Osteoarthritis Treatment in Hyderabad, India
PACE Hospitals is known as the best hospital for osteoarthritis treatment in Hyderabad, India, offering expert care for patients experiencing joint pain, stiffness, and limited mobility. Our team consists of the best orthopaedic doctors, rheumatologists, and physiotherapists who specialize in diagnosing and treating osteoarthritis affecting the knees, hips, and hands.
As the best osteoarthritis hospital in Hyderabad, we use advanced imaging and lab tests to create personalized treatment plans based on the severity of the condition. We offer both non-surgical options—such as physiotherapy, medications, and joint injections—and surgical solutions like knee and hip replacement when necessary.
Our focus is on relieving pain, restoring joint function, and improving quality of life.
Book an appointment for
Osteoarthritis Treatment
Osteoarthritis Treatment Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Osteoarthritis Treatment?
Advanced Diagnostic Facilities: High-Resolution MRI, Digital X-Ray, Gait Analysis, Musculoskeletal Ultrasound, & Joint Function Assessment
Expert Orthopaedic and Rheumatology Specialists in Hyderabad dedicated to preserving your joints
Minimally Invasive and Regenerative Treatments tailored to all stages of Osteoarthritis
Affordable & Transparent Osteoarthritis Treatment with Insurance & Cashless Options
Osteoarthritis Diagnosis
To diagnose osteoarthritis, orthopedic specialists use a comprehensive approach that includes several crucial tests. A thorough medical history is taken at the beginning of the process to determine risk factors and symptoms. To evaluate joint function, flexibility, and any indications of pain or oedema, a comprehensive physical examination is conducted next. To rule out further potential reasons for joint discomfort, laboratory testing is also performed.
The orthopedic doctor considers the following before selecting the appropriate tests to diagnose osteoarthritis:
- Medical history
- Physical examination
Medical history: The orthopedic specialist begins by evaluating the patient’s medical history, focusing on symptoms (such as joint pain, stiffness, and functional limitations) and assessing key risk factors, including age, obesity, sex, and family background. The risk of osteoarthritis increases with age, especially after the age of 45, and is more common in women than in men. A family history of osteoarthritis may also contribute to the risk. Obesity plays a significant role, as excess body weight puts strain on weight-bearing joints, such as the knees and hips. Osteoarthritis typically presents with joint pain that worsens with movement, and after periods of rest, a phenomenon known as the gelling effect occurs. Morning stiffness is also standard, but usually lasts for 30 minutes or less. Some patients may report joint locking or a feeling of instability.
Physical examination: To evaluate range of motion, joint tenderness, swelling, and the existence of bony enlargements or deformities, a comprehensive physical examination is performed. The evaluation helps determine which joints are affected and the severity of the symptoms. Pain and reduced range of motion (ROM) are common signs of all forms of osteoarthritis. The most common joints to be afflicted are the wrists, knees, hips, and spine. However, any joint can be impacted. Osteoarthritis is typically asymmetric. A patient can have severe osteoarthritis in one knee but can be able to use the other knee almost normally.
Diagnostic evaluation of osteoarthritis
Laboratory and imaging tests in the diagnosis of osteoarthritis are essential for assessing joint pain, as they help differentiate between various causes and guide the proper course of treatment. Below are the tests involved in diagnosing osteoarthritis:
- Blood examinations: Although OA cannot be diagnosed with blood tests, an osteoarthritis specialist may order them to rule out other conditions, such as gout or rheumatoid arthritis, that can cause joint pain and inflammation. That includes the following:
- CBC (complete blood count): White blood cell and platelet values are usually within the normal range. This test is used to exclude other causes of inflammatory arthritis, joint pain, or infection, however, it is not part of the standard diagnostic criteria for osteoarthritis.
- Erythrocyte sedimentation rate (ESR): ESR values are usually within the normal range. These laboratory tests are used to exclude other causes of inflammatory arthritis, joint pain, or infection, however, they are not part of the standard diagnostic criteria for osteoarthritis.
- Rheumatoid factor (RF) and anti-nuclear antibody (ANA): These are suitable in cases where there is clinical evidence of synovitis or joint inflammation, which would arouse suspicion of autoimmune arthritis, such as systemic lupus erythematosus or rheumatoid arthritis.
- X-ray: The primary imaging technique for OA is X-rays. They can exhibit distinctive characteristics that aid in diagnosis confirmation and assessment of disease severity, such as subchondral sclerosis, osteophyte (bone spur) formation, joint space narrowing, and bone remodelling. Standard X-rays, however, cannot show early cartilage loss or soft tissue changes.
- MRI scan (magnetic resonance imaging): Joint examination using MRI is effective, particularly when symptoms such as locking or instability are present. It provides fine-grained images of soft tissues that X-ray cannot display, including cartilage, muscles, ligaments, and tendons. MRI supports personalised treatment decisions, aids in the identification of soft tissue injuries (such as tears in tendons, ligaments, or meniscus), and guides management between conservative care and surgery by identifying subtle or early joint changes.
- Joint aspiration: It is also known as arthrocentesis, a standard procedure in which a local anaesthetic is used to numb the area around the joint before a small needle is used to withdraw synovial fluid. It is used mainly in osteoarthritis to rule out alternative causes of joint pain, such as infection, gout, or pseudogout, by examining the fluid for crystals or symptoms related to infection. The procedure helps rule out these alternative diagnoses, but is not routinely required for OA. While history, tests, and imaging are used to diagnose osteoarthritis, joint aspiration is crucial when the source of symptoms is unknown or when infection or crystal-induced arthritis is suspected.
- Ultrasound: Given its high sensitivity and accuracy in detecting osteoarthritis osteophytes, joint inflammation, meniscus protrusion, and localised cartilage damage, ultrasound is increasingly recognised as a valuable imaging modality for osteoarthritis, particularly in the knee and hand joints. Due to its cost, safety, and ability to visualise both structural and inflammatory changes, ultrasonography is a tool used for bedside assessment and monitoring in clinical practice, even though it is not considered a laboratory test. Based on current reviews and thorough studies, ultrasonography often outperforms standard radiography in several aspects of evaluating osteoarthritis; it is less useful for early disease detection and works best when used in conjunction with radiography and clinical evaluation.
Stages of Osteoarthritis
The stepwise progression of osteoarthritis, as described by the Kellgren-Lawrence Classification system, is widely used to characterise the radiographic progression of osteoarthritis, particularly in the knee, but is also applicable to other joints. The system includes five grades, each reflecting increasing severity. Below are the different stages of osteoarthritis:
- Stage 0 (No Osteoarthritis): At this stage, there are no signs and symptoms of osteoarthritis. X-ray imaging reveals a normal looking joint, and individuals will not experience functional disability or pain. The joint functions as expected, with no signs of degeneration or pain.
- Stage 1 (Doubtful): In this stage, alterations are minimal and may not be easily detected. X-ray results may show the presence of small osteophytes or a possible, but doubtful, narrowing of the joint space. Most individuals at this stage have very minor or no noticeable symptoms, and daily activities are generally unaffected.
- Stage 2 (Minimal): This stage marks the onset of early but noticeable signs of osteoarthritis. X-rays demonstrate definite osteophytes and possible joint space narrowing. Clinical features include minor symptoms such as occasional stiffness or discomfort, which may come and go but do not significantly interfere with daily life.
- Stage 3 (Moderate): At this stage, osteoarthritis is considered moderate, with more noticeable changes visible on imaging. X-rays show multiple osteophytes, an apparent narrowing of the joint space, and possibly some bone sclerosis. Clinically, individuals may experience swelling, increased stiffness, and moderate pain, all of which can begin to interfere with everyday activities.
- Stage 4 (Severe): This stage represents advanced osteoarthritis, characterised by severe changes on X-ray imaging. Findings include marked bone sclerosis and deformity, large osteophytes, and a noticeable narrowing of the joint space. Clinical features include prolonged stiffness, severe pain, substantial loss of function, and potentially unstable joints.
Osteoarthritis Differential Diagnosis
The differential diagnosis of osteoarthritis (OA) involves distinguishing it from other conditions that can present with same symptoms, including joint pain, swelling and stiffness. This includes the following conditions:
- Rheumatoid arthritis (RA): It is characterized by symmetrical involvement of minor joints, particularly the wrist, metacarpophalangeal (MCP) joints, and proximal interphalangeal (PIP) joints; prolonged morning stiffness (>1 hour); systemic symptoms, such as fever, fatigue, and weight loss; and elevated inflammatory markers.
