lung function within 2–12 weeks, decreases shortness of breath and cough within 1–9 months, and reduces the risk of stroke within 5–15 years.
Stopping drug use can reverse the damage to the heart and improve its function when combined with appropriate treatments.
- Losing weight: Weight loss improves metabolic function and high blood pressure and enhances heart pumping and relaxation, making the heart tissue and blood vessel walls thinner. Cholesterol levels also decrease after losing weight.
- Reducing alcohol intake: Less consumption of alcohol is related to a lower risk of heart conditions such as coronary artery disease (CAD) and ischemic stroke, which is characterized by blockage of blood vessels that supply the brain.
- Reducing stress: Managing stress can help a person sleep better, control weight, have less muscle tension, and reduce the risk of heart conditions.
Differences between Cardiac Arrest and Heart Failure
Cardiac arrest vs heart failure
Both cardiac arrest and heart failure are forms of heart disease. While they look like same conditions, many differences exist between them as well, such as:
| Elements | Cardiac arrest | Heart failure |
|---|---|---|
| What happens during the event | It is characterized by the sudden stoppage of heart function, leading to a cessation of blood circulation. | Heart failure or congestive heart failure is characterised by the inability of the heart to pump efficiently. |
| Causes | It caused by coronary artery disease, Irregular heart rhythms (electrical malfunction), congenital coronary artery abnormalities. | It may be caused by past heart attack (myocardial infection), abnormal heart valves, dilated cardiomyopathy, hypertrophic cardiomyopathy, myocarditis, congenital heart defects and abnormal heart rhythm. |
| Symptoms | Most cardiac attacks may occur suddenly with the unexpected loss of consciousness, pulse, and breathing. | Symptoms of left-sided heart failure may include fatigue, bluish colour of lips or fingers, sleepiness, and trouble breathing. However, symptoms of right-sided heart failure may include nausea, abdominal pain, weight gain, loss of appetite, and urination frequently. |
| Fatality | It can be dangerous if it is not treated within minutes. | It will be managed with treatment, but often progressive. |
| Treatment | It requires immediate defibrillation and CPR | It has no cure; however, treatments aim to aid a person to live longer with reduced symptoms. The choice of treatment may depend on the type of heart failure. |
| Onset | Most commonly occurs without any warning signs or symptoms. | Develops gradually over time but suddenly it may develop after heart attack. |
Frequently Asked Questions (FAQs) on Cardiac Arrest
Is cardiac arrest the same as a heart attack?
No, both conditions are not the same. Cardiac arrest is an electrical problem in the heart in which the person's heart stops pumping blood and oxygen to the brain and other organs of the body. The person who is attacked by cardiac arrest experiences symptoms such as loss of responsiveness and the absence of normal breathing and pulse. Heart attack is a circulatory problem in the heart, where the heart muscle is damaged due to the shortage of oxygen and blood caused by plaques in the coronary arteries. Heart attack symptoms include pain and chest discomfort, but the patient is awake and consists of normal breathing and pulse.
What causes cardiac arrest in young adults?
Cardiac arrest is rare in people younger than 30, but the risk increases with age. The main risk factors for cardiac arrest in younger people are genetic arrhythmias, problems with the structure of the coronary arteries or heart, heart inflammation, and substance use. Diseases including Brugada syndrome and long QT syndrome lead to SCA. Among young sportspersons who experience SCA, the cause is often an overlooked hereditary factor.
Can cardiac arrest be prevented?
Coronary heart disease (CAD) is the leading risk factor for cardiac arrest in adults. Studies have revealed that heart-healthy living prevents coronary heart disease and its complications, such as not smoking, eating healthy, and being physically active. It is highly recommended to take care of heart health and overall medical health to prevent cardiac arrest.
Is cardiac arrest hereditary?
A person may be at a higher risk for cardiac arrest if the person had a sudden cardiac arrest before or has it in his family. Have a personal or family history of abnormal heart rhythms like long QT syndrome and ventricular tachycardia.
Unexplained cardiac arrest is described as a cardiac arrest in the absence of CAD and over-structural heart disease, present in 5%-10% of cardiac arrest survivors. A genetic contribution to cardiac arrest is more common in this population, most commonly attributed to an inherited ion channel abnormality leading to familial syncope and sudden death.
