Nephrology Hospital in Hyderabad for Kidney Disease Treatment
PACE Hospitals is one of the Best Nephrology Hospital in Hyderabad, offering evidence-based treatment for all kinds of acute and chronic kidney diseases.
The team of skilled and experienced nephrology doctors have vast expertise in managing advanced dialysis processes and are apt in diagnosing and treating wide range of infectious, inflammatory, metabolic, obstructive and hereditary diseases related to kidneys, including Chronic Kidney Disease (CKD), End-Stage Renal Disease (ESRD), Polycystic Kidney Disease (PKD), Acute Kidney Injury (AKI), Diabetic Nephropathy, Acute Glomerulonephritis, Kidney Stones (Nephrolithiasis), Hydronephrosis, Hematuria, Proteinuria, Lupus Nephritis, Medullary Sponge Kidney, Renal Artery Stenosis etc.
Why Choose PACE Hospitals for Nephrology Treatments?
Comprehensive
Kidney Care
Providing treatment to a wide range of acute and chronic disorders related to kidney with high precision and lesser recovery time.
Advanced State-of-the-art Facility
Equipped with advanced and cutting edge diagnostic equipment to cater effective and precise treatment to all kind of acute and chronic kidney disorders.
Skilled & Experienced Nephrology Doctors
Team of experienced kidney disease doctor with vast experience in diagnosing and managing all kind of critical & complex kidney disorders.
Advanced Centre for Acute & Chronic Kidney Disease Treatments in Hyderabad, Telangana

PACE Hospitals is one of the best kidney specialist hospitals in Hyderabad. The department is staffed with a team of skilled and experienced kidney disease specialists expertise in handling a wide range of acute and chronic kidney diseases; they are apt with the latest diagnostic and treatment modalities to tackle any kidney-related disease from its early stage management to complex treatments like dialysis and kidney transplants.
The Department of Nephrology at PACE Hospitals is equipped with cutting-edge state-of-the-art Imaging diagnostic facilities and laboratory tests, including CT scans, MRI, ultrasound-guided imaging, kidney function test, and urinalysis to precisely evaluate the conditions and start with the appropriate treatment plans. The treatment plans designed by the skilled nephrology doctors are compassionate, personalized and precise to manage complex and critical chronic and acute kidney disorders and diseases like Polycystic Kidney Disease (PKD), Glomerulonephritis, Hydronephrosis, Kidney stone, Diabetic Nephropathy, kidney failure and more.
3,12,338
98,538
684
2011
Top Nephrology Doctors in Hyderabad | Kidney Specialist
A team of the best nephrology doctors in Hyderabad, India, are highly skilled and experienced in the management of a wide array of acute & chronic kidney diseases and infectious, genetic and autoimmune renal disorders. They have extensive expertise in the treatment of complex and critical kidney disorders like chronic kidney disease (CKD), acute kidney injury, kidney stones, nephrotic syndrome, glomerulonephritis, hypertension-induced kidney damage, and diabetic nephropathy. They are apt with advanced diagnostic tools and interventional treatment like kidney function tests (KFT), imaging tests, urinalysis, doppler studies, renal biopsies, dialysis, CRRT and kidney transplant preparations.
Dr. A Kishore Kumar
MD (Medicine) (JIPMER), DM (Nephrology) (AIIMS, New Delhi)
Experience : 11+ years
Consultant Nephrologist and Renal Transplant Physician
Consultation Timing:
Mon to Sat - 9 am to 6 pm
Location:
PACE Hospitals, HITEC City
Nephrology Conditions Explained by Drs
Need Help?
Are you struggling with symptoms like swelling in your legs, puffiness around the eyes, changes in urination, blood in the urine or unexplained back pain? It could be kidney-related disease and disorders like kidney infections, stones in the kidney or more complex kidney diseases like glomerulonephritis, Chronic Kidney Disease (CKD), Diabetic Nephropathy, Hypertensive Nephropathy, Polycystic Kidney Disease (PKD), Nephrotic Syndrome, Chronic Pyelonephritis. To avoid further complications and damage to kidney functioning, we offer comprehensive diagnostic examinations to cater to personalized and effective treatment plans to regain control of your kidney health.
What we treat?
We specialize in the treatment of the broad spectrum of kidney diseases, including kidney infections, kidney stones, Electrolyte imbalances, Glomerular disorders, autoimmune kidney disorders like IgA Nephropathy, Membranous Nephropathy, Lupus Nephritis, Focal Segmental Glomerulosclerosis (FSGS) to genetic kidney diseases like Polycystic Kidney Disease (PKD), Alport Syndrome, Bartter Syndrome, Nephronophthisis (NPH), Primary Hyperoxaluria, Tuberous Sclerosis Complex (TSC), Congenital Nephrotic Syndrome, Medullary Cystic Kidney Disease (MCKD), Sickle Cell Nephropathy.
From acute kidney diseases like Acute Kidney Injury (AKI), Acute Glomerulonephritis, Acute Interstitial Nephritis (AIN), Acute Pyelonephritis, Postrenal Acute Kidney Injury, Hemolytic Uremic Syndrome (HUS), Renal Vascular Disorders to complex chronic kidney diseases like Chronic Kidney Disease (CKD), Diabetic Nephropathy, Hypertensive Nephropathy, Polycystic Kidney Disease (PKD), Nephrotic Syndrome, Chronic Pyelonephritis, Obstructive Nephropathy, End-Stage Renal Disease (ESRD), our team of nephrology doctors and specialist for kidneys is committed to delivering effective, precise and compassionate treatments with minimal recovery time.
Acute Kidney Failure
It's also known as acute kidney injury, characterised by elevated serum creatinine (1.5 times more than baseline value before 7 days or 0.3 mg/dL or more within 48 hours as per KDIGO) and decreased urine output (<0.5mL/kg/hour for at least 6 hours as per KDIGO).
This condition is often reversible and is measured with the help of the global filtration rate (GFR). Acute renal failure can lead to water, sodium, and other metabolic product accumulation in addition to electrolyte imbalances. It is caused by acute tubular necrosis, interstitial nephritis, severe dehydration, acute nephrotic syndrome, urinary tract obstruction and reduced blood flow to the kidneys.
Acquired Cystic Kidney Disease
Acquired cystic kidney disease is a medical condition in which the kidneys develop cysts (fluid-filled sacks), different from polycystic kidney disease.
