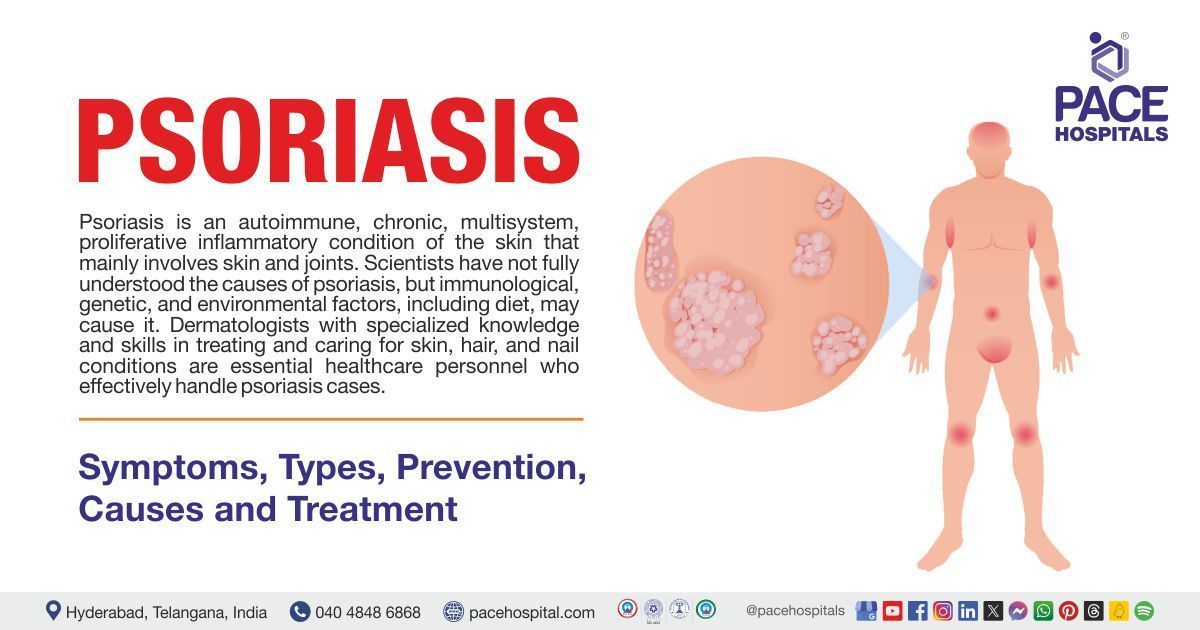
Psoriasis - Symptoms, Types, Causes, Prevention and Treatment
Psoriasis definition
Psoriasis, an autoimmune disorder, is a chronic (long-lasting), multisystem, proliferative (multiplying in number rapidly) inflammatory condition of the skin that mainly involves skin and joints.
Psoriasis is common in all age groups, from children to adolescents. It is seen as erythematous plaques covered with silvery scales, mainly over the extensor surfaces, lumbosacral region, and scalp. The disorder can also affect the eyes and joints. Some people with psoriasis may experience itching or soreness. Sometimes, the signs and symptoms of psoriasis will flare up for a few weeks or months; then, they will subside or go into remission (decrease in symptoms).
Scientists have not fully understood the causes of psoriasis, but immunological, genetic, and environmental factors, including diet, may cause it. The distribution and appearance of lesions determine the diagnosis of psoriasis, and the type and severity of the disease determine the treatment. Dermatologists with specialized knowledge and skills in treating and caring for skin, hair, and nail conditions are the essential healthcare personnel who effectively handle psoriasis cases.
Psoriasis meaning
The term psoriasis was first introduced by Greek physician Galen (133-200), meaning an itchy, exfoliative condition of the eyelids and scrotum, similar to the modern definition of seborrheic dermatitis, that was treated with a viper’s broth.
