Best Hydrocele Treatment Hospital in Hyderabad, India
PACE Hospitals is recognized as the best hospital for hydrocele treatment in Hyderabad, Telangana, India, providing exceptional urological care with a patient-centric approach. Our expert urologists specialize in diagnosing and treating hydrocele using the latest medical advancements, ensuring a seamless experience from consultation to recovery.
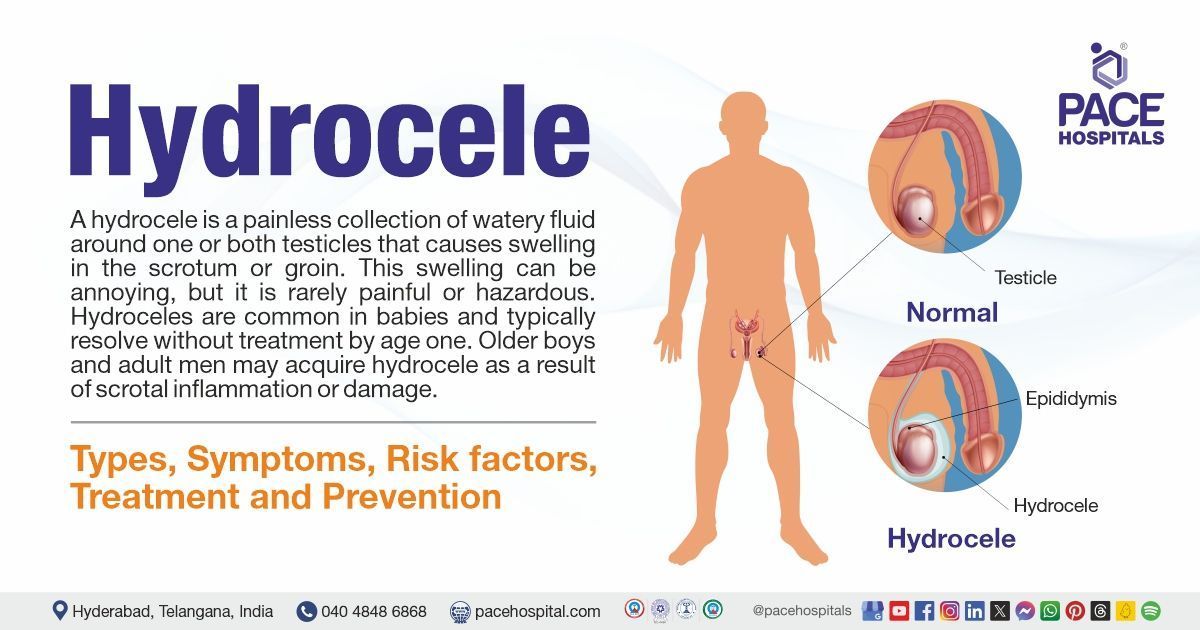
Hydrocele is a condition where fluid accumulates around the testicles, leading to swelling and discomfort. While often painless, it can cause discomfort, heaviness, or cosmetic concerns. At PACE Hospitals, our top urologists offer the
best treatment for hydrocele, including non-surgical and surgical treatment options, such as aspiration, sclerotherapy, and hydrocelectomy (surgical removal) for long-term relief. Our state-of-the-art facilities and minimally invasive procedures ensure faster recovery and reduced post-treatment complications.
Book an appointment for Hydrocele Treatment
Hydrocele Treatment Appointment
Why Choose PACE Hospitals for Hydrocele Treatment?

State-of-the-art Facilities, Minimally Invasive Surgery
Team of Best Urologists in Hyderabad, India
24/7 Emergency Care & Post-Surgical Support
Affordable & Reliable Hydrocele Treatment
Hydrocele diagnosis
A hydrocele is an accumulation of fluid in the scrotum that can be detected through a clinical examination of hydrocele that includes taking history, a physical examination, and imaging tests. The urologist considers the following before selecting the appropriate tests to diagnose hydrocele:
- Hydrocele history taking
- Hydrocele examination
Hydrocele history taking
During the process of history taking, the urologist may ask regarding the onset, duration, and severity of signs and symptoms, and identify any relevant genitourinary (GU) history, sexual history, recent trauma, exercise, or systemic illnesses.
