Guillain-Barré Syndrome: Types, Causes, Risk Factors, Symptoms, Diagnosis & Treatment
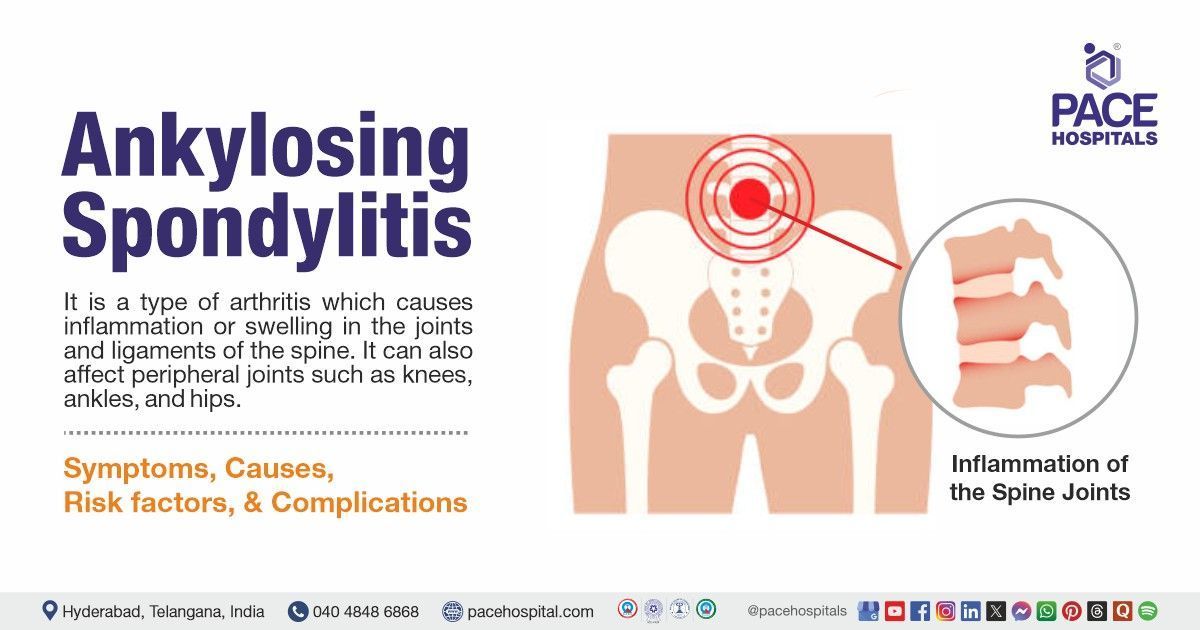
What is Guillain-Barré syndrome?
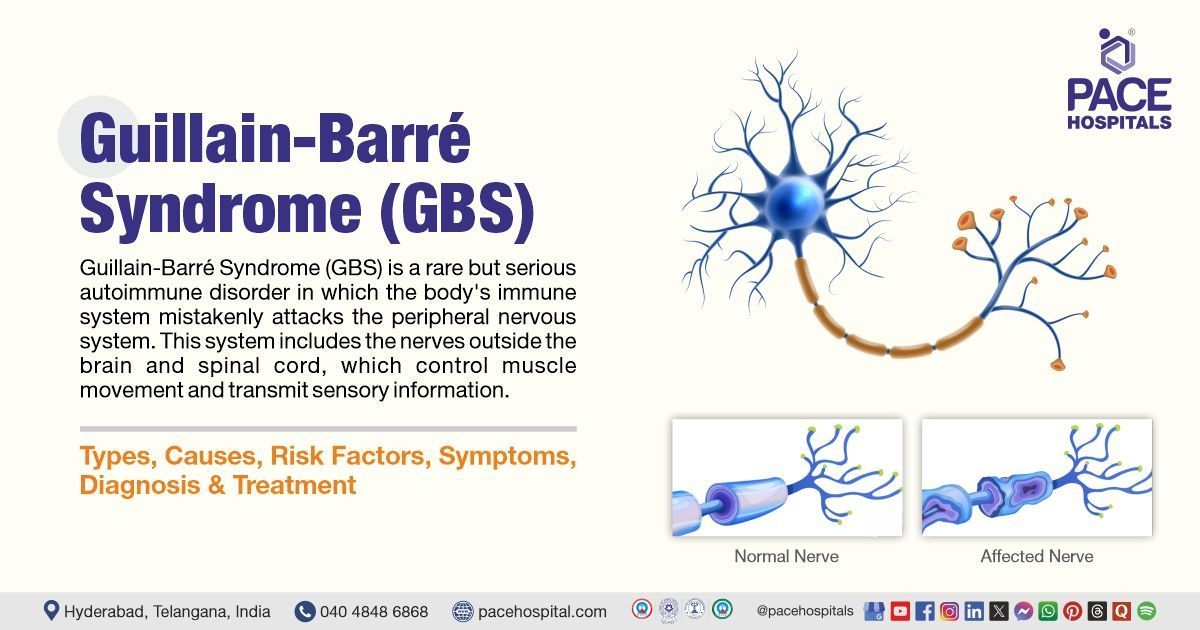
Guillain-Barré syndrome (GBS) is a rare but serious autoimmune disorder in which the body's immune system mistakenly attacks the peripheral nervous system.
This condition is commonly triggered by infectious agents of Guillain-Barré syndrome, such as Campylobacter jejuni, Cytomegalovirus (CMV), Epstein-Barr virus (EBV), Zika virus, and COVID-19. It can also occur after vaccination or surgical procedures in rare cases.
The immune system's attack damages the myelin sheath (the protective covering of nerves) or the axons (the nerve fibers themselves), leading to muscle weakness, numbness, and, in severe cases, paralysis. Guillain-Barré syndrome can affect people of all ages, but it is more common in adults and males. Early diagnosis and treatment are crucial to prevent complications and improve outcomes.
Guillain-Barré syndrome is considered a medical emergency because it can progress rapidly, leading to life-threatening complications such as respiratory failure. However, with prompt treatment, most patients recover fully or with minimal effects.
A neurologist is a specialist who treats Guillain-Barré syndrome (GBS). Guillain-Barré syndrome is a medical emergency that usually requires hospitalization.
Guillain-Barré syndrome meaning
The term "Guillain-Barré syndrome" is named after the French neurologists Georges Guillain and Jean Alexandre Barré, who, along with André Strohl, first described the condition in 1916. They identified the characteristic symptoms and the link between the syndrome and elevated protein levels in cerebrospinal fluid. Guillain-Barré syndrome is also known as acute inflammatory demyelinating polyneuropathy (AIDP), which refers to inflammation and damage to the myelin sheath of peripheral nerves.
Prevalence of Guillain-Barré syndrome
Incidence and prevalence of Guillain-Barré syndrome worldwide
Globally, the incidence of Guillain-Barré syndrome (GBS) is estimated to be between 1 and 2 cases per 100,000 people per year, which means it affects approximately 1-2 people out of 100,000 people each year.
Epidemiology of Guillain-Barré syndrome in Indian population
The reported incidence of Guillain-Barré syndrome in India varies, with estimates ranging from 1-2 cases per 100,000 people annually. A study conducted at major teaching hospitals found that approximately 138 cases are diagnosed each year. Another retrospective study from Rajasthan indicated a prevalence of 41.5% among cases of acute flaccid paralysis recorded between 2012 and 2015. There was a considerable male predominance (68.5%).

Types of Guillain-Barré syndrome
Guillain-Barré syndrome is classified into several subtypes based on the specific part of the nervous system affected and the progression of symptoms. The main types include:
- Acute inflammatory demyelinating polyneuropathy (AIDP): This is the most common form of Guillain-Barré syndrome, accounting for about 85–90% of cases in western countries. It is characterized by damage to the myelin sheath of peripheral nerves, leading to muscle weakness and sensory disturbances.
- Miller fisher syndrome (MFS): A rare variant of Guillain-Barré syndrome that primarily affects the cranial nerves, leading to symptoms like double vision, difficulty swallowing, and poor coordination. MFS is more common in Asia and is often associated with antibodies against a specific nerve component called GQ1b.
- Acute motor axonal neuropathy (AMAN): This type involves damage to the axons of motor nerves, leading to severe muscle weakness without significant sensory loss. AMAN is more common in children and young adults, particularly in rural areas of China and Mexico.
- Acute motor-sensory axonal neuropathy (AMSAN): A more severe form of Guillain-Barré syndrome that affects both motor and sensory nerves. AMSAN is less common but has a poorer prognosis due to extensive nerve damage.
- Acute panautonomic neuropathy: Acute panautonomic neuropathy, the rarest Guillain-Barré syndrome variant, involves sympathetic and parasympathetic nervous systems. Patients may have severe postural hypotension, bowel and bladder retention, decreased salivation and lacrimation, and pupillary abnormalities. Cardiovascular involvement is common, and dysrhythmias are a significant source of mortality. Recovery is gradual and often incomplete.
