Premenstrual syndrome (PMS): Causes, Risk factors, Symptoms, Treatment and Prevention
Premenstrual Syndrome Definition
Premenstrual syndrome is a
menstrual disorder that involves physical and emotional symptoms occurring one to two weeks before menstruation during the luteal phase of the menstrual cycle. Most women experience PMS, with symptoms typically ending when menstruation starts.
Premenstrual Syndrome (PMS) meaning
- The term "menstrual" originated from the old French word "menstruel," which is derived from the Latin word "menstrualis" It refers to monthly cycles, related to females.
- The Latin root "menstruus" means monthly occurrences and is linked to the word "mensis," which means "month."
Days back in 1865, the meaning of premenstrual was before menstrual. In 1928, it was referred to as premenstrual tension syndrome; the term premenstrual syndrome (PMS) emerged in 1971.
Prevalence of Premenstrual Syndrome
The prevalence of reproductive-age women affected with PMS worldwide amounts to 47.8%. Among these, 20% of women experience severe symptoms which disrupt their daily activities, and the others have mild to moderate symptoms.
Prevalence of Premenstrual Syndrome in India
As per some studies in India, a wide range of prevalence estimates for premenstrual syndrome (PMS) has been reported, ranging from 14.3% to 74.4%.
Premenstrual Syndrome Causes
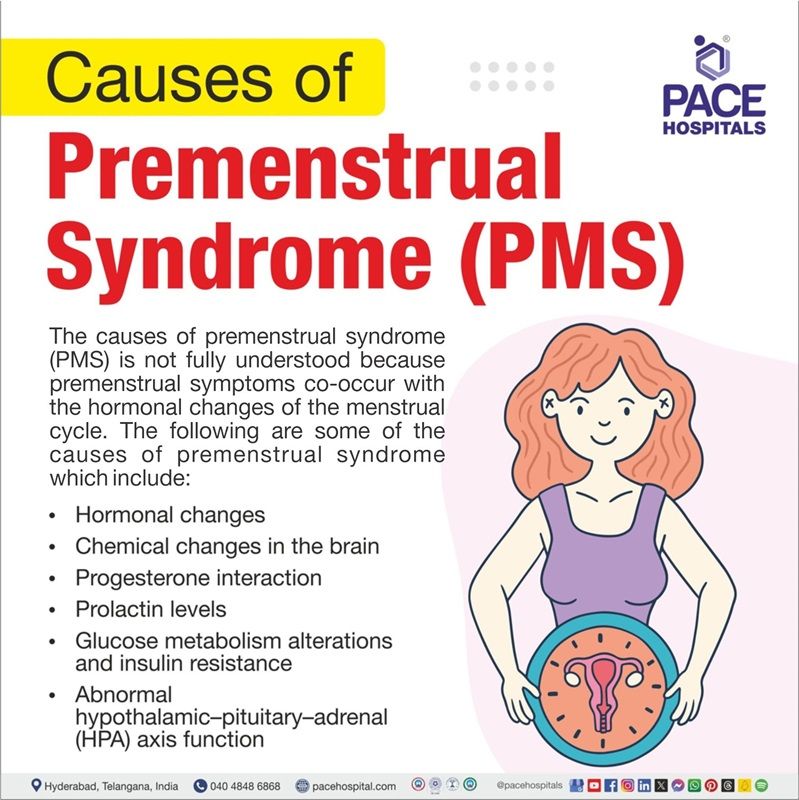
The causes of premenstrual syndrome (PMS) are not fully understood because premenstrual symptoms co-occur with the hormonal changes of the menstrual cycle. The following are some of the causes of premenstrual syndrome which include:
- Hormonal changes: Hormonal changes like excess oestrogen, progesterone deficiency and fluctuation of oestrogen levels during the luteal phase are responsible for mood changes leading to premenstrual syndrome.