The urologist/andrologist may ask the patient regarding:
- Pain: The presence of pain or discomfort in the scrotum
- Swelling: Whether the scrotum or testicles are swollen and if the swelling changes in size throughout the day
- Travel history: Whether the patient has lived or travelled in a region where filariasis (Parasitic infection ) is prevalent.
Hydrocele examination
The urologist/ andrologist initiates a hydrocele examination to look for discomfort, and swelling, in the scrotum. The doctor may also look for:
- An inguinal hernia by pressing the abdomen and the scrotum
- Fluid accumulation by shining a light through the scrotum to check if the fluid around the testicle is clear.
- Changes in swelling by asking the patient to cough
The examiner may examine the hydrocele in both the upright and supine positions. During the examination, the urologist/andrologist may ask the following questions:
- Is it possible to get above the swelling and palpate the cord? If not, this could indicate a hydrocele (congenital or infantile) or a hernia. A hernia differs from a hydrocele, in that it has an expansile cough impulse and is reducible but lacks transillumination and fluctuations.
- Does the swelling originate in the testis or epididymis, or does it encompass both of these structures? Hydroceles often surround the testes and epididymis, making them impalpable.
- Does the swelling transilluminate?
✅Imaging tests for hydrocele
Based on the above information a urologist might recommend the following diagnostic tests for hydrocele. These tests are useful for identifying and evaluating hydrocele. They can also look for underlying causes such as epididymitis, testicular torsion, or testicular tumor.
Hydrocele ultrasound (Ultrasonography)
Scrotal pain or failure to distinguish testicular tissue on examination are indications for ultrasonography, which provides great detail of the testicular parenchyma. During an ultrasonography examination, a hydrocele presents as an anechoic or echolucent region around the testis. Ultrasonography could potentially aid in the measurement and characterization of the hydrocele. Spermatoceles, testicular tumors, and testicular atrophy can all be clearly recognized with ultrasonography. The patient needs to be evaluated in both supine and upright postures since hydrocele tends to diminish into the abdomen depending on the position of the patient.
Duplex Ultrasonography
It provides information on testicular blood flow, which will be diminished or nonexistent in hydroceles caused by testicular torsion. However, if the hydroceles are caused by epididymitis, the epididymal flow will be increased. Duplex investigations also aid in the identification of Valsalva-augmented regurgitant flow in varicoceles.
Plain abdominal radiography
Plain abdominal radiography can help identify an acute hydrocele from an incarcerated hernia. For instance, gas above the groin could indicate an incarcerated hernia.
Computed tomography
Computed tomography (CT) is commonly used in imaging tests for abdominoscrotal hydroceles to assess the true amount of the intraabdominal component.
Transillumination test in hydrocele
The transillumination test for hydrocele involves a light that is directed through the scrotum to see the clear fluid surrounding the testicle. It allows the urologist /andrologist to quickly detect whether the mass is cystic (light shines through) or solid (light is obstructed by the mass).
✅Histological findings
In terms of basic histology, certain features can assist urologists in diagnosis and allowing them to distinguish hydrocele from other scrotal diseases. For example, the existence of inflammatory cells and prominent lymphatic proliferation may indicate inflammation or infection whereas simple hydrocele is achy and may not show any structural changes. The mesothelial lining, smooth muscle, scanty lymphatic vessels, lacking inflammatory cells, and thickened tunica vaginalis are important to consider because they are required in the management of hydrocele.
Some of the histological findings include:
Fluid composition
The fluid within the hydrocele can vary; it is often clear, but it may also contain a high protein concentration, resulting in hypoechoic or echogenic appearances on imaging investigations. This difference may be attributable to underlying diseases like inflammation or infection.
Inflammation and fibrosis
In some cases, particularly those associated with comorbidities such as endometriosis, a histological investigation may indicate inflammation, fibrosis, and haemosiderin (iron storage) accumulation. These results indicate chronic inflammation or bleeding within the sac.
Other pathological changes
In cases where the hydrocele is worsened by infection or hemorrhage, histology may show signs of a complex appearance with thicker walls or internal septation, which indicates changes in fluid dynamics and cellular response to injury.