- Psoriatic arthritis: It is linked to dactylitis, nail abnormalities, psoriasis, and frequently asymmetric joint involvement.
- Other inflammatory arthritides: These include systemic lupus erythematosus and ankylosing spondylitis, which can manifest as systemic symptoms and joint pain.
- Arthropathies of the crystalline: The first Metatarsophalangeal joint (MTP) joint is frequently affected by gout, which is characterized by acute, intense joint pain, erythema, oedema, and warmth. It might resemble an OA flare-up, but is typically more inflammatory. Like gout, calcium pyrophosphate deposition disease (CPPD) commonly affects the knee or wrist and can be distinguished through joint fluid analysis.
Periarticular system diseases include the following conditions:
- Bursitis: It is characterized by localized soreness and swelling, which often affects the bursae (such as the trochanteric or olecranon bursae) rather than the joint itself. The discomfort is frequently triggered by movement or pressure on the affected area.
- Tendonitis: A condition known as tenosynovitis is characterised by sensitivity and pain along tendons, which are most typically found in the hand, elbow, or shoulder. Symptoms are usually exacerbated by activity involving the specific tendon.
- Periostitis: It causes bone discomfort due to inflammation of the periosteum resulting from recurrent stress or trauma, leading to localised pain over the affected bone.
- Arthritis septic: The symptoms of septic arthritis include fever, palpable erythema, warmth, and severe monoarticular joint pain. Due to a medical emergency, a combined aspiration and culture are urgently needed for diagnosis.
- Fractures: Positive imaging results, a history of trauma, and localised pain are signs of fractures. At the site of the injury, symptoms include pain, oedema, deformity, and potential loss of function.
- Osteonecrosis (Avascular Necrosis): The abrupt onset of pain, frequently in the knee or hip, and characteristic imaging findings are hallmarks of osteonecrosis, also referred to as avascular necrosis. It could lead to joint dysfunction and a restricted range of motion.
- Malignancy: Primary tumours or metastatic illnesses that affect the bones can cause chronic or unusual joint pain. Imaging and biopsy are used to confirm the diagnosis.
- Ligament or meniscal injuries: These commonly occur in the knee and are generally linked to mechanical symptoms like locking or giving way, frequently accompanied by a history of trauma.
- Patellofemoral pain syndrome: Anterior knee discomfort in young individuals is a common symptom of patellofemoral pain syndrome, which is not associated with radiographic signs of osteoarthritis.
- Referred pain: It is when a joint, such as the knee, experiences pain that comes from somewhere else, like the hip or spine (e.g., spinal stenosis or radiculopathy). The afflicted joint could fail to exhibit any local findings.
Osteoarthritis Treatment Goals
The following are the main objectives of osteoarthritis (OA) management:
- Reduce pain: Since pain is a common complaint that lowers quality of life, minimising suffering is a key goal.
- Preserve or enhance joint function and mobility: A patient's independence depends on their capacity to carry out everyday tasks.
- Slow disease progression: While there is currently no cure for osteoarthritis (OA), available treatments focus on slowing disease progression and preventing further joint damage.
- Enhance quality of life: This involves attending to social engagement, psychological health, and physical ailments.
- Lower the risk of complications and falls: OA can cause muscle weakness, decreased mobility, and balance problems, which raises the risk of fractures and falls. Maintaining activity and preventing falls are two key management techniques.
Treatment of Osteoarthritis primarily aims at enhancing joint function, reducing pain, and, when possible, slowing the progression of the disease. Currently, most available treatments focus on alleviating symptoms rather than altering the underlying disease course. It includes the following:
Medical management of osteoarthritis
- NSAIDs and Analgesics
- Intraarticular Injections
- Polysaccharide (Viscous Supplementation)
- Topical Pain Relievers
- Antidepressants
- Dietary and Vitamin Supplements
New treatments for osteoarthritis include:
- Regenerative Medicine
- Gene Therapy
- Biologic Agents
- ACE Inhibitors and Angiotensin Receptor Blockers (ARBs)
Nonpharmacological management of osteoarthritis
- Osteoarthritis Physical Therapy (Physiotherapy)
- Tai Chi Exercises for Osteoarthritis and Yoga
- Osteoarthritis Exercises
- Heat Therapy
Supportive or Assistive Management
- Assistive Equipment
- Weight Loss for Osteoarthritis
- Group Exercise
- Transcutaneous Electrical Nerve Stimulation (TENS)
- Creative Visualization
Surgical Management of Osteoarthritis
- Arthroscopic Surgery
- Osteotomy
- Joint Fusion (Arthrodesis)
- Joint Replacement (Arthroplasty)
Medical management of osteoarthritis
- NSAIDs and analgesics: Nonsteroidal anti-inflammatory drugs (NSAIDs) are usually used to treat inflammation and pain, both orally and topically. Commonly prescribed for minor pain management with a lesser risk of gastrointestinal side effects.
