Pancreas Divisum - Symptoms, Causes, Types, Complications
Pace Hospitals
Pancreas divisum meaning
It is a congenital anomaly (birth defect) where dorsal and ventral buds of the pancreas fail to fuse during foetal development that occurs at approximately the seventh-week of pregnancy. As a result, rather than the major papilla, the majority of the pancreas drains into the minor papilla via the dorsal duct, commonly known as the duct of Santorini.
Pancreas divisum doesn't show any symptoms, however, 25 to 38 % of patients with pancreatic divisium can develop recurrent pancreatitis, which can eventually become chronic. It affects around 3% to 14% of the global population.
Pancreas divisum causes
In the initial process of pancreas formation, two different buds (dorsal and ventral) develop, dorsal bud towards the left and ventral bud at the right of the stomach. In the development process, the ventral bud makes a shift towards the left and fuse with the dorsal part and form a complete pancreas.
The ducts present inside the dorsal and ventral fuse together and form the main pancreatic duct or duct of Wirsung that connects to the common bile duct and opens into the duodenum (small intestine) via the major duodenal papilla. Through main pancreatic duct majority of the normal pancreas drains. The dorsal duct, in turn, is known as the Santorini duct, and it drains into the duodenum via the minor papilla.
The pancreas divisum develops when the ventral and dorsal ducts of the pancreas fail to join during development to form a main pancreatic duct, thus the majority of the pancreas drains into the minor papilla via the dorsal duct (duct of Santorini).
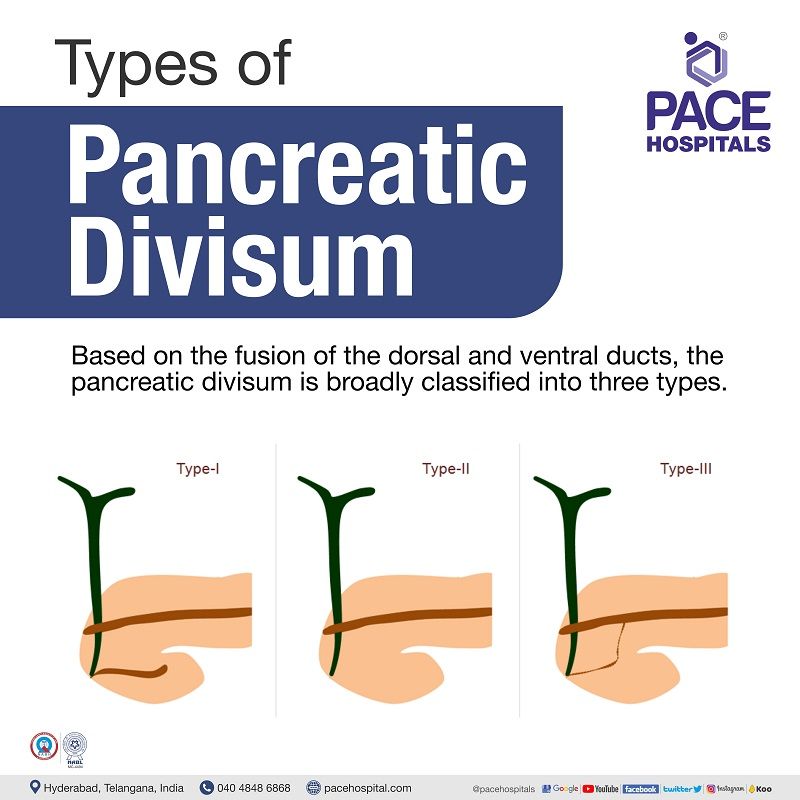
Types of Pancrease divisum
Based on the fusion and functionality of dorsal and ventral ducts, the pancreas divisum (PD) is broadly classified into four types.
- Type I pancreas divisum
- Type II pancreas divisum
- Type III pancreas divisum
- Type IV pancreas divisum
Type I pancreas divisum: It is also called a classic pancreatic divisum, where there is a complete failure of fusion between dorsal and ventral duct.
Type II pancreas divisum: In this type, there will be an absence of the ventral duct; therefore, the minor papilla drains the entire pancreas while the major papilla drains a portion of the common bile duct.
Type III pancreas divisum: It is characterised by a small remnant communication between the dorsal duct and ventral duct.
Type IV pancreas divisum: This is also known as Reverse PD, an unusual variation in which the Santorini duct (dorsal duct) does not connect with the main pancreatic duct, resulting in a small isolated component of the dorsal pancreas.
Pancreas divisum symptoms
The vast majority of patients born with pancreatic divisum will show no signs or symptoms of the condition. However, a few patients might show the following symptoms.
- Vomiting and nausea
- Pain in the abdomen (stomach)
- Inflammation of the pancreas (acute or chronic pancreatitis)
- Food intolerance
Pancreas divisum complications
Pancreas divisum can cause chronic or acute pancreatitis, leading to malnutrition.
Pancreas divisum diagnosis
Magnetic resonance cholangiopancreatography (MRCP) is the most prevalent method of diagnosing pancreatic divisum by the gastroenterologist. Other diagnostic methods include:
- Endoscopic Retrograde Cholangiopancreatography (ERCP)
- Computed tomography (CT scan)
- Magnetic resonance imaging (MRI)
Magnetic resonance cholangiopancreatography (MRCP)
The MRCP produces comprehensive pictures of the pancreas and pancreatic ducts using a strong magnetic field and radio waves. The patient will be administered with a contrast material intravenously. The patient needs to be in supine position in the MRI scanner while the pancreas is scanned.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
This is a non-invasive procedure, where a flexible tube containing a tiny camera will be inserted into the mouth through the stomach and small intestine (duodenum). The gastroenterologist will inject a radiopaque dye and takes X-ray images of the pancreas.
Computed tomography (CT scan)
This is a test that uses a combination of X-rays and computers to produce images of the pancreas.
Magnetic resonance imaging (MRI)
This testing method uses magnetic fields and radio waves to produce images of the pancreas. During this exam, the patient lies in enormous tubular magnet machines. These machines realign the water molecules in the patient’s body before using radio waves to make cross-sectional photographs.
Pancreas divisum treatment
The treatment of pancreas divisum generally involves symptomatic management. In many cases, the patient might not have any symptoms. In patients with symptomatic pancreas divisum, papillotomy of the minor papilla, with or without plastic stent implantation, is the first choice for therapeutic intervention.
The surgery generally involves the widening of the minor papilla (opening the vent of the dorsal duct into the small intestine) and increasing the flow of the pancreatic juices. The gastroenterologist might insert a stent into the duct for further closure and blockage.
Frequently Asked Questions - FAQs
Related article:
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles















