Gestational Diabetes Mellitus (GDM) Causes, Symptoms, Risks Factors
Pace Hospitals
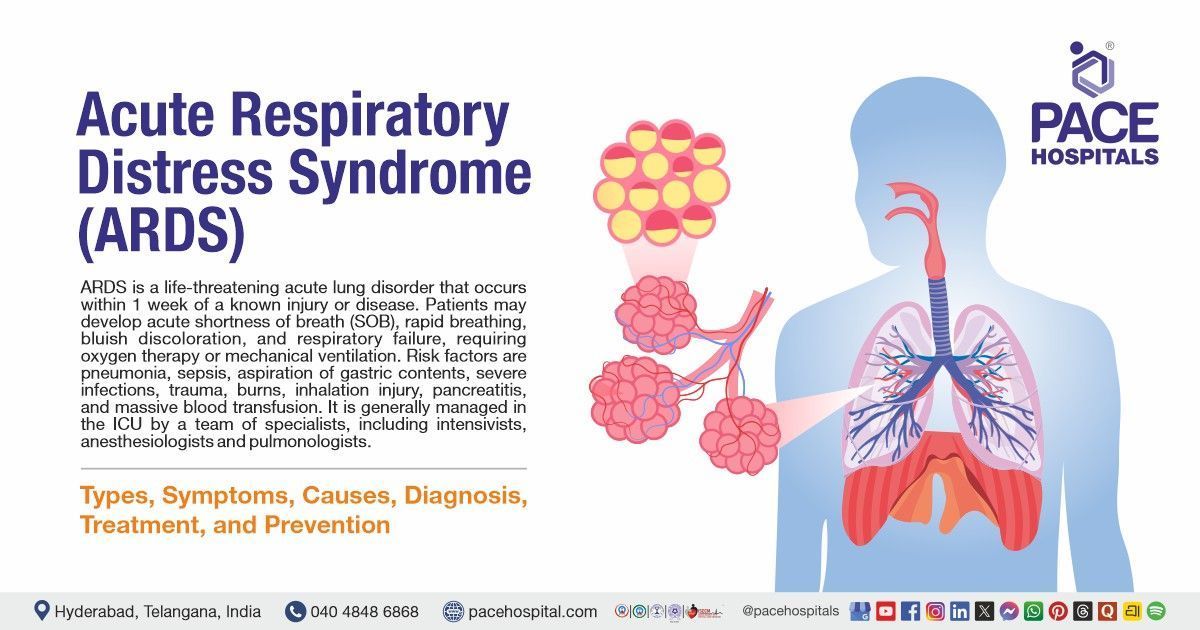
Gestational diabetes mellitus definition
It is defined as glucose intolerance that develops for the first time during pregnancy. Based on the requirement of medication to treat the condition, there are two types of gestational diabetes, such as Type 1 gestational diabetes mellitus (A1GDM) and Type 2 gestational diabetes mellitus (A2GDM). A woman with gestational diabetes has a 35 to 60% chances of developing type 2 diabetes over 10–20 years.
Human placental lactogen is the major hormone linked with increased insulin resistance in gestational diabetes (GDM), which is characterised by pancreatic beta-cell malfunction or delayed beta-cell responsiveness to glycaemic levels.
Types of Gestational Diabetes Mellitus (GDM)
There are two types of gestational diabetes mellitus which are categorised based on the treatment required.
- Type 1 gestational diabetes mellitus or A1GDM
- Type 2 gestational diabetes mellitus or A2GDM
Type 1 gestational diabetes mellitus or A1GDM
This type is also known as "diet-controlled gestational diabetes," as it can be managed without medication and will be responsive to nutritional therapy.
Type 2 gestational diabetes mellitus or A2GDM
This type of gestational diabetes can be treated with medicine to keep blood sugar levels in an optimum range.
Gestational diabetes causes
In a normal pregnancy, insulin resistance develops around the middle of the pregnancy and worsens during the third trimester. Hormones and adipokines released by the placenta, such as tumour necrosis factor (TNF), human placental lactogen, and human placental growth hormone, could be the causative factors for insulin resistance. In addition to this, when a woman is pregnant, her oestrogen, progesterone, and cortisol levels rise, leading to an imbalance between glucose and insulin.
To compensate the peripheral insulin resistance that occurs during pregnancy, a woman's pancreas secretes more insulin. Gestational diabetes develops when a woman's pancreas secretes insufficient insulin to keep up with the metabolic burden of insulin resistance.
In addition to the above, obesity and a high BMI are linked to chronic low-grade inflammation, according to several studies. Chronic inflammation leads to the synthesis of xanthurenic acid. This acid has been linked to the occurrence of prediabetes and gestational diabetes mellitus.