Psoriasis prevalence
Prevalence of psoriasis in the World
The prevalence of psoriasis among adults ranges from 0.91 to 8.5%, while in children, it varies from 0.0 to 2.1%, according to estimations of epidemiological data on psoriatic illness. Around 2-3% of people worldwide suffer from psoriasis, with prevalence rates as high as 8–11% in several Northern European nations. In 2017, there were 811 cases of psoriasis per 100,000 people worldwide, or roughly 0.84% of the world's population, or 64.6 million people. From 92 instances per 100,000 in 1990 to 99 in 2017, the incidence of new cases rose. Asia and the Western Pacific areas had the lowest rates, while North America and Western Europe had the highest rates.
Prevalence of psoriasis in India
The frequency of adult psoriasis in India ranges from 0.44 to 2.8%. The majority of patients are in their third or fourth decade at the time of clinical manifestation, and it affects men twice as frequently as it does women.

Psoriasis types
While there are various types of psoriasis, the plaque form is the most prevalent and affects the scalp, limbs, and trunk. The following are the three main types of psoriasis:
- Plaque psoriasis
- Pustular psoriasis
- Generalized pustular psoriasis (GPP)
- Localized pustular psoriasis
- Acrodermatitis continua of hallopeau (ACH)
- Psoriatic arthritis
Plaque psoriasis
Plaque psoriasis is the most frequent form of psoriasis and occurs in 85%–90% of affected patients. It is identified by oval or irregularly shaped, sharply demarcated, red-raised plaques covered by silvery scales.
Although plaques can affect any part of the body, and most frequently it develops symmetrically in the elbows, knees, and hands' lower back, scalp, and extensor surfaces. Lesions can vary in size, giving rise to two distinct clinical sub-phenotypes: larger, solitary lesions or smaller, confluent patches.
An additional classification considers the age of onset. Type I psoriasis manifests before age 40, is frequently linked to a well-known medical history, and has a strong correlation with the HLA-Cw0602 variant. In contrast, type II psoriasis appears after age 40.
Pustular psoriasis
Pustular psoriasis most commonly present in the form of aseptic pustules. It is further classified into three subgroups:
- Generalized pustular psoriasis (GPP): It has a large skin rash characterized by aseptic abscesses and includes a varied degree of fever as the acute beginning symptom and is later associated with general malaise, exhaustion, and other systemic symptoms. It can affect population of any age and is more seen in women than in males.
- Localized pustular psoriasis: It is the most widespread type of pustular psoriasis and is termed palmoplantar pustulosis (PPP). Patients with pustular psoriasis may experience tiny skin blisters filled with pus. In cases of pustular psoriasis, it may affect body parts, including extremities,
- Acrodermatitis continua of hallopeau (ACH): This unusual form of psoriasis affects the phalanges of the hands and feet; many blister crops fuse on the nail bed and matrix, generating pus streams that cause the nails to dystrophy (abnormal changes in the shape and color, and growth of the fingernails or toenails) and the affected digits to become anonychia (absence of nails).
Psoriatic arthritis
Psoriatic arthritis is an inflammatory muscular condition linked to psoriasis of the skin that can affect 20-30 % of individuals. It can affect different tissues such as synovium, bone, tendons, cartilage, and entheses (connective tissue between tendon or ligament and bone).

Psoriasis symptoms
The symptoms of psoriasis may change from one person to the other. Symptoms may flare up at specific periods, making people feel worse, and then subside at different times. Following are some of the common symptoms of psoriasis:
- Psoriasis plaques: Patches of thick, red skin associated with silvery-white scales, usually on the elbows, knees, scalp, trunk, palms, and soles of the feet, that are itchy or burned.
- Nail abnormalities: Pitted, ridged, thick nails.
- Skin dryness and irritation: Dry, cracked skin that bleeds or itches, shedding of scales of skin.
- Sleep disturbances: Inadequate quality of sleep.
Psoriasis risk factors
Some triggering factors can make psoriasis patients' symptoms worse. Knowing these factors may help avoid a flare-up. The following are some of the risk factors for psoriasis.
The risk factors for psoriasis are mainly divided into two groups one is extrinsic and the other intrinsic risk factors.