- Intraarticular injections: Corticosteroid intra-articular injections, administered directly into the joint, can provide temporary pain relief, particularly during flare-ups.
- Polysaccharide: Viscous supplementation injections may provide longer-term symptom relief for specific individuals, although the results vary.
- Topical Pain Relievers: Creams or gels containing non-steroidal anti-inflammatory drugs can be applied to the joint that is affected to provide localised pain relief, and counterirritant creams containing a topical analgesic agent may help relieve pain by altering pain signals at the site of application.
- Antidepressants: Certain antidepressants, like serotonin-norepinephrine reuptake inhibitors, are used to treat chronic pain, particularly when there is a neuropathic component.
- Dietary and vitamin supplements: These are widely used; however, the evidence for their effectiveness is conflicting. Herbal supplements may provide mild anti-inflammatory benefits when taken. Vitamin D and omega fatty acids may support joint health and can help relieve osteoarthritis symptoms.
New treatments for osteoarthritis include:
- Regenerative Medicine: Biological regenerative therapy is being investigated for its potential to repair cartilage and alleviate pain.
- Gene Therapy: Experimental techniques for cartilage regeneration and inflammation are being investigated.
- Biologic: agents targeting specific cytokines that cause inflammation are a promising area of research.
- ACE inhibitors and angiotensin receptor blockers (ARBs): Several cardiovascular drugs, including angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), are currently being explored for their potential anti-inflammatory effects and ability to protect cartilage in osteoarthritis.
Nonpharmacological management of osteoarthritis
Non-pharmacological therapy of osteoarthritis is a cornerstone of treatment, with the goal of relieving symptoms, improving function, and slowing disease progression without the use of drugs. A variety of evidence-based techniques suited to the individual's needs include:
- Osteoarthritis physical therapy (physiotherapy): Physical therapy is an essential component of controlling osteoarthritis. It relieves pain, improves joint function, and restores mobility for everyday tasks. Physical therapy improves quality of life by promoting long-term joint health through targeted workouts and interventions.
- Tai chi exercises for osteoarthritis and Yoga: Although the evidence is conflicting, some guidelines conditionally recommend yoga for knee osteoarthritis due to its positive effects on strength, flexibility, and mental health.
- Osteoarthritis exercises: For patients with osteoarthritis, physiotherapy exercises are highly effective and include both supervised and home-based activities. These exercises may involve strength training, such as squats and lunges, balance exercises like single-leg stands, and low-impact aerobic activities like walking, cycling, and swimming. Combining supervised sessions with regular home exercises leads to the best improvements in pain and joint function; however, stopping exercise can cause benefits to fade, so sticking to a routine is important for lasting results.
- Heat Therapy: It often helps in conjunction with other treatments; heat application can be comforting and help control oedema.
Supportive or Assistive Management
- Assistive equipment: For individuals with osteoarthritis, carefully designed footwear or cushioned insoles can help improve walking patterns and reduce strain on lower limb joints. Crutches, walking sticks and canes are examples of assistive equipment that can help redistribute weight and relieve discomfort, thus improving mobility for those with moderate to severe joint impairment. Knee braces provide extra support and alignment during weight-bearing exercises, which helps to alleviate pain. Splints are used to stabilise joints, especially in the hands, and supportive dressings can help minimise oedema and provide additional joint support. Custom or over-the-counter orthotic devices can further optimise foot and lower limb alignment, thereby reducing joint tension and enhancing overall foot and lower limb functionality.
- Weight Loss for Osteoarthritis: It is highly recommended that overweight individuals with osteoarthritis aim to lose a clinically meaningful amount of weight, such as 4–9 kg for a person weighing 80 kg (representing 5–10% of body weight), as this can significantly reduce functional limitations and discomfort associated with osteoarthritis in the knees and hips.