✅Differential diagnosis of hydrocele
A hydrocele often causes painless scrotal enlargement. Differentiating it from similar illnesses, such as inguinal hernias or testicular tumors, is critical for appropriate diagnosis and patient care.
Differential diagnoses of hydrocele include:
- Inguinal hernia
- Epididymal cyst
- Testicular tumor
- Scrotal edema
- Varicocele
Inguinal hernia: An inguinal hernia, also known as a groin hernia, is a bulge or lump in the groin caused by tissue pushing through a weak area in the abdominal muscles.
Epididymal cyst: Spermatocele, also known as an epididymal cyst, is a benign, fluid-filled cyst that forms in the epididymis, a coiled tube behind the testicle that stores and transports sperm.
Testicular tumor: Testicular cancer develops when cells in one or both testicles grow abnormally and uncontrollably. As the cells expand uncontrollably, they frequently create tumors. In certain circumstances, these tumors are benign, which means they do not spread to other parts of the body.
Scrotal edema: Scrotal edema is a swelling of the scrotal sac, or scrotum, which contains the testicles. Injury, an underlying medical condition, fluid buildup, inflammation, or abnormal growth within the scrotum can all be the causes.
Varicocele: Varicocele is a disorder marked by the growth of veins within the scrotum, comparable to varicose veins in the legs. It is caused by diminished blood flow in the testicular veins, which can result in decreased testicular function and lower fertility.
✅Considerations of a surgeon before opting for a hydrocelectomy
Before performing a hydrocelectomy, a surgeon may examine several crucial criteria to achieve the best possible results for the patient. Here are the main considerations:
Medical Evaluation
Patient history: Understanding the patient's medical history, including underlying diseases, allergies, and current medicines, is critical. This aids in determining the risks connected with anesthesia and surgery.
Physical examination: A complete physical examination, including procedures such as transillumination and ultrasound, may be required to confirm the diagnosis and define the hydrocele's features (e.g., communicating vs. non-communicating).
Hydrocele Characteristics
Size and symptoms: The extent of the hydrocele and the patient's symptoms (such as pain or discomfort) play an important part in determining if surgery is indicated. Larger hydroceles, or those producing substantial discomfort, often need surgical intervention.
Duration: If the hydrocele persists for more than six months without improvement, surgery may be indicated to avoid problems such as infection or hernia formation.
Surgical Options
Type of procedure: Surgeons may discuss several surgical alternatives with patients, such as open hydrocelectomy, less invasive methods, and aspiration with sclerotherapy. Each choice comes with varying recovery timelines and hazards.
Anaesthesia considerations: The decision between general and local anaesthesia is done based on the patient's health and preferences, as well as the complexity of the intended procedure.
Risks and Complications
Potential risks: Surgeons must educate patients about potential consequences such as infection, haematoma (A firm bulge of clotted blood), recurrent fluid accumulation, and tissue damage. Understanding these hazards enables patients to make informed decisions.
Postoperative care: Surgeons may discuss recovery expectations, such as pain management and activity restrictions after surgery, is critical to achieving a successful recovery.
Patient preferences
Informed consent: It is critical that patients are completely aware of their disease, treatment options, potential hazards, and expected outcomes. This includes discussing any lifestyle adjustments that may be required following surgery to prevent hydroceles recurrence.
Support systems: Surgeons should ensure that patients have enough home support during their recovery period, including transportation arrangements after surgery owing to probable anesthesia effects.
By carefully evaluating these criteria, surgeons can improve patient safety and surgical outcomes during hydrocelectomy procedures.
✅Goals of hydrocele treatment
The goals of hydrocele treatment include:
- Symptomatic relief
- Restoration of normal anatomy
- Prevention of complications
- Long term resolutions
Hydrocele treatment
When treating hydrocele, the surgeon follows specific treatment goals. These goals govern the therapeutic approach, delivering the best possible outcomes for patients. By focusing on symptom treatment, anatomical restoration, and complications prevention, overall quality of life is improved, and recurrence can be reduced. Hydrocele management includes the following:
Hydrocele treatment for children
If communicative hydroceles persist beyond the first year or two of life in children, they are surgically treated. Large noncommunicating hydroceles may also require surgical intervention.