Extrinsic risk factors of psoriasis
- Infection: Psoriasis occurs after streptococcal and Staphylococcus (S.) aureus infection. Human immunodeficiency virus (HIV) is also a well-known risk factor associated with psoriasis.
- Air pollution: The rise in air pollution has had significant effects on human skin. Air contaminants, including cadmium, influence the etiology of psoriasis.
- Vaccination: Numerous studies demonstrated the link between influenza vaccination and psoriasis exacerbation. Vaccination against influenza may potentially cause psoriasis to develop.
- Alcohol: Consumption of alcohol has been associated with an increased risk of psoriasis. Yet, a previous systematic research concluded that there wasn't enough information to say whether drinking alcohol was a risk factor.
- Smoking: A comprehensive review and meta-analysis found that people with psoriasis are more likely to smoke, either now or in the past. Smokers have an increased risk of developing psoriasis.
Intrinsic risk factors of psoriasis
- Obesity: The onset and aggravation of psoriasis are closely correlated with obesity. The prevalence and risk of obesity are much increased in psoriasis patients.
- Diabetes mellitus: A meta-analysis linked psoriasis to diabetes mellitus. Many other meta-analyses have also demonstrated a link between psoriasis and the risk of diabetes mellitus.
- Hypertension: A meta-analysis revealed a greater incidence and prevalence of hypertension among psoriasis patients.
- Mental stress: Most people agree that mental stress is a known cause of psoriasis, and people with psoriasis believe that mental stress exacerbates their illness.
- Dyslipidaemia: Patients with dyslipidaemia are more likely to have psoriasis; as psoriasis worsens, this incidence is predicted to increase.

Psoriasis causes
Though the exact cause of psoriasis is not known, skin cells that grow and shed excessively quickly are assumed to be the reason. Following are some of the known causes of psoriasis:
- Abnormal growth of the skin cells: In the skin's deepest layer, the body generates new skin cells. These skin cells ascend the skin's layers gradually until they reach the outermost layer; they decompose and fall off. Usually, this entire process takes three to four weeks, but it takes only 3-7 days in psoriasis patients. This leads to immature cells rapidly accumulating on the skin's surface, producing dry, crusty areas that are coated with scales.
- Immune system problems: T-cells normally travel through the body to detect and fight invading germs (like bacteria), but in psoriasis patients, they start to attack healthy skin cells by mistake, causing rapid production of new skin cells, thus triggering the immune system.
- Genetics: Although the specific role that heredity plays in psoriasis is unknown, psoriasis runs in families, so having a close family with the condition may increase the risk of developing psoriasis.

Psoriasis complications
Patients with psoriasis are highly affected by a range of systemic problems and comorbidities that are linked to the disease. Below are some of the complications of psoriasis.
- Psoriatic arthritis: Patients with psoriasis may develop psoriatic arthritis (PsA), a chronic inflammatory joint disease. It is one of the main psoriasis-related problems.
- Risk of lymphoma: Individuals who have psoriasis appear to be at a slightly greater risk of developing cancer, specifically lymphomas and keratinocyte carcinoma.
- Increased risk of adverse cardiac events: Heart disease is up to 50% more common in psoriasis patients, and the risk of cardiovascular (CV) disease rises with skin severity.
- Possibly inflammatory bowel disease: There has been evidence of a strong correlation between psoriasis and inflammatory bowel disease (IBD), a chronic, recurring immune-mediated inflammatory illness.
- Diabetes: Additionally, psoriasis has been connected to a higher incidence of type 2 diabetes mellitus. It may result in insulin resistance, which is a major cause of type 2 diabetes.
- Hypertension: Endothelial dysfunction and arterial stiffness are risk factors for hypertension that may be exacerbated by the chronic inflammation linked to psoriasis.
- Depression: Depression among psoriasis sufferers is often caused by social judgment and low confidence resulting from the disease.
Obesity, hyperlipidemia, mitral valve prolapse coeliac disease, and eye conditions, including blepharitis, conjunctivitis, and uveitis, are some of the other complications of psoriasis.
