Fluctuating Blood Sugar in Diabetes: Why It Happens & How to Keep It Stable
PACE Hospitals
Written by: Editorial Team
Medically reviewed by: Dr. Tripti Sharma - Consultant Endocrinologist (Adult & Paediatric), Physician & Diabetologist
Fluctuating blood sugar levels known as glycemic variability are among the most significant challenges in diabetes management. These unpredictable rises (hyperglycemia) and drops (hypoglycemia) can influence mood, energy, concentration, and organ function. Over time, uncontrolled fluctuations increase the risk of complications such as heart disease, kidney damage, nerve problems, eye disorders, poor wound healing, and frequent infections.
Maintaining stable blood glucose is essential for individuals with Type 1 diabetes, Type 2 diabetes, or gestational diabetes. Understanding what causes sugar instability, how to identify symptoms early, and what measures help restore balance can significantly improve long-term health outcomes.
This guide explains why blood sugar fluctuates, who is more vulnerable, how to diagnose the causes, and effective strategies to stabilise glucose levels for the long term.
What Are Fluctuating Blood Sugar Levels?
Fluctuating blood sugar refers to repeated and unpredictable swings in glucose levels throughout the day. These include:
- Hyperglycemia – High blood sugar
- Hypoglycemia – Low blood sugar
- Rapid shifts between high and low levels
Stable blood sugar supports brain function, energy regulation, cell repair, immunity, and healthy metabolism.
Ideal Blood Sugar Targets (General Guidelines)
- Fasting: 80–130 mg/dL
- Post-meal (2 hours): <180 mg/dL
- HbA1c: 6.5%–7% (or as advised by a doctor)
Fluctuations occur when glucose levels repeatedly shift outside these ranges.
Who Experiences Blood Sugar Fluctuations Most Often?
Blood sugar instability can occur in anyone with diabetes, but certain groups are more prone:
- Individuals using insulin
- People with long-standing diabetes
- Those with inconsistent meal timings
- Patients with fever, infections, or illness
- Individuals under high stress or poor sleep routines
- Pregnant women with gestational diabetes
- People with thyroid disorders
- Children and adolescents with Type 1 diabetes
Understanding susceptibility helps plan better prevention.
Why Do Blood Sugar Levels Fluctuate?
Blood sugar does not rise or fall without reason. Identifying triggers is the first step to achieving long-term control.
Irregular Eating Patterns
Meal timing plays a crucial role in glucose stability.
Common causes include:
- Skipping meals
- Long gaps between meals
- High-carbohydrate meals (rice, sweets, bakery items)
- Large dinners
- Frequent snacking
- Overeating after periods of fasting
These lead to sudden highs and lows.
Incorrect Medication or Insulin Dosing
Inaccurate medication usage commonly triggers fluctuations.
Common issues:
- Missed doses
- Double doses
- Wrong insulin type
- Incorrect injection timing
- Not rotating injection sites
- Faulty pens or syringes
Stress and Emotional Imbalance
Stress hormones such as cortisol and adrenaline increase glucose levels by causing the liver to release stored sugar.
Triggers include:
- Workload pressure
- Academic stress
- Family issues
- Emotional distress
- Anxiety or depression
Prolonged stress = persistent fluctuations.
Lack of Physical Activity
A sedentary lifestyle reduces insulin sensitivity, leading to sustained high sugar levels. Conversely, intense exercise without proper preparation may cause sudden drops.
Poor Sleep Quality
Sleeping less than 6 hours can cause:
- Morning sugar spikes
- Increased insulin resistance
- Greater appetite and cravings
- Fatigue-induced stress
This contributes significantly to the Dawn Phenomenon, where morning glucose rises due to hormonal influences.
Hormonal Changes
Hormones affect the body’s response to insulin. Fluctuations often occur during:
- Menstruation
- Pregnancy
- PCOS
- Menopause
Illness, Fever, or Infections
During infections like Urinary Tract Infections (UTI), flu, dengue, or pneumonia, the body releases stress hormones that elevate blood sugar.
Effects include:
- High glucose levels
- Insulin resistance
- Dehydration
- Risk of ketone formation (especially in Type 1 diabetes)
Alcohol Consumption
Alcohol affects the liver’s ability to release glucose, causing:
- Delayed hypoglycemia
- Unpredictable glucose readings
- Increased risk of sudden lows
More severe when consumed on an empty stomach.
Dehydration
Low fluid intake concentrates glucose in the blood, leading to higher readings.
Inaccurate Glucose Monitoring
Incorrect readings can misrepresent sugar stability.
