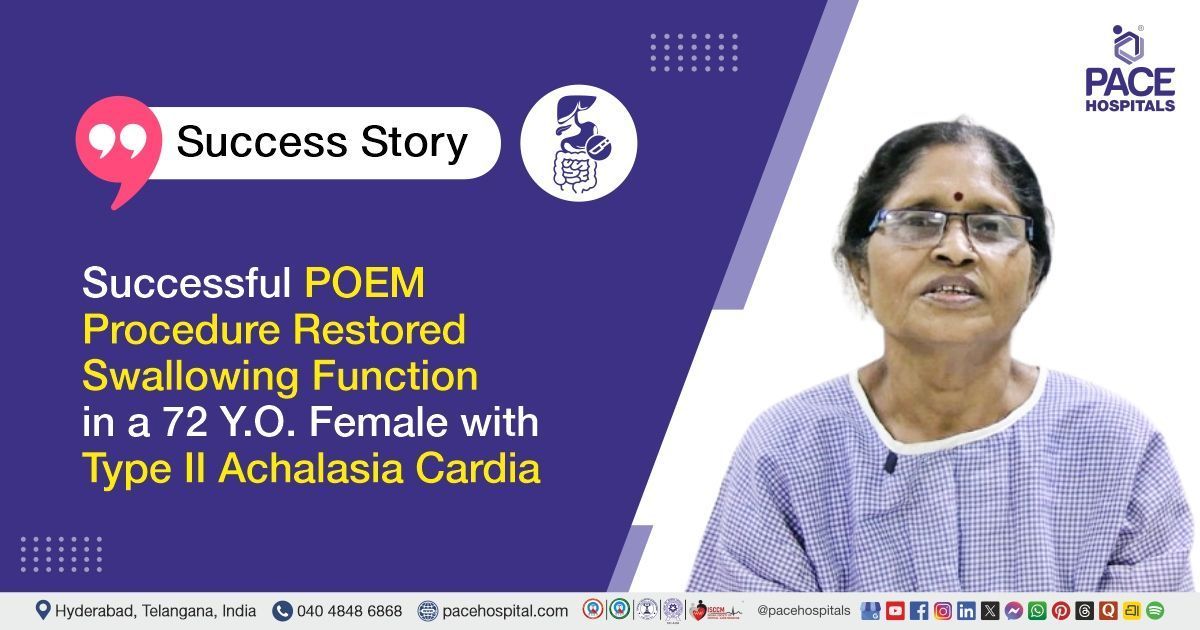
Transforming Dysphagia Management in Achalasia with Peroral Endoscopic Myotomy
PACE Hospitals
PACE Hospitals' Gastroenterology team successfully performed a POEM (PER ORAL ENDOSCOPIC MYOTOMY) procedure on a 43-year-old female with achalasia cardia (Eckardt's score: 11), improving her ability to eat and swallow comfortably.
Medical History
A 43-year-old female patient approached the gastroenterology department of PACE Hospitals, Hyderabad, complaining of difficulty swallowing both liquids and solids for 20 days. The patient also appeared to have lost weight and had a history of regurgitation (the act of bringing swallowed food back into the mouth) and excessive belching (Excessive belching is the frequent release of gas from the stomach through the mouth, often due to swallowed air or digestive issues). The patient was known case of mild dysphagia (swallowing difficulties) for two years.
On Examination
The patient’s physical examination was normal. Her systemic examination was normal except for the respiratory system, which showed bilateral normal vesicular breath sounds (RS -B/NVBS - which is generally considered abnormal, as it suggests the presence of a condition or factor that may require further evaluation).
Upon evaluating the patient’s medical history, no other existing comorbidities were observed. She was conscious and coherent when she approached the hospital, with no pallor or icterus.
Diagnosis
Considering the severity of the patient’s swallowing difficulty, she was admitted to PACE Hospitals, Hyderabad, for further treatment and management of her medical condition. She underwent an endoscopy and a barium swallow test. Endoscopy helps widen the oesophageal lumen and check for food residue in the oesophagus, whereas a barium swallow test assesses the oesophageal motility.
The diagnostic procedures were performed, and an oesophageal manometry procedure was done thereafter, which again revealed
Achalasia Cardia type 1 with Eckardt’s score of 11 and median integrated relaxation pressure (IRP) of 45.3 (<15mmHg considered normal). The patient was also diagnosed with Bronchial Asthma.
Treatment
As the patient was diagnosed with achalasia cardia type I with severe difficulty in swallowing, the interventional gastroenterologist, transplant hepatologist, pancreatologist and endosonologist Dr. Govind Verma, and other gastroenterologists, hepatologists and therapeutic endoscopists affirmed that Peroral Endoscopic Myotomy (POEM) procedure would help the patient recover from dysphagia and provide relief from symptoms associated. The patient was referred to the consultant interventional pulmonologist, Dr Pradeep Kiran Panchadi, to manage bronchial asthma.
On the day of the procedure, the patient was explained about the disease condition and treatment modality, and consent was obtained from her. Short-acting general anaesthesia was administered as premedication.
To prevent infection, she was priorly given antibiotics before the myotomy procedure. CO2 monitoring was done continuously throughout the procedure. An
Upper Gastrointestinal (UGI) endoscopy was done initially to examine the fundus. It appeared normal, but moderate resistance was felt at the gastroesophageal junction at 39 Cm. The mucosa was infiltrated with diluted methylene blue 9 cm above the gastroesophageal junction. Submucosal tunneling was done by an incision in the mucosa with a T- knife. Vessels were coagulated with a coag grasper, and a hybrid knife was used to incise circular muscle. After the procedure, the tunnel was closed with medorah clips, and the endoscope was passed across the gastroesophageal junction much easier.
Post-procedure
The procedure was successfully done with no complications. The patient was managed with intravenous fluids, antibiotics, proton pump inhibitors and other supportive care during hospitalization. She was strictly kept on ‘nil by mouth’ (NBM) for two days post-procedure. The oral gastrograffin test revealed no evidence of contrast extravasation, and transient retention of contrast was seen in the lower oesophagus. Later, the patient was discharged with medical advice.
Discharge notes
While she was discharged, the patient was stable and well-tolerant to a liquid diet. She was also prescribed antibiotics, antifungals, proton pump inhibitors, and antihistamines (anti-allergic drugs).
She was advised to consume a liquid diet followed by a soft diet for the next five days. She was objected to consuming cool liquids to preserve the oesophagus's better motility.
With a prior appointment, the patient was asked to get reviewed by Dr. Govind R Verma in OPD after a week. However, she was instructed to admit herself anytime in the
medical emergency ward in case of adverse symptoms like fever, abdominal pain, or vomiting.
Integrated relaxation pressure (IRP)
Integrated relaxation pressure (IRP) is a metric that measures the average pressure in the esophagogastric junction (EGJ) during a period of relaxation after swallowing, and it is defined as the average of the lowest pressure in the EGJ for the first four seconds within 10 seconds of swallowing. It assesses the relaxation of the lower oesophageal sphincter (LES) and the completeness of the upper oesophageal sphincter (UES) relaxation.
Healthcare professionals consider it as an essential metric for diagnosing oesophageal motility diseases and differentiating between intact and impaired EGJ relaxation. IRP values can differ based on position, measurement system, and analysis software. For instance, IRP values greater than 15 mmHg in the Sierra system suggest an obstruction at the EGJ outflow. Lower IRP values are associated with reflux-predominant disease, while higher IRP values are related to dysphagia-predominant disease.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868