- Chemical changes in the brain: Serotonin is a neurotransmitter and an etiological factor that regulates mood. Symptoms of PMS are linked to serotonin levels. The substances the body uses to produce serotonin are known as Serotonin precursors, and they increase significantly between 7 to 11 days and 17 to 19 days of the menstrual cycle causing PMS.
- Hence, PMS is closely related to mood disorders through the regulation of oestrogen-serotonin levels.
- Progesterone interaction: It is believed that the interaction of progesterone with neurotransmitters is influenced by PMS. Preexisting serotonin deficiency combined with high levels of progesterone plays a role in the development of PMS.
- Prolactin levels: High prolactin levels are linked with low levels of oestrogen, which may cause symptoms such as depression. The association of High prolactin levels with low levels of progesterone may cause symptoms such as anxiety or irritability.
- Glucose metabolism alterations and insulin resistance: Lower blood glucose levels and insulin resistance were found after ovulation or during the luteal phases of the menstrual cycle. Hence, hypoglycaemia is a stimulating factor of PMS symptoms .
- Abnormal hypothalamic–pituitary–adrenal (HPA) axis function: The HPA axis controls various physiological processes and stress responses, including the production of hormones. HPA axis abnormalities are a factor linked to premenstrual syndrome (PMS), particularly the hormonal fluctuations that occur during the menstrual cycle.
Risk factors of Premenstrual Syndrome
Risk factors of PMS are essential to help individuals and healthcare providers identify those who are more susceptible to experience severe symptoms. Here are some common risk factors:
- Being obese: Women with a higher BMI have a greater chance of developing severe PMS compared to women with normal BMI. A possible reason for the relationship between PMS and BMI is the lower level of oestradiol in women with higher body weight.
- Age: Premenstrual syndrome (PMS) commonly affects women of childbearing age, and symptoms often begin in the late 20s to early 30s.
- Stress: Experiencing high levels of stress can trigger symptoms of premenstrual syndrome (PMS) and disrupt the delicate hormone balance in the body, potentially contributing to the onset of PMS.
- Sedentary lifestyle: A sedentary lifestyle or low physical activity levels can contribute to hormonal imbalances, including disruptions in oestrogen and progesterone levels. These fluctuations play a significant role in the onset and severity of PMS symptoms.
- Improper diet: Dietary choices, such as consuming high amounts of caffeine, sugar, or alcohol, can exacerbate PMS symptoms. A diet lacking vitamins and minerals, especially calcium and magnesium, can also increase the risk of PMS.
- Smoking: Smoking impacts on hormonal balance and circulation. It increases the risk and severity of PMS symptoms.
- Mental health: Individuals experiencing severe PMS symptoms may also have conditions such as depression, anxiety, and other mental health disorders, as fluctuations in hormones, particularly progesterone, can affect neurotransmitters such as serotonin, which play a role in regulating mood.
- Family history: Women with a family history of PMS or mood disorders are more likely to experience symptoms indicating a potential genetic component.
Premenstrual Syndrome Symptoms
Premenstrual syndrome (PMS) symptoms include both emotional and physical symptoms that can impact the quality of life. It's important to remember that symptoms usually stop during or at the beginning of the menstrual period. This means there is at least one symptom-free week before symptoms start returning, and the premenstrual syndrome symptoms include:
PMS Physical symptoms
- Breast tenderness or swelling
- Abdominal bloating
- Acne
- Diarrhoea and constipation
- Fluid retention
- Weight gain
PMS Emotional symptoms
- Irritability
- Anxiety
- Low mood
- Trouble with concentration and memory
Complications Of Premenstrual Syndrome
Complications of premenstrual syndrome affect women’s daily life and overall well-being. Some of these complications include:
- Relationship problems: Untreated PMS can affect sexual life, which can lead to sexual distress and relationship problems.
- Psychological issues: PMS can cause mood swings, irritability, anxiety, and depression, which can lead to psychological issues.
- Absenteeism in the workplace: Poor menstrual hygiene management can results in feelings of shame, anxiety, and embarrassment that contribute to absenteeism and poor performance.
Premenstrual Syndrome Diagnosis
There is no single method for diagnosing premenstrual syndrome. A gynaecologist confirms it based on three key elements:
- The symptoms must match those of PMS.
- The symptoms must occur only during the luteal phase of the menstrual cycle.
- The symptoms must negatively impact the patient's daily function and lifestyle.
Once a physician is suspicious of the diagnosis, patients are advised to keep a diary of premenstrual symptoms that includes.
- Calendar of premenstrual experiences (COPE): Among other things, it is the most valid and reliable tool for diagnosing PMS. However, these methods require immense time and effort since patients must report their symptoms daily for at least two menstrual cycles.
- Daily record of severity of problems (DRSP)
Laboratory diagnostic testing is not necessary, but it can be used as a complementary tool. For example:
- Blood count: This blood count can be recommended to check for anaemia.
- Thyroid function tests: These tests can help detect hypothyroidism and hyperthyroidism.
Premenstrual Syndrome Treatments
The main intention of PMS treatment is to relieve symptoms and reduce its effects on daily routine activities. Recent research has suggested that there are superior benefits of combination therapies they include:
- Pharmacological management
- Selective serotonin reuptake inhibitors
- Combined oral contraceptives
- Gonadotropin-releasing hormone
- Diuretics
- Nonpharmacological management
- Cognitive-behavioural therapy
- Complementary therapies
- Dietary supplements
Pharmacological Management
The pharmacological approach of treating premenstrual syndrome includes drugs as mentioned below:
- Selective serotonin reuptake inhibitors: SSRIs can be used as the first-line therapy. These are preferred due to their rapid onset of effect. They can be administered continuously or cyclically during the luteal phase to alleviate symptoms effectively.
- Combined oral contraceptives: COCs are less effective in treating the affective symptoms of PMS compared with SSRIs.
- Gonadotropin-releasing hormone: GnRH agonists rarely treat severe PMS. These medications interfere with the balance of hormones in the body, significantly reducing the production of hormones in the ovaries.
- Diuretics: Diuretics, also called water pills, may reduce symptoms of bloating and breast tenderness.
Nonpharmacological Management
Nonpharmacological has been proven beneficial for treating premenstrual symptoms. Hence, here are some of the therapies that include:
- Cognitive-behavioural therapy: CBT focuses on correcting disruptive thoughts, behaviours, and emotions.
- Complementary therapies: Complementary therapies may help with PMS, but there's not much evidence that they work. Some of the therapies include:
- Acupuncture
- Reflexology
- Dietary supplements: Dietary supplements may help with PMS, but there's not much evidence. The following are some of the supplements that can be helpful in reducing the symptom of PMS, such as
- Vitamin B6
- Calcium
- Vitamin D
- Magnesium
Premenstrual Syndrome Prevention
Prevention of PMS (Premenstrual Syndrome) focuses on reducing the symptoms and improving the quality of life. Here are some strategies that can help to prevent PMS symptoms:
- Exercising regularly: Daily physical activity can help balance hormone levels and improve mood, potentially reducing some PMS symptoms
- Maintaining a healthy diet: Maintaining a healthy, balanced diet and eating small meals every two to three hours can help manage weight.
- Managing stress: It's important to get enough sleep and manage stress through activities like yoga to reduce symptoms.
- Taking painkillers: When needed, taking painkillers (prescribed by healthcare professional) can help in managing cramps during PMS.
- Tracking PMS symptoms: Keeping a symptom diary for at least two menstrual cycles can help to track the changes that occur throughout the menstrual cycle and to identify any abnormalities.
- Avoiding excessive consumption of alcohol: Avoiding the consumption of alcohol and caffeine for at least two weeks before periods can help in managing symptoms.