- Group Exercise: When compared to individual at-home programs, group exercise or activity sessions enhance adherence and results.
- Transcutaneous Electrical Nerve Stimulation (TENS): Some patients may have short-term pain alleviation.
- Creative Visualisation: Methods like these can enhance pain management and general well-being by reducing stress and despair.
Surgical management of osteoarthritis
Treatment of Osteoarthritis Surgically included the following:
- Arthroscopic surgery: Although there is little evidence of long-term benefits in osteoarthritis, arthroscopic surgery is used for diagnostic purposes and to treat mechanical symptoms (such as loose bodies and meniscal tears).
- Osteotomy: In younger, active patients with early osteoarthritis, osteotomy—a surgical realignment of the bones to redistribute weight away from damaged joint areas—is frequently utilised. When joint replacement is not practical,
- Joint fusion: It is also known as arthrodesis, is a surgical procedure that will permanently join the bones of a joint. This process eliminates movement at the joint, which can help reduce pain and stabilise the area; however, it also results in a loss of mobility.
- Joint Replacement (Arthroplasty): For end-stage osteoarthritis, joint replacement surgery (arthroplasty or total joint replacement) is considered the gold standard. This surgery involves replacing the damaged joint with an artificial implant, which significantly reduces pain and improves joint function and overall quality of life.
Osteoarthritis Prognosis
The prognosis of osteoarthritis depends on the extent of joint involvement, symptom severity, and the degree of functional impairment. OA is a chronic, progressive condition for which there is currently no cure; however, symptoms can be managed, and quality of life can be improved with appropriate treatment. Most patients will need to manage their symptoms over the long term. The following factors influence prognosis:
- Joint involvement: The course of the illness depends on the joints involved (e.g., knee, hip, hand, spine) and whether multiple joints are affected.
- Pain and Function: Severe pain and loss of function usually predict a worse prognosis.
- BMI and Age: Older age (over 45) and a higher body mass index (BMI) are both strongly associated with a greater risk and faster progression of knee osteoarthritis, particularly in weight-bearing joints. Research demonstrates that these factors are among the most significant modifiable and non-modifiable risk factors for the development and progression of osteoarthritis.
- Other osteoarthritis risk factors: The prognosis can be significantly impacted by other osteoarthritis risk factors, including varus deformity, multiple joint involvement, and the presence of comorbidities.
- Surgical Intervention: Hip and knee replacements have success rates above 90%, improving quality of life. After 10–15 years, younger, more active patients may need revision operations. Weight loss, exercise, and patient education can help alleviate symptoms and slow disease progression, emphasising the importance of ongoing treatment and self-management.
Osteoarthritis is a lifelong illness, but appropriate care can help most patients preserve function and quality of life.
Frequently Asked Questions (FAQs) on Osteoarthritis
What are the symptoms of osteoarthritis?
The symptoms include reduced flexibility, joint stiffness (especially after periods of inactivity), soreness, swelling, and pain that typically worsen with movement and improve with rest. Some people also experience joint instability or a sensation of grating.
How to detect osteoarthritis?
The diagnosis involves a physical examination, medical history, and imaging tests such as Magnetic Resonance Imaging (MRI) or X-rays. Blood tests may be used to exclude other types of arthritis.
What lifestyle modifications aid in the treatment of osteoarthritis?
Maintaining a good healthy weight, engaging in regular low-impact exercise, protecting joints, using supportive footwear, and avoiding activities that stress the joints are essential for reducing pain and slowing progression.
Can osteoarthritis be cured by surgery?
Yes, it can be cured by surgical options that include joint replacement, joint fusion, osteotomy, and arthroscopy. Surgery is opted for when other treatments fail to relieve pain or restore function.
