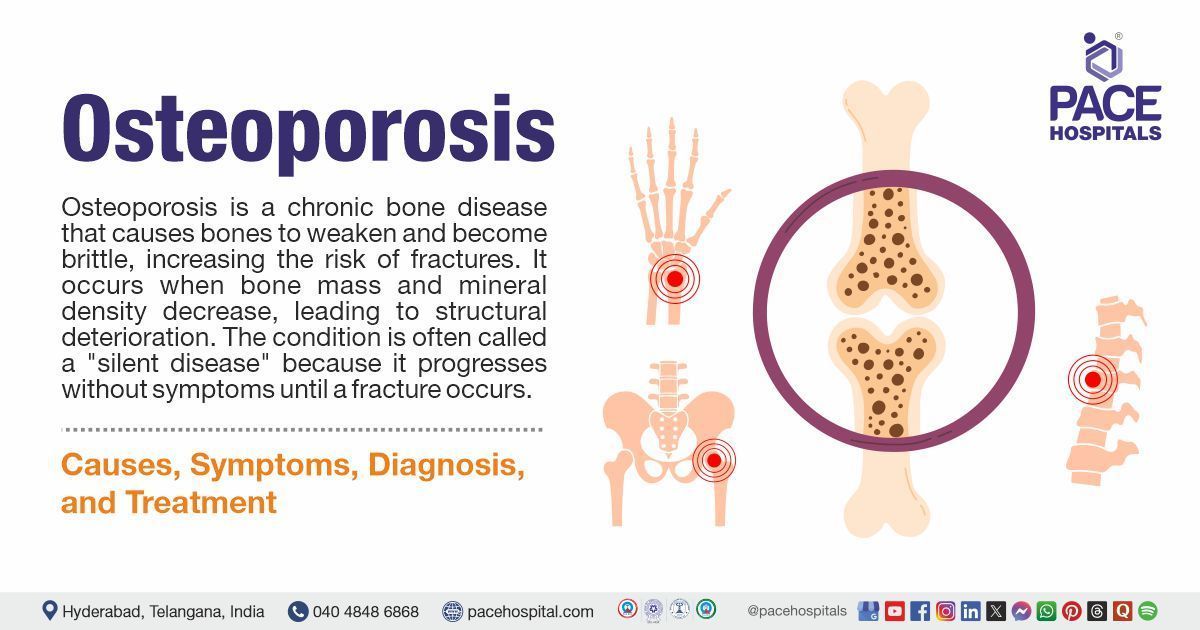
Osteoporosis: Causes, Symptoms, Diagnosis, Treatment & Prevention
PACE Hospitals
What is Osteoporosis?
Osteoporosis is a chronic bone disease that causes bones to weaken and become brittle, increasing the risk of fractures. It occurs when bone mass and mineral density decrease, leading to structural deterioration. The condition is often called a "silent disease" because it progresses without symptoms until a fracture occurs.
How Osteoporosis Affects the Body?
Healthy bones constantly undergo a process of renewal, where old bone is broken down and new bone is formed. With osteoporosis, bone loss occurs faster than bone formation, making bones weak and fragile. The most commonly affected areas include:
- Spine (Vertebrae): Compression fractures can cause severe back pain and height loss.
- Hips: Hip fractures often require surgery and can lead to long-term disability.
- Wrists: A simple fall can cause a wrist fracture, affecting daily activities.
- Ribs: Rib fractures can lead to pain and breathing difficulties.
Causes & Risk Factors of Osteoporosis
Osteoporosis develops due to a combination of genetic, lifestyle, and medical factors that influence bone density.
1. Genetic Factors
- Family history of osteoporosis increases the risk.
- People with smaller body frames or lower bone mass are more susceptible.
2. Hormonal Changes
- Menopause: Estrogen plays a crucial role in bone maintenance, and its decline in postmenopausal women accelerates bone loss.
- Testosterone Deficiency: In men, low testosterone levels can lead to decreased bone density.
- Thyroid Disorders: Overactive thyroid (hyperthyroidism) increases bone loss.
3. Lifestyle & Dietary Factors
- Poor Nutrition: Inadequate calcium, vitamin D, and protein intake weakens bones.
- Sedentary Lifestyle: Lack of weight-bearing exercise reduces bone strength.
- Smoking & Alcohol: Both contribute to bone loss and increase fracture risk.
- High Sodium & Caffeine Intake: Excess sodium and caffeine can interfere with calcium absorption.
4. Medical Conditions & Medications
- Long-term steroid use weakens bones.
- Chronic conditions such as rheumatoid arthritis, diabetes, and gastrointestinal disorders affect bone health.
- Chemotherapy and certain medications for seizures and depression can impact bone density.
Symptoms of Osteoporosis
Osteoporosis does not typically cause noticeable symptoms until bone fractures occur. However, signs may include:
- Back Pain: Often caused by spinal fractures.
- Loss of Height: Due to compression fractures in the spine.
- Stooped Posture: Known as kyphosis, it results from spinal fractures.
- Fragile Bones: Increased risk of fractures from minor falls or impacts.
When to See a Doctor?
Consult a healthcare provider if you experience:
- Persistent back pain.
- Height loss over time.
- Frequent fractures.
- A family history of osteoporosis.
Complications of Osteoporosis
If left untreated, osteoporosis can lead to serious complications:
- Fractures: Increased risk of hip, spine, and wrist fractures.
- Chronic Pain: Bone fractures can cause persistent pain.
- Limited Mobility: Severe fractures may lead to reduced physical activity.
- Postural Changes: Spinal fractures can lead to a hunched posture.
- Increased Mortality Risk: Hip fractures, particularly in older adults, can lead to serious health complications.
How to Determine Bone Strength?
Bone Density Testing (DEXA Scan)
A bone mineral density (BMD) test measures bone strength and predicts fracture risk. It is recommended for:
- Women over 65 and men over 70.
- Postmenopausal women with risk factors.
- People with a history of fractures.
- Individuals on long-term steroid therapy.
Best Treatment Options for Osteoporosis
1. Lifestyle Modifications
- Quit Smoking & Limit Alcohol: Reduces bone loss and lowers fracture risk.
- Regular Exercise: Weight-bearing activities (walking, jogging, and resistance training) improve bone strength.
- Calcium & Vitamin D Intake: Essential for maintaining bone density. Include dairy, leafy greens, nuts, and fortified foods in your diet.
2. Medications for Osteoporosis
- Doctors may prescribe medications to slow bone loss and promote bone formation, including:
- Bisphosphonates: Help prevent bone loss and fractures.
- Hormone Therapy: Useful for postmenopausal women to maintain bone density.
- Monoclonal Antibodies: Improve bone strength and reduce fracture risk.
- Selective Estrogen Receptor Modulators (SERMs): Maintain bone density in postmenopausal women.
3. Preventive Measures
- Adequate Calcium & Vitamin D: Daily intake of at least 1,200 mg of calcium and 800–1,000 IU of vitamin D.
- Regular Physical Activity: Strengthens bones and improves balance.
- Healthy Diet: Avoid processed foods high in sodium and refined sugars.
- Routine Bone Density Tests: Early detection helps in effective management.
Osteoporosis in Men and Women
Although osteoporosis is more common in women due to hormonal changes, men are also at risk. Aging, low testosterone levels, and medical conditions can contribute to osteoporosis in men. Regular screening and preventive care are crucial for both genders.
Osteoporosis Prevention: Take Action Today
- Maintain a balanced diet rich in bone-healthy nutrients.
- Engage in weight-bearing and resistance exercises regularly.
- Avoid smoking and excessive alcohol consumption.
- Schedule bone density tests if at risk.
- Ensure adequate sun exposure for vitamin D production.
Frequently Asked Questions (FAQs) on Osteoporosis
What are the first signs of osteoporosis?
Back pain, height loss, and frequent fractures are early indicators.
Who is at the highest risk for osteoporosis?
Postmenopausal women, elderly individuals, and those with a family history of osteoporosis.
Can osteoporosis be reversed?
While osteoporosis cannot be fully reversed, treatment can slow bone loss and improve strength.
How much calcium do I need daily?
Adults need approximately 1,200 mg of calcium per day for optimal bone health.
Is osteoporosis preventable?
Yes, a healthy diet, regular exercise, and lifestyle changes can help prevent osteoporosis.
What foods should I avoid with osteoporosis?
Limit caffeine, alcohol, and high-sodium foods as they can reduce bone density.
Can men get osteoporosis?
Yes, though more common in women, men can also develop osteoporosis.
How does exercise help osteoporosis?
Weight-bearing exercises stimulate bone growth and maintain bone mass.
How often should I get a bone density test?
Every 2–3 years if at risk or as advised by your doctor.
Does osteoporosis cause joint pain?
Osteoporosis affects bones, not joints, but fractures can lead to chronic pain.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868