This condition can occur in children and adults suffering from chronic kidney disease or end-stage renal failure. The exact aetiology of this condition is idiopathic (unknown); however, the cyst mostly develops in people who are on dialysis (kidney failure). This condition is often asymptomatic; nevertheless, the complications of acquired cystic kidney disease show signs and symptoms such as fever, back pain, and haematuria (blood in urine).
Aneamia of kidney Disease
Anaemia of Chronic Kidney Disease is a common complication that occurs due to the kidneys' reduced ability to produce erythropoietin. The hormone that stimulates the production of RBC.
Chronic kidney disease leads to a shortage of erythropoietin, causing a low red blood cell count (anaemia). This can lead to paleness, weakness, fatigue, and shortness of breath. Anaemia in CKD is worsened by factors like iron deficiency, inflammation, and the effects of dialysis. Treatment typically involves erythropoiesis-stimulating agents (ESAs), iron supplementation, and sometimes blood transfusions to improve red blood cell production, address iron deficiency, and manage the underlying kidney disease. Proper management of anaemia in CKD helps improve quality of life and reduce complications such as cardiovascular disease.
Acute Kidney Injury (AKI)
Acute kidney damage is characterized by a rapid loss in renal function over days to weeks, resulting in the accumulation of nitrogenous products in the blood (azotemia) and no drop in urine production.
It is mainly caused by insufficient renal perfusion as a result of severe trauma, illness, or surgery, but it can also be caused by a rapidly progressive, intrinsic renal disease. Symptoms may include anorexia, nausea, and vomiting. If neglected, it can lead to seizures and coma. Fluid, electrolyte, and acid-base problems develop rapidly. Treatment focuses on the underlying cause but may also require hydration, electrolyte control, and dialysis.
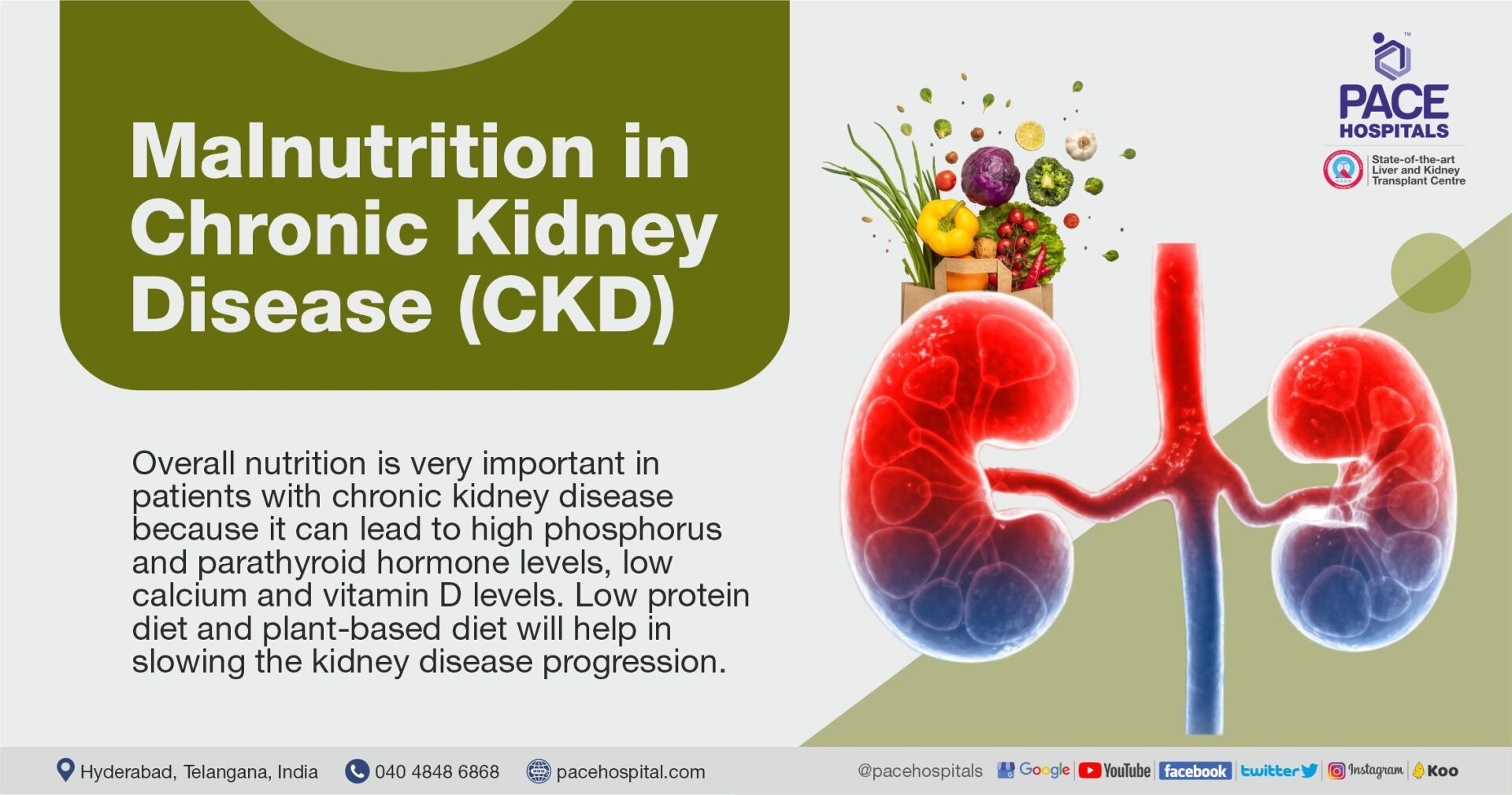
Chronic Kidney Disease
Chronic kidney disease, or CKD, is a disorder in which the kidneys gradually lose the ability to function normally over time. In the early stages, symptoms might not be noticeable, but as the disease progresses, people may experience problems like loss of appetite (anorexia), nausea, vomiting, mouth sores, bad taste, frequent urination at night (nocturia), fatigue, itching, muscle cramps, fluid buildup, poor nutrition, and nerve issues.
In severe cases, it can affect mental clarity and lead to seizures. Treatment focuses on managing the causes, including fluid and electrolyte management, blood pressure control, anaemia treatment, several types of dialysis, and kidney transplantation.