Difference between PMS and Pregnancy symptoms
PMS symptoms vs Pregnancy symptoms
Premenstrual syndrome (PMS) and pregnancy symptoms can have many similarities, but some symptoms are more likely to indicate pregnancy:
| Symptoms | PMS | Pregnancy |
|---|---|---|
| Breast pain | PMS breast pain can feel heavy and dull and may reduce during or after period. | Pregnancy breast pain can feel sore, tender, or sensitive and can start one to two weeks after conception . |
| Bloating | PMS bloating is caused by water retention and hormonal changes and goes away after period. | Pregnancy bloating can last longer and is caused by hormonal changes that increase uterine blood flow . |
| Nausea | High levels of prostaglandins usually cause PMS nausea | Pregnancy nausea usually occurs before six weeks of pregnancy. |
| Mood swings | PMS mood swings typically occur two weeks after ovulation. | Pregnancy mood swings can occur throughout the entire pregnancy. |
| Abdominal pain | PMS pain typically starts two days before period or 13 days after ovulation. | Pregnancy-related discomfort can begin with implantation, causing a pinching sensation. |
Frequently Asked Questions (FAQs) on PMS
Can lifestyle factors like exercise and diet affect PMS symptoms?
Yes, sticking to a healthy lifestyle that includes regular physical activity, a well-rounded diet, sufficient sleep, and stress-reducing methods can assist in reducing PMS symptoms for some people .
What is the first line treatment for premenstrual syndrome?
Currently, selective serotonin reuptake inhibitors (SSRIs) are commonly considered the most suitable initial therapy for premenstrual disorders, especially where psychological or behavioural symptoms are prominent.
What is premenstrual dysphoric syndrome?
Premenstrual dysphoric disorder (PMDD) is the serious form of PMS. The symptoms of PMDD are considered as severe PMS symptoms and can significantly disrupt daily life. PMDD is less common than PMS.
Is it possible to have PMS after your period?
PMS symptoms often occur days or weeks before menstruation due to changes in hormone levels. However, PMS cannot occur after menstrual periods because hormone levels start to rise again after periods.
Can PMS symptoms change from month to month?
The severity of premenstrual syndrome (PMS) can vary significantly from person to person, month to month, and change over the years. However, it is not possible to predict how PMS will develop over time. The sure thing is that it will stop after menopause.
What is premenstrual syndrome?
Premenstrual syndrome (PMS) refers to the emotional and physical symptoms that some women experience before menstruation, impacting their quality of life. These symptoms typically resolve during or at the beginning of the menstrual period.
Can PMS symptoms impact academic or work performance?
Yes, symptoms such as fatigue, difficulty concentrating, or mood swings can affect academic or work performance. It's important to manage symptoms effectively.
Is there a connection between PMS and mental health conditions like anxiety or depression?
Some individuals with PMS may experience worsened symptoms of anxiety or depression during the premenstrual phase because fluctuations in hormones, particularly progesterone, can affect neurotransmitters such as serotonin, which play a role in regulating mood and anxiety. Hence, it's essential to discuss any mental health concerns with a healthcare provider for appropriate management.
When do PMS symptoms typically occur?
Symptoms of PMS usually start after ovulation or during the luteal phase of the menses and diminish shortly after menstruation begins. Symptoms may vary in severity and duration among individuals.
Is PMS the same for every person?
No, PMS symptoms can vary widely among individuals regarding type, severity, and duration. Factors such as hormone sensitivity, overall health, and lifestyle habits can influence how PMS affects each person.
Why are PMS symptoms getting worse?
As women approach their late 30s or 40s and transition to menopause, known as perimenopause, they may experience serious PMS symptoms. This is particularly common among women whose emotional well-being is affected by fluctuating hormone levels throughout the menstrual cycle.
Is PMS treatable?
Yes, PMS can be treatable, a gynaecologist may recommend therapies and lifestyle changes. These may include cognitive behavioural therapy and hormonal medicine, such as the combined contraceptive pill.
What is the diagnostic test of PMS?
Physicians do not have specific tests for diagnosing PMS. The diagnosis is often based on the patient's symptoms and medical background. It is recommended to track symptoms for at least two menstrual cycles and then share any observed patterns.
Related articles
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868