Gestational diabetes symptoms
Symptoms of gestational diabetes mellitus are uncommon. However, if the blood sugar levels reach too high, some women may experience the following symptoms such as:
- Polydipsia (excessive thirst)
- Polyurea (increase in the frequency of urination)
- Xerostomia (dry mouth)
- Genital itching
- Blurred vision
- General malaise
Risk factors for gestational diabetes
Gestational diabetes mellitus risk factors are as follows:
- Being overweight (BMI > 25)
- Low concentration of HDL
- Presence of polycystic ovarian syndrome
- High triglycerides level (> 200 mg/dL)
- Low physical activity
- Parents diagnosed with diabetes mellitus
- HbA1c greater than 5.7
- Previous history of gestational diabetes and cardiovascular diseases
- Abnormal oral glucose tolerance test
Gestational diabetes complications
The complications of gestational diabetes mellitus can affect both the mother and child if it is not adequately managed.
Mother complications:
- Preeclampsia (increase in blood pressure during pregnancy)
- More chances for C-section
- Probability of type 2 diabetes
In newborns
- Overweight baby
- Difficulty in breathing
- Preterm birth (early birth)
- Risk of obesity and type 2 diabetes in future
- Stillbirth
Gestational diabetes diagnosis
Diagnosis of gestational diabetes mellitus can be made in either of two procedures as per the American Diabetic Association and American College of Obstetrics and Gynaecology. It is tested at the 24th and 28th week of pregnancy.
- One-Step Strategy
- Two-Step Strategy
One-Step Strategy
It is a single-step procedure where 75 grams of oral glucose tolerance test is performed in the morning after an overnight fast. Blood samples are collected at fasting and post intake (1 hour and 2 hours) of 75 grams of glucose solution.
If the fasting blood glucose levels are more than 92 mg/ dL, 180 mg/dL for 1 hour (postprandial) and 153mg/dL for 2 hours (postprandial), it indicates the presence of gestational diabetes.
Two-Step Strategy
It is a two-step procedure where a glucose test is conducted with two different doses (50 and 100 grams) at different times, and the second one follows the first process.
In the first step, the patient will be given 50 grams of glucose regardless of the previous meal. If the blood glucose is more than 140 mg/ dL after one hour of glucose intake, step 2 will be initiated.
In step-2, the patient will be given 100 grams of glucose in the morning after overnight fasting (next day). Blood samples are collected at fasting and post-intake (1, 2 and 3 hours) 100 grams of glucose.
Gestational diabetes levels for step 2
The threshold values for women during pregnancy are as follows:
- Fasting blood glucose levels: 95 to 105 mg/ dL
- After one hour of glucose solution: 180 to 190 mg/dL
- After two hours of glucose solution: 155 to 165 mg/dL
- After three hours of glucose solution: 140 to 145 mg/dL
If two or more blood glucose values equal or surpass these threshold values, gestational diabetes mellitus is diagnosed.
Based on the results obtained, the diabetologist would like to assess the type of gestational diabetes mellitus the patient is suffering with.
Gestational diabetes treatment
Once the type of diagnosis is confirmed, the diabetologist would like to prescribe the therapy. Based on the type of gestational diabetes mellitus, the treatment is of two types.
- Pharmacological
- Non-Pharmacological
Pharmacological management of gestational diabetes mellitus
It is used in the treatment of type 2 gestational diabetes mellitus and also intype 1 gestational diabetes if the non-pharmacological approaches (diet and exercise) don’t work in controlling high blood glucose.
As per the American Diabetic Association, the first line treatment for gestational diabetes mellitus is insulin when women have high blood sugar levels or adequate blood glucose levels that are not manageable with diet and exercise therapy.
Based on the patient's blood sugar levels, the diabetologist prescribes the type of insulin. However, there is a change in the total daily insulin requirement as follows:
- First trimester 0.7 units/kg/day
- Second trimester 0.8 units/kg/day
- Third trimester 0.9 to 1.0 units/kg/day
Non-pharmacological
It is used in the treatment of type 1 gestational diabetes mellitus. The patient will be advised to engage in moderate aerobic exercise for at least 30 minutes per day or 150 minutes per week, as well as a diet rich in fruits (low glycaemic ones) and vegetables with three small to moderate meals and one to two snacks per day.
Prevention of Gestational Diabetes Mellitus
It is good to adhere to the following to prevent from having gestational diabetes before getting pregnant:
- Losing weight
- Getting regular exercise
- Include a diet rich in fibre and low glycaemic index food
Losing weight after being pregnant is not suggestive, as the mother needs to put on some weight for a healthy baby.
Frequently asked questions
Related Articles

Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868