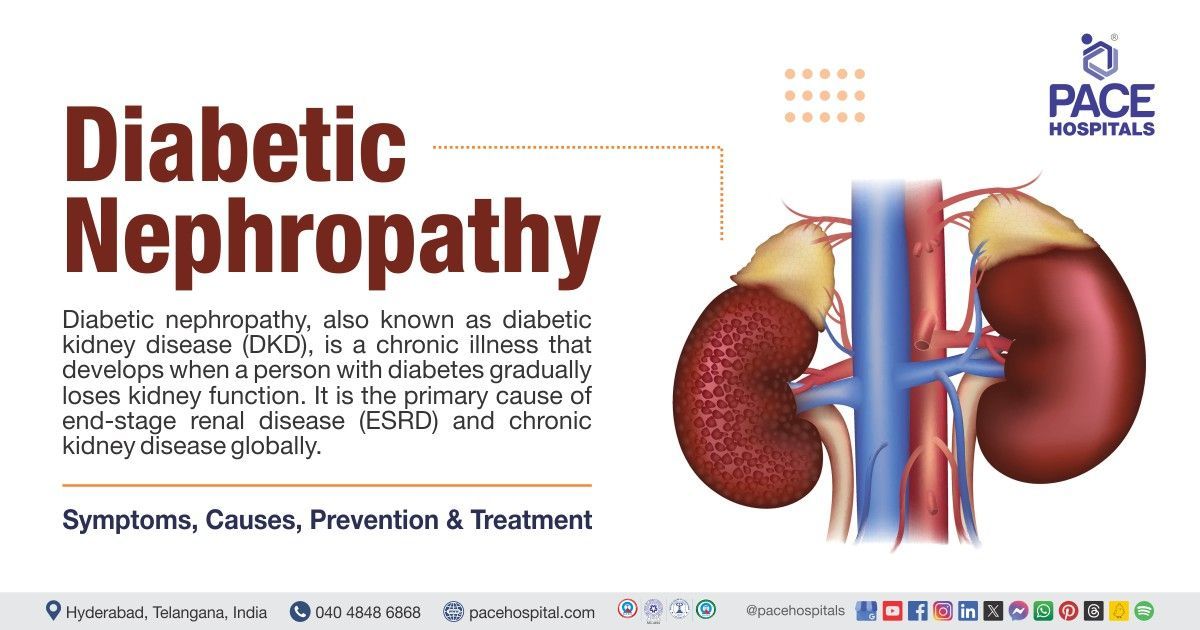
Diabetic Kidney Disease
It is a long-term kidney disease that affects people with diabetes. It occurs due to prolonged increased levels of glucose in the blood and damages the renal blood vessels because of insulin resistance or low/no insulin production. Smoking, age above 65 years, women's gender, obesity, increased blood pressure, and hyperlipidaemia are the risk factors for diabetic nephropathy.
Changes in blood pressure, shortness of breath, fatigue, vomiting, metallic taste, blood in urine, swollen legs, hands and feet are the symptoms of diabetic nephropathy.
Ectopic Kidney
An ectopic kidney is a condition where the kidney is not located in its usual position or present on the opposite side above or below the kidney's normal position. The two kidneys are usually positioned just below the rib cage (on either side of the spinal cord), near the middle of the back.
The exact cause of this condition is idiopathic; however, researchers estimate that an ectopic kidney may result from a weakly developed kidney bud, the presence of a genetic disorder, a problem in the kidney tissue, and the presence of any disease or infection during foetal growth.
An ectopic kidney is usually asymptomatic (doesn't cause any symptoms or health problems), and it is usually found during a foetal ultrasound or during regular screening tests done to check for urinary tract infection (UTI) or to find the cause of abdominal pain.
End-stage Renal Disease
End-stage renal disease (ESRD), also known as end-stage renal failure, is the last irreversible stage of chronic kidney disease. It occurs when kidney function has decreased to the point where the kidneys can no longer function independently.
Dialysis or a kidney transplant are the only ways an end-stage renal failure patient can live more than a few weeks.
Patients with ESRD might experience various symptoms that include drowsiness, difficulty urinating, skin itchiness, headache, nausea, bone pain, loss of weight, dry skin, etc. It can be diagnosed by urine tests, renal ultrasound, kidney biopsy, CT scan, and blood tests. Hypertension, diabetes, heart problems, and drug abuse are some of the risk factors for End Stage Renal Disease.
Focal Segmental Glomerulosclerosis
Focal segmental glomerulosclerosis is a rare disease that results in scarring of the glomerulus (the kidneys' filtering unit). It is caused by certain drugs, infection, obesity, inherited genetic problems, and sickle cell disease.
This disease affects both adults and children but more common in men, it is characterized by symptoms of edema, proteinuria (protein in blood), weight gain and poor appetite. Managed by drugs that lowers high blood pressure, agents that get rid of excess body fluids and diet with low salt intake. If not treated properly this condition may lead to some complications such as nephrotic syndrome, infection, malnutrition, chronic kidney disease and end stage kidney disease.
Glomerulonephritis
Glomerulonephritis is a condition characterised by the inflammation and scarring of the glomerulus. The kidneys' capacity to filter waste products and extra fluid from the blood to produce urine gradually declines. Medicines (toxins), viral infections (HIV, hepatitis B& C), Lupus-related kidney inflammation, IgA nephropathy, and bacterial (strep or staph bacteria) infections are the causative factors for glomerulonephritis.
An increase in blood pressure, fatigue, protein in urine, blood in urine, and low urine output are the symptoms of glomerulonephritis. This condition can be diagnosed by blood tests, kidney ultrasound, kidney biopsy and urinalysis.
Glomerulosclerosis
Glomerulosclerosis is the scarring of tiny kidney blood vessels (glomeruli). It may develop in children and adults and can result from different types of kidney problems and diabetes. Protein in urine, swelling of ankles, puffy eyes, and fluid accumulation in the abdomen are the symptoms of this condition. Nearly 7 to 15% of people with proteinuria have glomerulosclerosis.