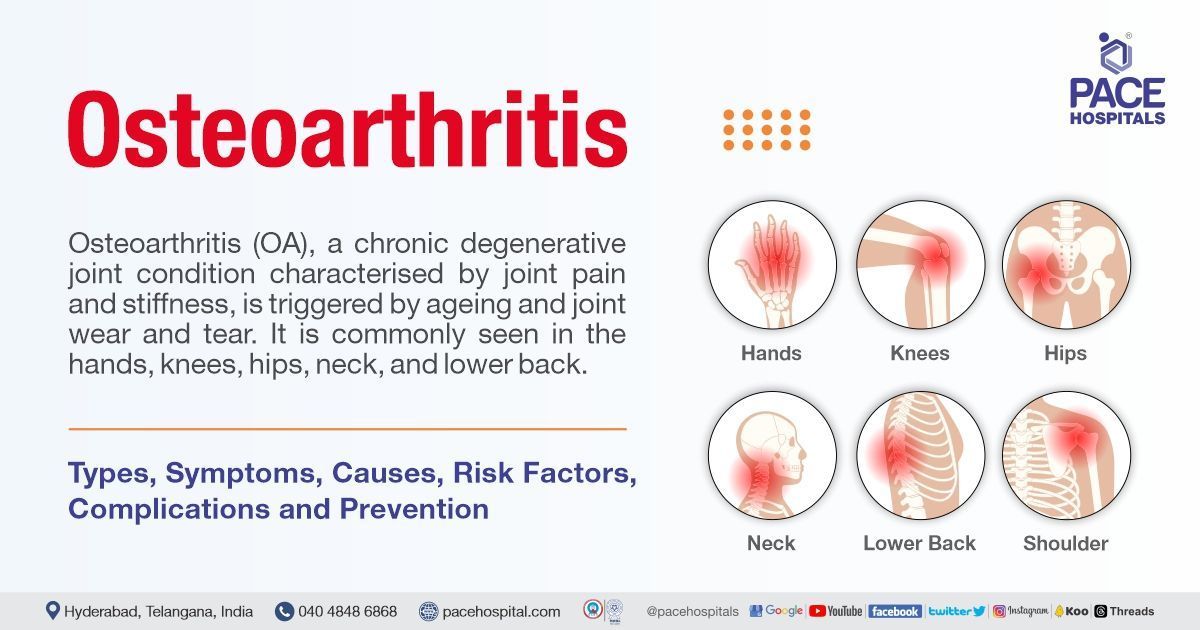
What is osteoarthritis?
Osteoarthritis is a chronic, degenerative joint disease primarily characterised by the gradual breakdown of cartilage, resulting in joint pain, stiffness, and reduced mobility. It commonly affects the hands, knees, hips, and spine and is the most prevalent form of arthritis globally.
How does osteoarthritis occur?
Osteoarthritis develops primarily due to ageing, genetic predisposition, joint overuse, and previous joint injuries. Additional risk factors include joint misalignment and excess weight, both of which increase the risk of cartilage damage and joint deterioration.
Who can get osteoarthritis?
Anyone can develop OA, but the risk is higher in individuals with a family history of the disease, those who are overweight, people with past joint injuries, and older adults. Women are more likely than men to develop OA, especially after age 50.
What is the best prescription medication for osteoarthritis?
Common medications are non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief. Topical creams, oral medicines, and sometimes antidepressants are also used. Injections (such as corticosteroids) may be recommended for severe pain.
How well do osteoarthritis supplements work?
The majority of osteoarthritis supplements show little to no clinically meaningful benefit in the medium or long term; widespread supplements have minor, frequently clinically insignificant effects. However, they can offer moderate, short-term improvements in pain and function. While some particular supplements (like ginger and curcumin) may have noticeable short-term effects, the quality of the evidence is generally poor, and study results vary.
In osteoarthritis, what part does physical therapy play?
Physical therapy helps strengthen muscles, reduce pain, and improve joint function. Therapists create personalised exercise plans to support joint health and mobility.
Does osteoarthritis improve with heat or cold therapy?
Yes, heat therapy can increase flexibility and relieve stiffness, while cold therapy helps numb pain and reduce swelling. Both can be used as needed to manage symptoms.
Can more than one joint be impacted by osteoarthritis?
Yes, osteoarthritis often affects multiple joints, especially in older individuals. While any joint can be involved, the knees, hands, hips, and spine are most affected.
Which exercise is best for osteoarthritis?
Low-impact exercises that enhance cardiovascular health, strength, and flexibility are generally recommended for individuals with osteoarthritis. These include activities that focus on balance and gentle movements, such as yoga and tai-chi, as well as walking, cycling, swimming, and water aerobics. Using resistance bands or small weights for strength training can also be helpful.