Possible causes:
- Expired strips
- Faulty glucometers
- Incorrect finger-prick technique
- Dehydration
- Dirty sensors
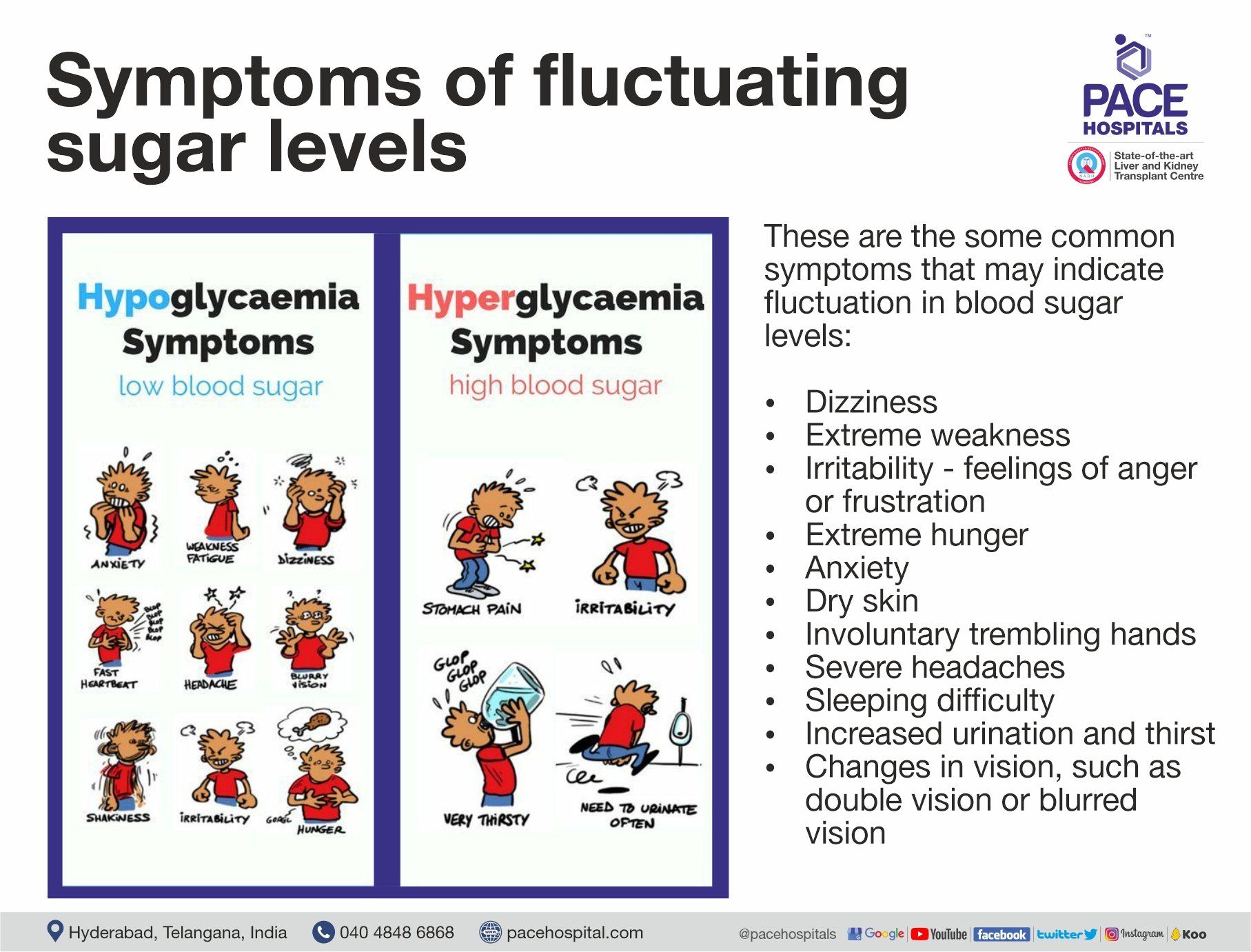
Symptoms of Fluctuating Blood Sugar Levels
Symptoms of Fluctuating Blood Sugar Levels
- Excessive thirst
- Frequent urination
- Fatigue
- Headache
- Blurred vision
- Increased hunger
- Slow-healing wounds
- Dry mouth
Symptoms of Low Blood Sugar (Hypoglycemia)
- Sweating
- Shakiness
- Sudden hunger
- Irritability
- Dizziness
- Rapid heartbeat
- Confusion
- Fainting (severe)
Early recognition prevents complications.
How Are Blood Sugar Fluctuations Diagnosed?
Evaluation includes multiple assessments to understand the cause:
- Self-Monitoring of Blood Glucose (SMBG)
- Checking sugars before and after meals.