If the child also has a hernia, it will normally be repaired at the same operation (during hydrocele repair).
A hydrocele is treated by making a very small cut in the lower abdomen or scrotum. Sometimes the procedure is performed through a keyhole (laparoscopically). The fluid is then drained from the testicle. The channel between the abdomen and scrotum will also be shut, preventing the fluid from reforming in the future. This is a small operation that is normally performed on the same day, so there is no need to stay in the hospital overnight.
Hydrocele treatment for adults
While yoga may help with hydrocele symptoms, it is essential to consult with a urologist for more complete options for treatment. For hydroceles that are persistent or symptomatic, Minimal invasive surgery is considered the gold standard.
Surgical management of hydrocele
Surgery is the preferred treatment for hydrocele, and it is necessary when the hydrocele becomes difficult or symptomatic. There are two sorts of surgical interventions that can be equally beneficial.
- Aspiration and sclerotherapy
- Hydrocele surgery (Hydrocelectomy)
Aspiration and sclerotherapy
A needle can be put into the fluid, and the fluid will drain into a syringe. However, the fluid normally recovers rapidly. Sclerotherapy involves injecting a chemical into the region to harden it and prevent additional fluid accumulation. A typical sclerosing agent is used in this procedure.
The negative effects include the recurrence of the hydrocele and partial gangrene (scrotal tissue death). This is frequently utilized when a person is too fragile to undergo more thorough surgery.
Hydrocele surgery (Hydrocelectomy)
There are two commonly used surgical methods for hydrocelectomy:
- Plication
- Excision and eversion
Plication: Plication of the hydrocele sac is appropriate for thin-walled hydroceles. Because there is minimal dissection, the risk of hematocele or infection is greatly decreased. Lord plication is the process of bunching the tunica into a ruff using a series of many interrupted chromic catgut sutures such that the sac forms fibrous tissue.
Excision and eversion: This procedure (hydrocele excision and eversion) is appropriate for large, thick-walled hydroceles and chyloceles (accumulation of milky fluid in the scrotum). It entails subtotal excision of the tunica vaginalis, everting the sac behind the testes, and putting the testes in a newly formed pocket between the scrotum's fascial layers (Jaboulay procedure). The epididymis, testicular arteries, and ductus deferens are all carefully protected from injury.
✅Hydrocele prognosis
Congenital hydrocele has a good prognosis, however adult-onset hydrocele is dependent on the underlying reason.
Usually, congenital hydroceles go away on their own by the end of the first year of life. They have good long-term prognosis and a high success rate when surgically addressed if they persist. The risks of testicular injury or recurrence is extremely low when hydrocele surgery is performed by skilled professionals.
The underlying cause of adult-onset hydrocele largely determines the outcome. The extent and degree of lymphatic blockage, for example, determine the prognosis of filarial hydrocele.
Frequently Asked Questions (FAQs) on Hydrocele Treatment
Is hydrocele hereditary?
Hydroceles can occasionally be seen in most family members, although there is no known hereditary basis for their occurrence. The majority of cases are congenital or acquired as a result of environmental or health-related circumstances, rather than a genetic predisposition.
Is hydrocele operation painful?
No, patients will not experience discomfort or pain during hydrocele surgery because they will be under general anaesthesia. During the process, the patient is put into a deep sleep-like state.
Is hydrocele surgery dangerous?
Hydrocele surgery, also known as hydrocelectomy, is generally regarded as safe, but there are certain risks. A study discovered that 16.1% of patients experienced moderate to severe problems after 90 days of surgery, including infection and reoperation in certain cases. Despite the hazards, the treatment is frequently required for symptomatic relief.
What are the best treatment options for filarial hydrocele, and can it be treated without surgery?
Filarial hydrocele is a condition caused by lymphatic filariasis, a parasitic infection that leads to fluid accumulation in the scrotum, resulting in swelling, discomfort, and restricted mobility. At PACE Hospitals, our expert urologists and infectious disease specialists provide advanced treatment for filarial hydrocele, focusing on both medical management and surgical intervention.
