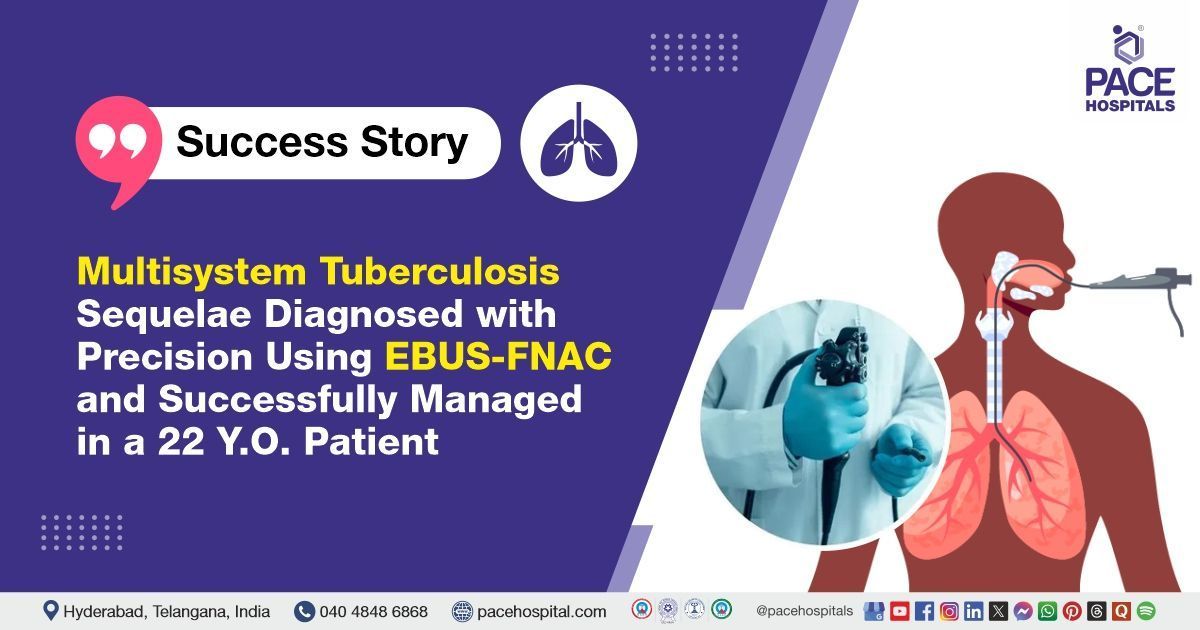
Multisystem TB Sequelae Diagnosed with Precision Using EBUS and Successfully Treated
PACE Hospitals Pulmonologist team successfully carried out an EBUS-guided FNAC (Fine Needle Aspiration Cytology) on a 22-year-old female patient suffering from a non-resolving pneumonia in the right upper lobe, mediastinal lymphadenopathy, a history of old disseminated tuberculosis, and acyanotic congenital heart disease.
Chief Complaints
A 22-year-old female patient presented for evaluation of non-resolving pneumonia affecting the right upper lobe at
PACE Hospitals, Hitech City, Hyderabad.
Medical History
The patient was asymptomatic. However, during follow-up, non-resolving
pneumonia was detected in the right upper lobe.
On Examination
The patient had a history of disseminated tuberculosis involving the abdominal, pulmonary, and skeletal systems, for which she completed a six-month course of anti-tubercular therapy (ATT). She also had a history of moderate anaemia and received one unit of packed red blood cells (PRBC) transfusion. There is no known history of drug or food allergies, nor any previous episodes of ATT-induced hepatitis. The patient has received two doses of the COVID-19 vaccine.
Her menstrual cycles are regular, occurring every 30 days and lasting for five days with normal flow. She does not experience dysmenorrhea and reports occasional leucorrhea. Her last menstrual period (LMP) occurred in mid-February.
The patient does not have a history of hypertension, diabetes, or thyroid disorders. She has a known heart condition called acyanotic congenital heart disease, specifically patent ductus arteriosus (PDA), where she was born with a small hole in her heart's blood vessels, which usually closes shortly after birth but has remained open in her case.
Fortunately, this condition doesn't cause a lack of oxygen in the blood, and it is being managed with a conservative approach, meaning no immediate surgery is needed. Additionally, she has no history of COVID-19 infection.
Diagnosis
Upon admission to PACE Hospitals, the patient’s vital signs were stable. General examination revealed that she was conscious and oriented, with no signs of respiratory distress. There was no tenderness over the paranasal sinuses, and no evidence of peripheral lymphadenopathy. The posterior pharyngeal wall appeared normal. Cardiovascular examination showed normal S1 and S2 heart sounds. On chest examination, bilateral vesicular breath sounds (VBS) were noted. Abdominal examination revealed a soft abdomen with positive shifting dullness (PSD+).
Medical Decision-Making
After being admitted to PACE Hospitals, the pulmonologist thoroughly reviewed the patient's medical history and conducted a detailed examination. Initial investigations showed normal renal and liver function, prothrombin time, and thyroid profile. However, the erythrocyte sedimentation rate (ESR) was elevated, and her blood group was identified as B positive.
A 2D echocardiogram confirmed the presence of a patent ductus arteriosus with a minimal left-to-right shunt. A cardiology consultation was obtained, and device closure was recommended for this congenital heart condition.
Further imaging through Contrast-enhanced CT (CECT) revealed the following:
- Focal subsegmental consolidation in the posterior segment of the right upper lobe.
- A loculated hypodense pleural collection in the posterior basal aspect of the left lower lung.
- A focal lytic lesion at the left lateral aspect of the 8th rib.