- Continuous Glucose Monitoring (CGM)
- Provides real-time data every few minutes.
- HbA1c Test
- Reflects 3-month glucose average.
- Fasting and Post-Prandial Tests
- Identify meal-related fluctuations.
- Kidney, Liver & Thyroid Function Tests
- Detect metabolic or hormonal contributors.
- Lipid Profile
- Identifies cholesterol-related insulin resistance.
- These tests help map sugar patterns and personalise treatment.
How to Manage Fluctuating Blood Sugar Effectively for the Long Term?
Achieving stable glucose levels requires a coordinated approach involving food habits, medication, activity, monitoring, and lifestyle changes.
Follow a Balanced and Regular Meal Schedule
- Do not skip meals
- Eat smaller, frequent portions
- Prefer whole grains over refined foods
- Include protein in every meal
- Add fibre-rich vegetables
- Avoid heavy, late dinners
Low-GI Options:
- Oats
- Millets (jowar, bajra, ragi)
- Brown rice
- Legumes and dals
- Green leafy vegetables
Manage Carbohydrates Sensibly
As carbs affect sugar more than proteins or fats:
- Choose complex carbohydrates
- Spread carb intake evenly
- Avoid sweets and sugary drinks
- Limit bakery products
Maintain Medication and Insulin Accuracy
- Take medicines at consistent times
- Follow correct insulin technique
- Rotate injection sites
- Store insulin properly
Stay Physically Active
Recommended activities include:
- Brisk walking
- Cycling
- Swimming
- Yoga
- Stretching
- Light strength training
Avoid heavy workouts on an empty stomach.
Manage Stress Effectively
Helpful strategies:
- Deep breathing
- Meditation
- Yoga
- Journaling
- Short breaks
Stress management reduces glucose surges.
Improve Sleep Quality
Aim for 7–8 hours daily.
Sleep tips:
- Avoid screens before bed
- Follow a consistent routine
- Limit caffeine
- Keep bedroom dark and cool
Stay Hydrated
Drink 2–2.5 litres of water daily unless medically restricted.
Manage Illness Promptly
During infections:
- Monitor sugars more frequently
- Adjust medications under supervision
- Maintain hydration
Limit Alcohol
Alcohol increases the risk of sudden lows and should be consumed cautiously, if at all.
Use Diabetes Technology & Smart Monitoring
- CGM devices
- Smart glucometers
- Pattern-tracking apps
Technology helps identify trends and prevent extremes.
Do’s and Don’ts for Stable Sugar Levels
Do’s
- Eat on time
- Exercise regularly
- Monitor sugars daily
- Maintain hydration
- Manage stress
- Follow medication as prescribed
Don’ts
- Avoid sugary snacks
- Avoid skipping medication
- Avoid erratic sleep routines
- Avoid overeating carbohydrates
- Avoid ignoring symptoms
How Long Does It Take to Stabilise Blood Sugar?
Timeframes depend on diabetes type, duration, medication, stress, diet, and activity level.
Typical timelines:
- Dietary & lifestyle improvements: 2–4 weeks
- Medication optimisation: 1–2 weeks
- Reduction in spikes & drops: 1–2 weeks
- HbA1c improvement: 8–12 weeks
Most individuals see meaningful improvements within 4–8 weeks.
When to Consult a Doctor
Medical evaluation is needed if:
- Daily fluctuations occur
- Morning spikes persist
- Frequent hypoglycemia is noticed
- Blurred vision develops
- Frequent infections occur
- Wounds heal slowly
- Fatigue or dizziness is persistent
Early evaluation prevents long-term complications.
Diagnostic Tools Used to Investigate Fluctuations
- Continuous glucose monitoring
- HbA1c every 3 months
- Thyroid panel
- Kidney function tests & liver function tests
- Vitamin D & B12 levels
- Urine microalbumin
- ECG for cardiac evaluation
Preventing Blood Sugar Fluctuations in the Long Term
Prevention is based on consistency:
- Regular meals
- Balanced carbohydrates
- Adequate sleep
- Routine exercise
- Stress control
- Hydration
- Medication adherence
- Early treatment of infections
- Regular monitoring
Long-term habits matter more than short-term fixes.
Diabetes Care at PACE Hospitals – Why Patients Trust Us
PACE Hospitals is a leading centre for comprehensive diabetes care, specialising in identifying and managing fluctuating blood sugar levels. The care model is built on precision assessment, personalised treatment, and long-term glucose stability.
Our Strengths Include:
- Experienced
endocrinologists and
diabetes specialists skilled in managing glycemic variability and complex cases.
- Advanced diagnostics including CGM, metabolic profiling, and HbA1c trend analysis.
- Personalised diabetes plans covering nutrition, medication, activity, sleep, and stress management.
- State-of-the-art monitoring technology for accurate glucose pattern tracking.
- Dedicated diabetes educators and nutrition experts for structured lifestyle guidance.
- Integrated complication screening for eye, kidney, nerve, cardiac, and foot health.
- Holistic long-term approach focused on stability, prevention, and metabolic improvement.
- Supportive, patient-centred care ensuring clarity, comfort, and continuous follow-up.
PACE Hospitals is committed to providing safe, structured, and dependable diabetes management for individuals with fluctuating blood sugar levels.
FAQs on Fluctuating Blood Sugar Levels in Diabetes
What are fluctuating blood sugar levels and why do they occur?
Fluctuating blood sugar levels refer to repeated ups and downs in glucose throughout the day. They occur due to factors such as irregular meals, stress, medication errors, infections, hormonal changes, poor sleep, dehydration, or inconsistent physical activity.
Why should blood sugar fluctuations be treated early?
Early management prevents long-term complications including heart disease, kidney damage, nerve problems, vision issues, poor wound healing, and increased infection risk. Stabilising glucose early also improves energy levels, sleep, mood, and overall metabolic health.
Can fluctuating blood sugar levels be managed without medication?
Mild fluctuations may improve with diet control, hydration, sleep regulation, and exercise. However, most cases, especially those involving insulin resistance or long-standing diabetes, require medication adjustments or insulin therapy.
How long does it take to stabilise fluctuating blood sugar?
Initial improvements may be seen within 1–2 weeks after adjusting diet, activity, and medications. Significant stabilisation usually occurs within 4–8 weeks. HbA1c improvement takes around 8–12 weeks.
Who is at higher risk for blood sugar fluctuations?
Fluctuations are more common in people using insulin, those with long-standing diabetes, pregnant women, individuals with thyroid disorders, children with Type 1 diabetes, and individuals with irregular routines or poor sleep patterns.
Can fluctuating blood sugar return after stabilisation?
Yes, if dietary habits, sleep, stress levels, medication routines, or physical activity become inconsistent. Regular follow-ups and structured monitoring help maintain long-term stability.
Does PACE Hospitals manage severe or complex fluctuation cases of blood sugar levels?
Yes. The team has highly experienced endocrinologist and diabetologists to manage highly unstable glucose patterns, insulin resistance, recurrent hypoglycemia, gestational diabetes, and fluctuations caused by hormonal or metabolic disorders.
How long does it take to stabilise fluctuating blood sugar levels?
In general, improvements may begin within 1–2 weeks after diet and medication adjustments. Significant stabilisation typically occurs within 4–8 weeks. HbA1c results reflect changes over 8–12 weeks.
What diagnostic tools are used at PACE Hospitals to assess fluctuating blood sugar?
Common assessments include:
- Continuous Glucose Monitoring (CGM)
- HbA1c evaluation
- Fasting and post-meal blood sugar monitoring
- Thyroid, kidney, and liver function tests
- Lipid profile
These help identify patterns, triggers, and underlying metabolic issues.
Can fluctuating sugars be controlled with diet alone?
Diet plays a major role, but many individuals require medication optimisation, physical activity, stress reduction, adequate sleep, and hydration. A combined approach achieves the best long-term outcomes.
Can fluctuating blood sugar affect long-term health?
Yes. Persistent instability increases the risk of cardiovascular disease, kidney dysfunction, neuropathy, vision problems, infections, and slow wound healing. Early management reduces these risks significantly.
Is stabilising blood sugar a one-time process?
No. It requires continuous monitoring, consistent meals, regular physical activity, correct medication use, and ongoing follow-ups. Long-term stability depends on routine and lifestyle consistency.
Why is accurate glucose monitoring important?
Incorrect readings can lead to wrong medication adjustments. PACE Hospitals recommends validated glucometers or CGM devices to ensure accurate pattern detection and safe insulin or medication titration.
What makes PACE Hospitals a leading centre for diabetes and blood sugar fluctuation management?
- Experienced endocrinologists
- Advanced diagnostic tools including CGM
- Personalised diabetes management plans
- Dedicated diabetes educators and nutrition experts
- Modern glucose monitoring technologies
- Integrated complication screening
- Holistic approach focused on long-term metabolic stability
How does PACE Hospitals help minimise complications and achieve long-term stability for blood sugar levels in diabetes?
Through comprehensive care including:
- Optimised treatment plans
- CGM-based decision making
- Nutrition and lifestyle counselling
- Early detection of associated conditions
- Preventive screening for eyes, kidneys, nerves, heart, and feet
- This approach ensures safer long-term outcomes and reduced sugar variability.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868