Glomerular Disease
Glomerular disease is a condition that can affect the kidneys. This condition damages tiny kidney filters known as glomeruli, which purify the blood. Due to glomerular damage, Proteins and, in certain cases, red blood cells can leak into urine. Albumin is a type of protein found in the blood. If too much albumin passes into the urine, fluid can accumulate in the body, causing edema in the face, hands, feet, or legs. In some situations, glomerular disease may stop the kidneys from effectively eliminating waste products, causing wastes to accumulate in the blood.
Slow progression of this disease causes serious complications such as hypertension, chronic renal disease, nephrotic syndrome and kidney failure; in some cases, it causes rapid kidney failure, which leads to confusion and death if not treated immediately. It affects men and women of all ages, and having a family member who has glomerular disease increases the risk. Health care providers treat glomeruli with medications including angiotensin II receptor blockers (ARB)., statins, diuretics (water pills) and drugs that make the immune system less active, such as corticosteroids, antimetabolite agents or monoclonal antibodies.
Horseshoe kidney
A Horseshoe kidney, also known as renal fusion, is where two kidneys are fused together and form a horseshoe-shaped kidney that might be located at different positions compared to typical kidneys. In general, during the stage of foetal development, the kidney first forms in the lower belly and moves up toward the back of the pelvic area. In the case of the horseshoe kidney, the kidneys attached to the lower end fuse and form a "U shape".
Horseshoe kidney affects about one in every 500 people (especially in men) and are asymptomatic. The exact causes of horseshoe kidney disease are idiopathic (unknown); however, it could be related to the genes that form the kidneys and exposure to environmental factors and toxins before birth.
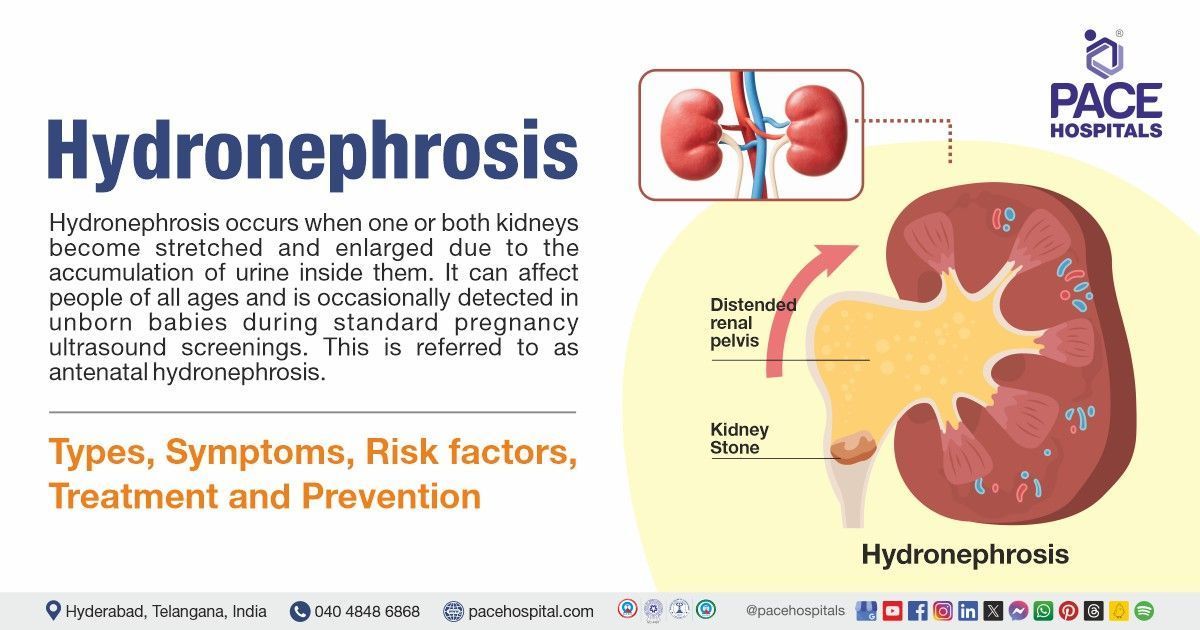
Hydronephrosis
Hydronephrosis is defined as kidney swelling that occurs due to urine backup or backflow. It is caused by bladder blockage, birth defects of the urinary system, kidney stones, and cancer or tumours that develop in the ureter, bladder, or pelvic region.
It can occur in one or both kidneys, when it occurs in both kidneys it is termed bilateral hydronephrosis. It is characterized by symptoms of flank pain, nausea, vomiting, fever, painful urination, urinary urgency and increased urinary frequency. Hydronephrosis is managed by removing kidney stones, antibiotics to treat infection and with placement of stent through bladder and ureter to allow passage of urine from kidneys to bladder. The affected kidney gets damaged permanently if it is left untreated.
Hematuria
Hematuria indicates the presence of blood in urine. It is classified into gross hematuria, which can see blood in urine, and microscopic hematuria, which cannot see blood in urine but can be observed under a microscope or by a urine test known as a urinalysis. Gross hematuria is less prevalent than microscopic hematuria. Gross hematuria changes urine colour to pink, red, or brown. It does not produce discomfort or other symptoms, although it may induce bladder or back pain if blood clots are in the urine.
Microscopic hematuria, on the other hand, does not change the colour of the urine and usually does not cause symptoms. This is caused by infection or inflammation of the bladder, urinary tract stones or a recent urinary tract procedure, BPH (Benign prostatic hyperplasia), prostate, kidney and urethra trauma, prolonged sexual activity, and endometriosis Health care practitioners treat hematuria by addressing its underlying cause.
Hypertensive Nephropathy
Hypertensive nephropathy (HTN) or hypertensive nephrosclerosis is a kidney disease caused by chronic high blood pressure and is the second most common cause of end-stage renal disease (ESRD). Symptoms include nausea, vomiting, loss of appetite, itching, sleepiness, weight loss, and an unpleasant taste in the mouth.
Risk factors include older age, poorly controlled high blood pressure, and other kidney disorders, including diabetic nephropathy. Treatment focuses on strict blood pressure control with a combination of drugs, including an angiotensin II receptor blocker (ARB), an angiotensin-converting enzyme (ACE) inhibitor, calcium channel blockers, thiazide diuretics and beta-blockers. Lifestyle changes like weight loss, exercise, and salt and water restriction also help control blood pressure and sometimes dialysis.
IgA Nephropathy
Immunoglobulin A (IgA) nephropathy is an autoimmune disease that causes inflammation and damage to the kidneys by accumulating or depositing clumps of antibodies.