These findings, combined with the clinical suspicion, led to the decision to proceed with an EBUS-guided FNAC procedure to further investigate the cause of the patient's symptoms, ultimately confirming an active tuberculosis.
Based on the patient's current condition, the doctors recommended performing an EBUS-FNAC (Endobronchial Ultrasound)-Guided (Fine Needle Aspiration Cytology) to investigate the underlying cause of the patient's non-resolving pneumonia, which was suspected to be linked to active tuberculosis.
The procedure was carried out as part of the patient's active tuberculosis treatment in Hyderabad, India, under the care of the Pulmonology Department. The goal was to confirm the underlying etiology of the pneumonia and guide the most appropriate management strategy for her condition.
Surgical Procedure
After consulting with the consultant pulmonologist, Dr. Pradeep Kiran P, along with other specialists including Dr. Seshi Vardhan Janjirala, a comprehensive evaluation was conducted to determine the most appropriate diagnostic approach for the patient. Based on their collective expertise, it was concluded that an EBUS-guided FNAC (Endobronchial Ultrasound-Guided Fine Needle Aspiration Cytology) would be the most suitable procedure to further investigate and confirm the underlying cause of the patient’s condition.
Postoperative Care
Following the clinical suspicion, the patient was scheduled for an EBUS-guided FNAC procedure in Hyderabad at PACE Hospitals, under the expert supervision of the Pulmonology Department.
The procedure was performed under general anaesthesia and revealed mucosal fibrosis in the right upper lobe, along with a large, heterogeneous, matted subcarinal lymph node exhibiting necrosis, measuring 18.9 x 22.1 mm. Bronchoalveolar lavage (BAL) was collected from the right upper lobe, and three passes of EBUS-guided FNAC were taken from the station 7 (subcarinal) lymph node and sent for further analysis. Rapid On-Site Evaluation (ROSE) during the procedure revealed features suggestive of necrotizing inflammation.
GeneXpert testing of the EBUS FNAC sample detected Mycobacterium tuberculosis (MTb) with a low bacterial load and no Rifampicin resistance, confirming the diagnosis of active tuberculosis.
Discharge Medications
During her hospital stay, the patient was managed with intravenous antibiotics, proton pump inhibitors (PPIs), and anti-tubercular therapy (ATT), along with other supportive measures.
Anti-tubercular therapy (ATT) was initiated as per RNTCP guidelines, tailored to the patient’s weight band of 43.2 kg. Bronchoalveolar lavage (BAL) and EBUS FNAC samples were sent for AFB culture, with results expected in approximately two months.
Discharge notes
The patient was discharged in a stable condition.
Condition at Discharge
The patient was conscious and oriented, with no active complaints. Her vital signs are stable, with a pulse rate of 78 beats per minute, blood pressure of 110/70 mmHg, and oxygen saturation of 98% on room air. Cardiovascular examination revealed normal heart sounds (S1, S2+), and chest examination showed bilateral vesicular breath sounds.
Discharge Medications
Upon discharge, the patient was prescribed antibiotics, proton pump inhibitors (PPIs), antitubercular agents, antimycobacterial, vitamin supplements, and antitussives.
Advice on Discharge
The treating doctor has advised that the anti-tubercular therapy (ATT) course may need to be extended for up to 18 months, especially if skeletal lesions persist beyond 12 months of treatment. The patient has been instructed to maintain adequate hydration by drinking plenty of water throughout the course of therapy.
The doctor informed the patient that mild side effects such as nausea, vomiting, joint pains, itching without rashes, and orange-coloured urine are commonly observed with ATT and generally do not require immediate intervention. However, the patient was clearly advised to report to the hospital immediately if she experiences serious symptoms including persistent vomiting, severe abdominal pain, yellowing of the eyes or skin (jaundice), visual disturbances, severe skin rashes, swelling, difficulty in breathing, or excessive fatigue, as these may indicate potential drug-related complications.
Additionally, the patient was advised to undergo liver function tests (LFTs) and serum uric acid levels every two weeks during the initial two months of treatment to closely monitor for any adverse effects.
Dietary
The patient was advised to follow a high-protein diet, which should include at least two eggs per day, to support recovery and improve overall nutritional status during the course of treatment.
Emergency Care
The patient was informed to contact the Emergency ward at PACE Hospitals in case of any emergency or development of symptoms like fever, abdominal pain, or vomiting.
Review and follow-up notes
The patient was advised to return for a follow-up appointment with both the Interventional Pulmonologists in Hyderabad at PACE Hospitals after five days, bringing along the BAL and EBUS-guided FNAC reports.
Additionally, a review with the Cardiologists was recommended to discuss the device closure of the patent ductus arteriosus. This visit will include a comprehensive evaluation, wound assessment, and monitoring of postoperative recovery.
Conclusion
This case highlights the importance of a multidisciplinary approach in the evaluation and management of acute miliary tuberculosis, guiding treatment strategies effectively in Hyderabad, India.
Advantages of the Minimally Invasive Approach in Geriatric Gynecologic Surgery
A pulmonologist/ pulmonology doctor plays a key role in performing EBUS-guided FNAC (Endobronchial Ultrasound-Guided Fine Needle Aspiration Cytology), utilizing bronchoscopy as a vital, minimally invasive, and highly effective diagnostic technique for thoracic diseases. By combining direct airway visualization with real-time ultrasound guidance, bronchoscopy enables precise localization and sampling of mediastinal and hilar lymph nodes or masses. This method is particularly valuable in diagnosing conditions such as tuberculosis, lung cancer, and sarcoidosis. Compared to traditional surgical biopsies, EBUS-guided FNAC via bronchoscopy offers reduced patient discomfort, lower risk of complications, and quicker recovery, making it a preferred diagnostic approach in contemporary pulmonary care.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868