Treatment options include anti-filarial medications to eliminate the parasite, compression therapy to reduce swelling, and hydrocelectomy surgery for severe cases where fluid removal is necessary. With state-of-the-art facilities and personalized care, our minimally invasive surgical techniques ensure a faster recovery with minimal discomfort.
What is encysted hydrocele, and what are the best treatment options?
Encysted hydrocele, also known as hydrocele of the spermatic cord, occurs when fluid collects along the spermatic cord, leading to a small, movable swelling in the groin or scrotal area. While often painless, it can cause discomfort, tenderness, or cosmetic concerns.
Our expert urologists offer the best treatment for encysted hydrocele, including observation for mild cases, aspiration with sclerotherapy for temporary relief, and hydrocelectomy surgery for permanent resolution. Our minimally invasive surgical techniques ensure faster recovery, minimal scarring, and reduced complications.
How can septated hydrocele be treated effectively?
Septated hydrocele is a rare condition where fluid accumulates in the scrotum, divided by thin tissue walls (septa), creating multiple fluid-filled compartments. This condition may cause swelling, discomfort, or heaviness in the scrotum; in some cases, it can lead to complications if left untreated.
The best treatment for septated hydrocele includes observation for mild cases, aspiration and sclerotherapy for temporary relief, and hydrocelectomy surgery for long-term resolution. We use advanced diagnostic imaging to assess the condition accurately and offer minimally invasive surgical techniques to ensure faster recovery with minimal discomfort.
What are the best treatment options for funicular hydrocele?
Funicular hydrocele occurs when the processus vaginalis remains partially open, allowing fluid to accumulate along the spermatic cord but not communicating with the abdominal cavity. This condition can cause scrotal or groin swelling, discomfort, or a feeling of heaviness.
The best treatment for funicular hydrocele, including observation for mild cases, aspiration with sclerotherapy for temporary relief, and hydrocelectomy surgery for a permanent solution. We specialize in minimally invasive procedures that ensure quicker recovery, minimal scarring, and reduced post-operative complications.
How much time does it take to cure hydrocele?
The time it takes to cure hydrocele varies depending on the type of treatment used. Sclerotherapy allows for an instantaneous return to normal activities, whereas hydrocelectomy usually takes around 15 days to fully recover. Congenital hydroceles can heal spontaneously within a year, although surgical intervention is frequently required for symptomatic relief in adulthood.
Can persons with hydrocele do walking regularly?
Individuals with hydrocele are usually able to walk regularly. Walking is suggested after surgery because it improves blood circulation and helps with rehabilitation. Patients are encouraged to gradually raise their activity level while listening to their bodies, to avoid discomfort or strain during the healing process.
Can hydrocele effect PSA level?
Yes. Sometimes hydrocele can be a sign of prostate cancer if it is cancerous and results from a paratesticular metastasis. There have been cases reported of higher PSA levels in patients with hydrocele.
Can primary hydrocele be cured without surgery?
Yes, if a primary hydrocele is congenital and resolves on its own by the end of the first year of life, surgery is not required. However, if the hydrocele persists, surgery can correct it with a high success rate and a favorable long-term prognosis.
Does hydrocele cause weakness?
Hydrocele does not often result in weakness. However, if it causes difficulties, like increased pressure on adjacent structures, it may indirectly contribute to discomfort or weakness in the affected area.
Does working out cause hydrocele?
Yes. Working out may cause injury to the testicular region. This might result in fluid collection in the scrotum. Strenuous activities may put pressure on the abdominal and groin areas, which might lead to fluid accumulation.
Does varicocele cause hydrocele?
Hydrocele formation is the most common consequence of varicocele repair. The onset of this type of hydrocele is variable. The shortest documented onset time is one week. In this context, we document an uncommon beginning of hydrocele formation after varicocele repair.
Can a female doctor do hydrocele treatment?
Yes, a female doctor can treat hydrocele, especially if she is a urologist or general surgeon who specialises in this area. Hydrocele treatment consists mostly of surgical techniques, such as hydrocelectomy, which can be performed by qualified medical specialists regardless of gender.
Does hydrocele cause cancer?
A hydrocele is a common disorder that is not generally carcinogenic (cancerous), however, it can occasionally be an early indicator of testicular cancer.