It is more common in men and individuals with a family history of IgA vasculitis, characterized by symptoms of hematuria (blood in urine), proteinuria (protein in urine), swelling of legs, ankles and other parts of the body due to accumulation of body fluids. It can be managed with angiotensin-converting enzyme (ACE) inhibitor or with angiotensin receptor blocker (ARB) to treat high blood pressure and with certain dietary modifications by limiting sodium intake. If left untreated this autoimmune disease may result in complications such as nephrotic syndrome, chronic kidney disease and kidney failure.
Interstitial Nephritis
Interstitial nephritis is a kidney disorder which decreases the ability of kidneys to filter the blood, affecting older individuals, it is caused by allergic reactions to drugs, autoimmune disorders such as Kawasaki disease, excess calcium and low potassium in the blood. It is characterized by symptoms of fever, increased or decreased urination, nausea, vomiting and hematuria (blood in urine). These symptoms can be managed by avoiding the causative drug and by maintaining a balanced diet with low salt intake.
If it is not treated this condition may cause complications such as metabolic acidosis, chronic kidney disease and end stage kidney disease. Describe the item or answer the question so that site visitors who are interested get more information. You can emphasize this text with bullets, italics or bold, and add links.
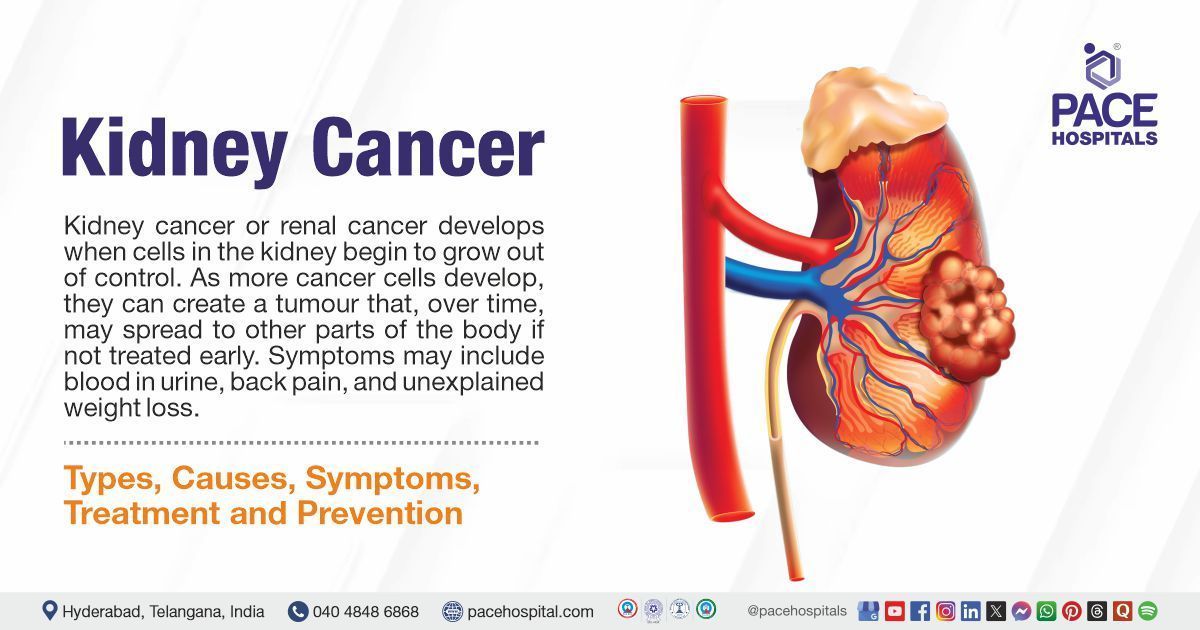
Kidney cancer
Kidney cancer develops when the cells in the kidneys grow out of control, resulting in an increase in blood pressure, urine in blood, flank pain, tiredness, loss of hunger, loss of body weight, fever (low grade), bone pain, anaemia, and lump or mass in the kidney. Smoking, Obesity, hypertension, radiation therapy, family history, gene mutations, dialysis treatment, and the presence of tuberous sclerosis complex and Von Hippel-Lindau disease are the primary causes of kidney cancer.
Urinalysis, blood tests, CT scans, Magnetic resonance imaging, ultrasound and renal mass biopsy can diagnose it.
Kidney stones (Nephrolithiasis)
Kidney stones are strong, hard objects composed of chemicals in urine. Calcium oxalate, struvite, uric acid and cystine are the four types of kidney stones. The common symptoms include pain, blood in urine, nausea, vomiting, fever and chills.
The most common causes (etiology) of kidney stones are drinking less water than the daily requirement, low exercise, weight loss surgery, obesity, consuming food with too much salt or sugar, family history, and infections. In addition to these, consuming excess fructose can increase the risk of kidney stones. This can be disguised by a CT scan and KUB x-ray.
Kidney Failure
It is the condition where the kidneys no longer function on their own, resulting in itchy skin, loss of hunger, hand-face or ankle swelling, nausea, vomiting, difficulty concentrating, muscle cramps, and fatigue.
The most common causes of kidney failure are unmanaged high blood sugar levels and high blood pressure (hypertension). People with diabetes, abnormal kidney structure, high blood pressure, heart disease, a family history of kidney disease, age over 60, and intake of pain relievers are at high risk of developing kidney failure and chronic kidney disease (CKD). Polycystic kidney disease, Lupus and Glomerular diseases are the major causes of CKD leading to kidney failure.
Kidney Abscess
A kidney abscess is a pus formation in a hollow area of the kidney. Patients with renal abscesses might have symptoms that include an increase in body temperature(fever), chills, pain in the abdomen, loss of body weight, pain while passing urine, and blood in urine.
Kidney abscesses can be caused by bacteria that spread to the kidney from the blood or from urine that backs up into the kidney, thereby spreading the infection. Kidney abscesses can also occur because of kidney stone disease, kidney inflammation, and urine backward flow from the bladder into the kidney. Complicated urinary tract infections such as pregnancy, diabetes mellitus, and neurogenic bladder can increase the risk of kidney abscess.
Lupus Nephritis
Lupus nephritis is kidney inflammation caused by systemic lupus erythematosus; this disease is more common in women than men. It is characterized by symptoms of swelling of hands and feet (due to excess body fluid), weight gain or loss, fatigue, foamy urine due to protein, and high blood pressure.
It can be managed with immunosuppressants and with the use of diuretics (that treat edema), calcium channel blockers and beta blockers (to treat high blood pressure). If it is not treated it may lead to complications such as diffuse proliferative nephritis and kidney failure.
Medullary Sponge Kidney
Medullary sponge disease or Cacchi–Ricchi disease is a birth defect that results in changes in tubules and tiny tubes of a fetus's kidney. The cause of this disease is unknown, and it occurs more often in women than men in individuals with a risk of calcium-based kidney stones. It is characterized by symptoms of painful or burning urination, cloudy or dark-coloured urine, fever, and smelling urine.
This condition is not reversable, and treatment usually focuses on managing existing urinary tract infection and removing kidney stones. Complications like hematuria (blood in urine) and kidney stones occur when it is left untreated.
Nephrotic syndrome
Nephrotic syndrome is a renal disorder where the kidney excretes an excessive amount of protein in the urine. The destruction of the small renal (kidney) blood vessels that aids in removing waste and extra water from the blood, resulting in nephrotic syndrome. In addition to increasing the risk of other health issues, the disorder produces swelling, especially around the eyes, ankles and feet, loss of hunger, fatigue, weight gain due to fluid retention, and foamy urine (due to excess protein in the urine).
Diabetic kidney disease (diabetic nephropathy), minimal change disease, amyloidosis, focal segmental glomerulosclerosis, membranous nephropathy, and systemic lupus erythematosus are the primary possible causes of nephrotic syndrome.
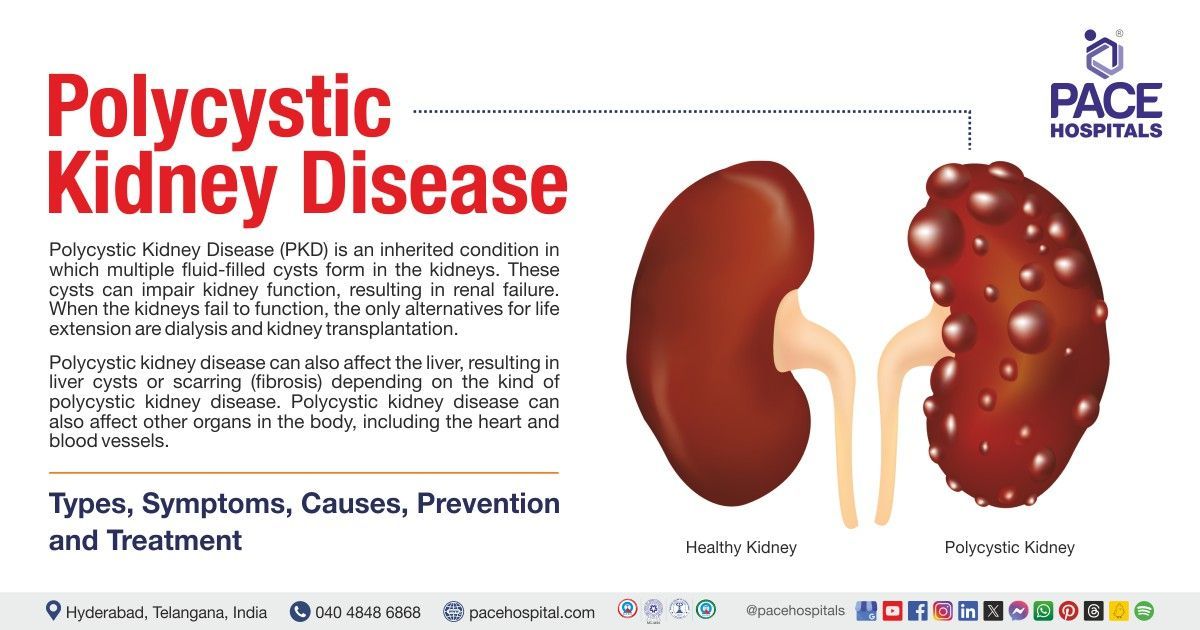
Polycystic Kidney Disease
Polycystic kidney disease (PKD) is a genetic condition that results in the growth of many fluid-filled cysts in the kidneys. In contrast to ordinary kidney cysts, PKD cysts can change the shape of the kidneys, resulting in an increase in their size. Kidney failure may result from PKD, a type of chronic kidney disease (CKD) that impairs kidney function.
Autosomal dominant PKD and autosomal recessive PKD are the two types of polycystic kidney disease. An increase in blood pressure, chest pain, backside pain, blood in urine, and an increase in abdominal size are the symptoms of PKD.
Proteinuria
Proteinuria, also known as albuminuria, is a condition in which urine contains an abnormally high protein called albumin, the main protein in the bloodstream. In the early stage, Proteinuria has no signs or symptoms, but high protein levels in urine may cause it to appear frothy in the toilet. This leads to no longer absorbing enough fluid, resulting in swelling in the hands, feet, abdomen, or face.
These signs of large protein loss indicate that kidney disease has progressed. People with diabetes, hypertension, or certain family history are at risk for Proteinuria. Treatment mainly involves angiotensin-converting enzyme (ACE), angiotensin receptor blockers (ARBs), and diuretics, and it follows a healthy diet plan.
Renal Tubular Acidosis
Renal tubular acidosis is a condition which occurs when the kidneys are not able to remove or excrete acids from blood into the urine. It is of three types: type 1 (distal renal tubular acidosis) is caused by an autoimmune disease known as Sjogren’s syndrome, type 2 (proximal renal tubular acidosis) is caused by Fanconi syndrome or caused by drugs to treat viral hepatitis, type 4 (hyperkalemic renal tubular acidosis) is caused due to rejection of kidney transplantation.
It is characterized by symptoms of weakness, paralysis, irregular heartbeat, abdominal pain; can be treated by oral intake of alkali solution (solution that contains sodium carbonate or sodium citrate) that decreases the acid levels. Untreated type 1 and type 2 renal tubular acidosis causes complications like slow growth of children and rickets (bone disease). Type 4 renal tubular acidosis when left untreated causes muscle weakness and cardiac problems like irregular heartbeat and cardiac arrest.