Difference between Eczema and Psoriasis
Eczema vs psoriasis
Eczema and psoriasis are both chronic (long-lasting) skin conditions that may cause the same symptoms. The exact cause of both conditions is not known, but the immune system may play a significant role in psoriasis. Yet below are some parameters that can differentiate eczema and psoriasis:
| Parameters | Eczema | Psoriasis |
|---|---|---|
| Definition | Eczema, also known as atopic dermatitis, is a frequent chronic(long-lasting) skin condition that can cause recurrent infections and poor quality of life if left untreated. | Psoriasis is an autoimmune disorder that is chronic(long-lasting), multisystem, proliferative (multiplying in number rapidly), and an inflammatory condition of the skin that mainly involves the skin and joints. |
| Symptoms | Dry, red, itchy skin, most frequently seen in the creases of elbows, behind the knees, ankles and wrists. | Patches of thick, red skin associated with silvery-white scales, usually on the elbows, knees, scalp, trunk, palms, and soles of the feet, that are itchy or burned. |
| Cause | The exact cause of atopic eczema is not known. | Though the exact cause of psoriasis is not known, skin cells that grow and shed excessively quickly are assumed to be the reason. |
| Treatment | Topical therapy, phototherapy, systemic therapy, biologic therapy and antihistamines | Topical therapy, phototherapy, systemic therapy, biologic therapy and medicated shampoos |
Difference between Scalp Psoriasis vs Dandruff
Scalp psoriasis vs dandruff
Small, white flakes are produced by both dandruff and scalp psoriasis and can be seen in the hair, neck, and shoulders. However, the causes of the two illnesses are completely different. Below are some of the parameters that can differentiate scalp psoriasis and dandruff:
| Parameters | Scalp psoriasis | Dandruff |
|---|---|---|
| What is it | Psoriasis can affect the scalp, and the scaly red patches it causes can flake off. | A common skin condition is dandruff, characterized by flakes that fall off the scalp and stick to hair or clothes. |
| Duration | Chronic (long-lasting) | Not long-lasting (may come and go) |
| Cause | Though the exact cause of psoriasis is not known, skin cells that grow and shed excessively quickly are assumed to be the reason. | A common causative agent is lipophilic yeasts Malassezia spp. (previously Pityrosporum) |
| Preventable | It cannot be prevented | Can be prevented |
Psoriasis prevention
Psoriasis cannot be prevented. However, some things can be done to lessen the frequency of psoriasis flare-ups or to aid with symptoms. Below are some of the measures that help in reducing the severity of symptoms:
- Diet: A healthy, low-glycaemic diet may be a helpful adjunct in managing and preventing moderate nonpustular psoriasis.
- Avoiding alcohol and smoking: Increased smoking or consumption of alcohol increases the risk of developing psoriasis and may influence the severity of the disease; hence, it needs to be avoided.
- Baths: Patients with psoriasis can soften and lift their scales by soaking in warm water with a bath oil or tar solution and using a soft brush.
- Avoiding OTC medications: Over-the-counter and prescription drugs that are known to worsen psoriasis should be avoided by people who have psoriasis.
Psoriasis diagnosis
The diagnosis is mainly clinical. Although psoriasis is typically easy to diagnose, there are occasions when it can be challenging since some of the symptoms, such as erythema and scaling can also be seen in other skin conditions. Following are some of the steps involved in diagnosing psoriasis:
- Medical history
- Physical examination
- Laboratory studies
- Complete blood cell (CBC) count
- Blood urea nitrogen (BUN), creatinine
- Liver function tests (LFTs)
- Tuberculosis (TB) screening
- Hepatitis panel
- Pregnancy test
- Erythrocyte sedimentation rate (ESR)
- Rheumatoid factor (RF)
- Uric acid level
- Fungal studies
- Imaging tests
- Bone scans
- Joint x-rays
- Dermatoscopy
- Skin biopsy
Psoriasis treatment
Treatment of psoriasis is based on type and severity and the area of skin that is affected. Different treatment options are available for psoriasis, but it is challenging to identify the most effective one. Below are the treatment options available for psoriasis patients.