What if you have already survived a cardiac arrest?
Most patients who experience cardiac arrest may not survive. Among those who do, there is a risk of developing of neurological dysfunction, brain injury, neurocognitive deficits, disorders of consciousness, changes in quality of life, and declining physical and psychological well-being. However, If the patient has survived one cardiac arrest, the risk of another one is very high. One in five cardiac arrest survivors will have another life-threatening arrhythmia within the following year.
Can caffeine cause cardiac arrest?
High usual caffeine consumption has been associated with a modestly elevated risk of primary cardiac arrest , especially in young people . For regular coffee drinkers, limiting the consumption to no more than 5-ounce cups per day is suggested. Getting too much coffee in powders, pills, or energy drinks may also lead to cardiac arrest because drinking caffeine promotes the release of noradrenaline and norepinephrine, which can increase heart rate and blood pressure in some individuals.
Can fear cause cardiac arrest?
When a person is frightened or perceives themselves to be in a dangerous situation, the brain triggers a surge of adrenaline hormones, making the heartbeat fast and instantly pushing the body into "fight-or-flight" mode. Swings of emotion are ok for people who are young and who have a healthy heart, but certainly, people with preexisting risk factors or preexisting cardiovascular disease are at high risk. An occasional rush of adrenaline cannot harm, but prolonged stress and an excess of stress hormones over time might cause negative effects such as heart rate and high blood pressure, which raises the risk of cardiac arrest.
Which is more dangerous, heart attack or cardiac arrest?
Heart attack and cardiac arrest are both profound medical emergencies. Cardiac arrest is more severe than a heart attack because it may result in death within minutes if the person doesn't receive immediate medical care. Heart attack is less immediate but can still be life-threatening if left untreated. Therefore, both conditions needed to be treated promptly to reduce the risk of major complications or death.
Sudden cardiac arrest (SCA) is a dangerous condition in which the person's heart stops beating suddenly, leading to a stoppage of blood and oxygen flow to the different organs, including the brain. If this condition is not treated promptly, SCA causes death within minutes. However, immediate treatment increases the chances of survival. A person's heart has an electrical system that controls the rhythm and rate of the heartbeat; when the person's heart's electrical system is not working correctly, irregular heartbeats lead to SCA. Irregular or abnormal heartbeats are called arrhythmias. Many arrhythmias may cause the heart to beat too slow, too fast, or with an irregular rhythm.
What is post-cardiac arrest syndrome?
Post-cardiac arrest syndrome occurs after the return of spontaneous circulation (ROSC) following cardiorespiratory arrest and involves multiple systems. Without specific and prompt treatment, it usually leads to multiple organ failure and death.
The post-cardiac arrest syndrome can be divided into four phases. The immediate post-arrest phase occurs in the first 20 minutes following the return of spontaneous circulation (ROSC). The early post-arrest phase occurs between 20 minutes and 6 to 12 hours after ROSC. Early interventions may be effective in this window of time. The intermediate phase is between 6 to 12 hours and 72 hours when injury pathways are still active and aggressive treatment can be initiated. The recovery phase extends from 3 days and beyond. It is at this point that prognostication becomes more reliable.
When to consult a doctor for cardiac arrest treatment?
Consult a doctor immediately if you suspect Cardiac Arrest (CA), as it is a life-threatening emergency where the heart suddenly stops beating effectively. Blood flow to key organs is disrupted by this disorder, mainly the brain, and can be fatal without prompt treatment. Cardiac arrest may occur due to heart rhythm disturbances, coronary artery disease, severe heart attack, or other underlying health issues.
Key warning signs include:
- Sudden collapse or loss of consciousness
- No detectable pulse or heartbeat
- Absence of regular breathing or gasping for air
- Unresponsiveness despite attempts to wake the person
- Possible chest discomfort, dizziness, or palpitations before collapse
If these warning signs occur, a Cardiac Arrest doctor or cardiologist can perform an immediate evaluation with an ECG, blood tests, and cardiac monitoring to confirm the diagnosis. Depending on the severity, treatment may include CPR, defibrillation, advanced medications, or emergency procedures to restore heart rhythm and circulation.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868