Renal Artery Stenosis
Renal artery stenosis, also known as renal artery disease, is a narrowing or constricting of renal (kidney) arteries which carry oxygenated blood from the heart to the kidneys. People with atherosclerosis (plaque or obstruction that builds up due to fat accumulation on artery walls) are at high risk of renal artery stenosis.
In addition, high blood pressure, high cholesterol, obesity, diabetes, family history of cardiovascular disease, smoking, poor diet and older age are at-risk factors for renal artery stenosis. Difficulty in sleeping, fatigue, loss of hunger, muscle cramps, oedema, shortness of breath, dry/itchy skin, sudden weight loss, abnormal urination, headache, nausea and vomiting are the symptoms of renal artery stenosis.
Patient Testimonials
Common Nephrology Diagnosis & Procedures
The Nephrology Department at PACE Hospitals is committed to catering excellent diagnostic services focused on delivering an accurate and comprehensive range of diagnostic evaluations to examine and treat various acute and chronic kidney diseases. The team of experienced and skilled nephrology doctors uses extensive diagnostic tests, including kidney function tests, urinalysis, ultrasound, and renal biopsies, aiming at early diagnosis and thorough evaluations of the issues to address them with appropriate treatment modalities.
They are also experienced with state-of-the-art life-saving interventional procedures like hemodialysis, peritoneal dialysis, CRRT and kidney transplant preparation to ensure precise and effective kidney disease treatment with a high success rate and quicker recovery.

- Kidney Function Tests: A kidney Function Test (KFT) is a blood test done to examine and evaluate the functioning of the kidney in terms of how efficiently it is filtering the waste and maintaining the fluid and electrolyte balance. This test helps diagnose and evaluate critical kidney conditions like chronic kidney disease, acute kidney injury, and renal failure. Common tests included in Kidney function Tests are:
- Glomerular Filtration Rate (GFR): It is the rate at which the substance in plasma is filtered out through the glomerulus in a minute. The normal GFR in adults is 90 to 120 mL per minute. The values for GFR as per the stages are as follows.
- Stage 1 GFR > 90 ml/min/1.73 m²
- Stage 2 GFR ≥ 60 and ≤89 ml/min/1.73 m²
- Stage 3a GFR ≥ 45 and ≤59 ml/min/1.73 m²
- Stage 3b GFR ≥ 30 and ≤44 ml/min/1.73 m²
- Stage 4 GFR ≥ 15 and ≤29 ml/min/1.73 m²
- Stage 5 GFR (end-stage renal disease) <15 ml/min/1.73 m²
- Creatinine: Creatinine is a waste product that develops from the digestion of protein intake from the diet and muscle tissue breakdown. It is removed from the blood through the kidney. An increase in creatinine concentration can be a sign of kidney disease. It is the endogenous marker for the assessment of GFR that involves the collection of urine over a 24-hour period or for 5 to 8 hours. It is calculated by using the formula. C = (U x V) / P.
- Blood Urea Nitrogen (BUN): It is an end product of protein metabolism and the urea cycle. It's mostly formed in the liver. Nearly 85% of the urea is eliminated through the kidneys. Any abnormality in the kidney function results in an increase in serum urea levels.
- BUN (Creatinine Ratio): This test is used to differentiate prerenal from renal causes based on increased blood nitrogen levels. The ratio is close to 20:1 in the case of prerenal disease (poor blood perfusion to nephrons, leading to a decrease in GFR) and 10:1 if it is an intrinsic renal disease (conditions that affect glomerulus or tubule). Upper gastrointestinal bleeding can be associated with a high BUN to creatinine ratio (>30:1).
- Cystatin C: It is a low molecular weight protein that functions as a protease inhibitor, which is produced by the body's nucleated cells, formed at a constant rate and filtered out by the kidneys. Serum cystatin C levels will be increased with decrease in GFR rate. Cystatin C was measured both in urine and serum samples.
- Albuminuria: Albuminuria is defined as the abnormal presence of albumin in the urine. It is the independent marker for cardiovascular disease and incipient nephropathy in diabetics, in addition to being a marker for chronic renal impairment. It may be measured in a 24-hour urine sample or early morning sample. The presence of albumin in the urine on both occasions (early morning and 24 hours) with an exclusion of urinary tract infection can indicate the presence of kidney dysfunction. The presence of albuminuria for more than three months indicates chronic kidney disease.
2. Urinalysis: It is a test that examines the visual, chemical, and microscopic aspects of urine and detects various compounds passing through the kidneys.
- Visual: The healthcare provider examines the colour (pale, dark yellow, etc.) and appearance (cloudy or clear) of urine through the naked eye.
- Chemical: It can be analysed with the help of strips known as a dipstick, which consists of chemical pads that change colour when in contact with a urine sample. The degree of colour change in the dipstick estimates the presence of chemical substances in the urine. A light colour represents the trace or small amounts of substance in the provided urine sample, while a deep colour represents large amounts. The dipstick test detects proteins, ketones, glucose, bilirubin, nitrites, and leukocyte esterase concentrations in the urine in addition to urine pH and specific gravity.
- Microscopic: This test is used to examine the presence of substances such as mucus, urinary casts, cells and their fragments, bacteria, yeast, parasites, and crystals. In addition, the presence of red blood cells(RBC), white blood cells (WBC), epithelial cells, and urinary casts can also be detected in the urine sample.
3. Kidney Ultrasound: It is a non-invasive diagnostic exam that visualizes the blood flow, shape, size and location of the kidneys. The urologist will be placing an ultrasound transducer on the skin that emits high-frequency ultrasound waves that move through the kidney. These ultrasound waves produce images of the kidney that are presented to the computer. This test is used to diagnose the presence of cysts, obstructions, abscesses, stones and infections of the kidney. In addition, it is indicated after a kidney transplant to evaluate the transplanted kidney.
4. Kidney CT- Scan: It is also known as renal scintigraphy, where the kidneys can be visualized with the help of nuclear radioactive material (radioisotope) that will be inserted into the vein (hand or arm). The images of the kidney can be created when the scanner detects the gamma rays released from the radioisotope. This test can be used to examine the size, shape and structure of the kidney. In addition, it is used to identify and evaluate the reduced flow of blood to the kidneys, high blood pressure in real arteries, kidney diseases, success or rejection of kidney transplant, renal abscesses, tumours, kidney inflammation due to infections, urine backflow from the bladder to the kidney and kidney failure.