Topical therapy
- Ointments
- Creams
- Vitamin D analogues
- Coal tar
- Calcineurin inhibitors
- Dithranol
Phototherapy
- Ultraviolet B (UVB) phototherapy
- Psoralen plus ultraviolet A (PUVA)
- Narrowband UVB light (NBUVB)
- Combination light therapy
Systemic therapy
- Oral medications
- Injectable medications
Biologic therapy
- TNF-α inhibitors
- IL23 inhibitors
- IL36 receptor antagonist
- IL17 inhibitor
- Janus kinase inhibitor (JAK)
- Sphingosine one phosphate (S1P) agonist
- AHR agonist (tapinarof)
- Rho-associated kinase inhibitor (ROCK2)
Frequently Asked Questions (FAQs) on Psoriasis
Is psoriasis contagious?
No, psoriasis is not a contagious disease (spread of a disease by either direct or indirect contact) as it does not spread by air or water. In 2014, the World Health Organization recognized it as a major non-communicable disease.
How to cure psoriasis permanently?
While there is no exact cure for psoriasis, numerous treatment options are available now, such as topical, photo, systemic, and biologic therapies, which are used to treat psoriasis symptoms.
Is psoriasis genetic?
Although the specific role that heredity plays in psoriasis is unknown, research has shown that numerous genes have been connected to the development of psoriasis. However, having those genes does not necessarily mean that people will have psoriasis.
Is psoriasis linked to vitamin D deficiency?
Research has indicated that psoriatic patients have a significant prevalence of vitamin D deficiency in their serum. There is a strong correlation between vitamin D levels and the severity of psoriatic illness.
Is psoriasis dangerous?
In some rare cases, psoriasis may lead to the risk of causing other serious conditions, including psoriatic arthritis and cardiovascular events, such as heart attacks and strokes.
What is psoriasis?
Psoriasis is a chronic (long-lasting) condition caused by an overactive immune system that multiplies skin cells too quickly. Skin becomes scaly and irritated in patches, usually on the knees, elbows, or scalp, but it can also affect other body parts.
What is scalp psoriasis?
Scalp psoriasis is usually the initial presentation(symptom) of psoriasis, and almost 80 % of psoriasis patients will eventually experience it. It is a chronic autoimmune illness characterized by erythematous, well-defined skin covered with thick scales, which are often silvery white.
Is psoriasis itchy?
Over the last ten years, a growing body of research has demonstrated that itching can be among the most common and bothersome symptoms of psoriasis, impacting nearly all psoriatic patients to some extent.
Can diet help psoriasis?
A healthy, low-glycaemic diet may be a helpful adjunct in managing and preventing moderate nonpustular psoriasis. It may lessen the severity of the symptoms or lessen flare-ups (more intense) of psoriasis.
Does acupuncture help psoriasis?
Research has indicated that acupuncture can be helpful in treating plaque psoriasis. While the exact mechanism of acupuncture's effects on psoriasis remains unclear, there is evidence that, when combined with other treatments like phototherapy, it can reduce the inflammation and excessive thickening of skin lesions associated with plaque psoriasis.
How effective is light therapy for psoriasis?
Psoriasis is typically successfully treated with light therapy; 50-90 out of 100 psoriasis cases, the symptoms are thought to significantly improve or disappear entirely for a period.
Is psoriasis worse in winter?
A three-year study utilizing the Physician Global Assessment severity scale revealed that doctors had seen an increase in psoriasis and acne in the winter and a decrease in the same conditions in the summer.
Is psoriasis an autoimmune disease?
Yes, psoriasis is an autoimmune disease in which the body's immune system turns on itself and attacks normal cells and tissues—in this case, skin cells known as keratinocytes.
Does scalp psoriasis cause hair loss?
One of the most common signs of psoriasis is the involvement of the scalp in affected individuals. Psoriasis on the scalp often results in hair loss.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868