5. Kidney Biopsy: A kidney biopsy is a diagnostic procedure that involves taking a small piece or sample of kidney tissue in order to view it under a microscope for indications of kidney damage or injury. In addition to this, kidney biopsy is indicated in the development of treatment plans based on the patient's condition to determine the kidney disease progression, extent of kidney damage, evaluation of prescribed treatment for kidney disease, and monitoring of transplanted kidney, which is failed to perform normal functions.
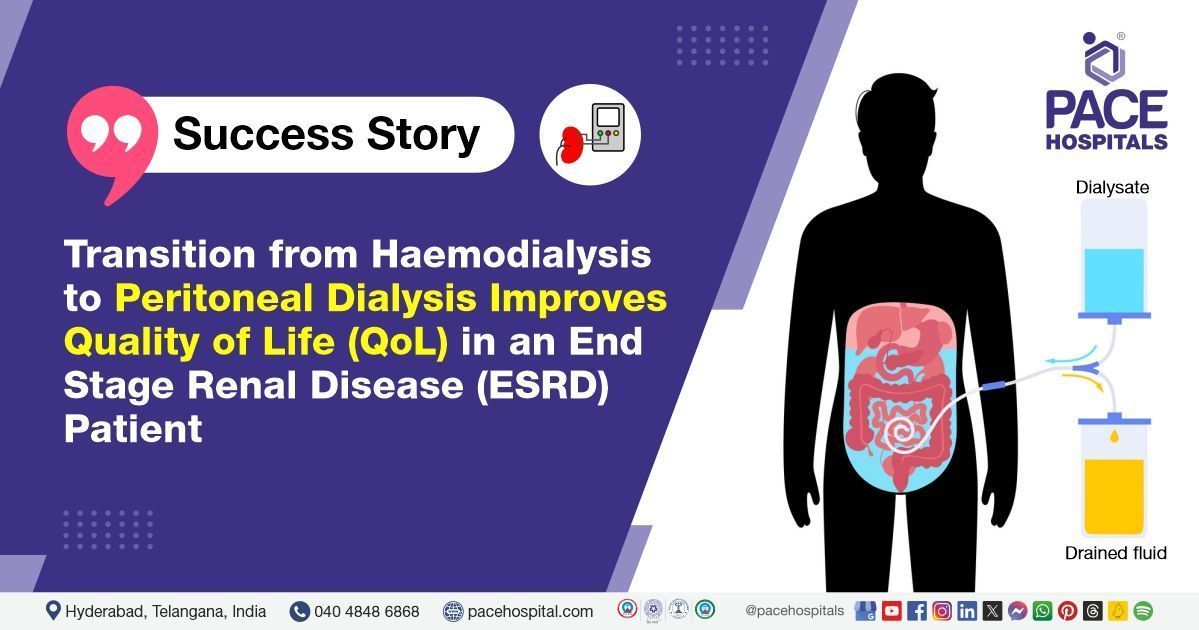
6. Dialysis: Dialysis is a medical procedure that helps in filtering blood when the kidneys are not functioning. It removes waste products, excess fluids and toxins from the blood, which otherwise can accumulate and lead to some serious health problems. It is primarily of two types: hemodialysis and peritoneal dialysis. It is an effective treatment option, and it is indicated in two different situations; one is acute kidney injury, and the other is kidney failure.
- Hemodialysis: Hemodialysis is the most common type of dialysis, in which the blood is filtered through a filtering machine. This procedure involves a dialyzer that removes extra fluids and waste from blood. Before carrying out dialysis, a minor surgical procedure called AV fistula (connection between an artery and vein) is required to provide a vascular access site, usually in the arm, to allow withdrawal and return of blood. Blood from one end of the filter passes through thin hollow fibers, dialysis solution passes on the outside of the fiber collecting waste from the blood. The filtered blood remains in the fiber and is returned to the body. The entire process lasts for about four hours and is conducted three times a week at home or at the dialysis centre.
- Peritoneal dialysis: Peritoneal dialysis is the process of filtering the blood inside the body using the belly area or lining of the abdomen (peritoneum) as a filter. Before this procedure, a minor surgery is required to insert a catheter into the belly. Through the catheter the belly is filled with a dialysate which is a cleansing solution made from a mixture of water and salt. Dialysate extracts extra fluids and waste products from the blood vessels into the belly area as the blood flood flows through the area. Using the same catheter, the fluid mixture is drained out in the bag used in the treatment. It is commonly of two types: continuous ambulatory peritoneal dialysis (CAPD) and automated peritoneal dialysis (APD).
7. Continuous Renal Replacement Therapy (CRRT): Continuous renal replacement therapy (CRRT) is a dialysis technique used in intensive care unit for critically ill patients with acute kidney injury (AKI) and to patients who are hemodynamically unstable. The initiation of this therapy is indicated in volume overload, metabolic acidosis, electrolyte abnormalities and progressive acute kidney injury situations. It is a continuous and slow-motion therapy which runs for 24 hours. A large intravenous catheter is placed into a vein, either into their neck or groin. It is a temporary procedure and is carried out up to the point that the patient can tolerate standard dialysis.
8.
Kidney Transplant: It is a surgical procedure that is used to replace a healthy kidney from a donor with a diseased or damaged kidney. The healthy kidney can come from a living donor (family members or other suitable candidates to donate one of their kidneys) or from a deceased (dead) organ donor. Infection, Urine leakage, blockage of renal blood vessels, bleeding, and infections are the risks associated with this procedure. In some cases, a rejection of transplanted kidneys can occur.
Health and Diseases Information
Why choose PACE Hospitals?
- A Multi-Super Speciality Hospital.
- NABH, NABL, NBE & NABH - Nursing Excellence accreditation.
- State-of-the-art Liver and Kidney transplant centre.
- Empanelled with all TPA’s for smooth cashless benefits.
- Centralized HIMS (Hospital Information System).
- Computerized health records available via website.
- Minimum waiting time for Inpatient and Outpatient.
- Round-the-clock guidance from highly qualified nephrology and urology doctors.
- Standardization of ethical medical care.
- 24X7 Outpatient & Inpatient Pharmacy Services.
- State-of-the-art operation theaters.
- Intensive Care Units (Surgical and Medical) with ISO-9001 accreditation.