- Pure sensory GBS: It is characterized by a symmetrical and extensive pattern of rapid onset sensory loss, sensory ataxia, and areflexia. The results of EMG tests reveal distinctive indications of a demyelinating process in the peripheral nerves, and lumbar puncture examinations reveal albumin cytologic separation in the Cerebro spinal fluid (CSF).
- Pharyngeal-cervical-brachial variant: Weaknesses are limited to facial, oropharyngeal, cervical, and upper limb areas without lower limb involvement.
Symptoms of Guillain-Barré syndrome
Guillain-Barré syndrome symptoms often develop rapidly and can progress over days or weeks. The most common Guillain-Barré syndrome signs and symptoms include:
- Muscle weakness and Tingling: Often begins in the feet and legs, spreading to the arms and upper body.
- Paresthesia: Sensations such as "pins and needles," tingling, or numbness in hands and feet.
- Pain: Sharp, shooting pain often occurs in the legs or back, which may worsen at night.
- Coordination problems: Unsteadiness or difficulty walking due to muscle weakness.
- Facial symptoms: Drooping face muscles, trouble swallowing (dysphagia), speaking (dysarthria), or chewing; double vision; difficulty moving eyes.
- Respiratory issues: Difficulty breathing if chest muscles are affected; may require intensive care support.
- Autonomic dysfunction: Abnormal heart rate or blood pressure fluctuations; bladder control issues may occur in severe cases.
The progression of symptoms typically peaks within 2–4 weeks, after which patients enter a plateau phase before recovery begins. Recovery can take weeks to months, and some patients may experience long-term residual effects.
Guillain-Barré syndrome in children symptoms
In children, Guillain-Barré syndrome often begins with weakness in the lower limbs, which can spread to the upper body. A common sign is the loss of reflexes, making it harder for health care experts to detect them. Many children experience neuropathic pain, which can be quite distressing. Younger kids might refuse to walk due to pain or weakness in their legs.
Some may also have trouble with facial movements or swallowing because of cranial nerve involvement. Additionally, children with GBS might experience fluctuations in blood pressure and other autonomic issues. Sensory disturbances like numbness or tingling are also common. These symptoms can vary widely among children, and some might show unusual signs like uneven weakness or predominant sensory problems.
Early symptoms of Guillain-Barré syndrome
The initial symptoms of Guillain-Barré syndrome (GBS) include weakness in the limbs and tingling. These symptoms may spread to the arms and upper body.
Guillain-Barré syndrome causes
Guillain-Barré Syndrome (GBS) is not inherited, but it is linked to various infections, illnesses, and traumas. The exact cause remains unknown. It's believed that certain illnesses might alter nerve cells, causing the immune system to mistakenly view them as threats. In some cases, the immune system seems to lose its ability to distinguish between harmful invaders and the body's own cells.
When GBS occurs, the immune system starts attacking the nerves. In the most common form of GBS, known as Acute inflammatory demyelinating polyneuropathy (AIDP), the protective covering of the nerves (myelin sheath) is damaged. Sometimes, the nerve's core (axon) is also affected. This damage disrupts the nerve signals between the brain and muscles, leading to muscle weakness and abnormal sensations. As a result, muscles cannot respond properly to brain commands, and the brain receives distorted sensory information from the affected areas.
Risk Factors for Guillain-Barré syndrome
Guillain-Barré syndrome is a complex condition where the immune system mistakenly attacks nerves. Identifying its triggers and risk factors is crucial for developing effective treatment strategies and improving patient outcomes in this challenging neurological disorder.
Certain factors may increase the risk of developing Guillain-Barré syndrome, including:
- Age
- Gender
- Recent infection
- Chronic illness
- Surgery or Trauma
- Vaccinations
- Other factors
Age: Older adults above the age of 50 years old have a higher risk of Guillain-Barré syndrome due to age-related immune system changes, making them more susceptible to autoimmune responses that attack peripheral nerves.
Gender: Men are slightly more likely to develop Guillain-Barré syndrome than women, possibly due to hormonal or genetic differences that influence immune system behavior and nerve vulnerability.
Recent infection: Bacterial (e.g., Campylobacter jejuni) or viral (e.g., flu, Zika) infections can trigger Guillain-Barré syndrome by causing the immune system to mistakenly attack nerve cells.
Chronic illnesses: Conditions like lupus or HIV weaken the immune system or cause chronic inflammation, increasing the likelihood of autoimmune reactions that lead to Guillain-Barré syndrome.
Surgery or Trauma: Recent surgeries or injuries can stress the immune system, potentially triggering an abnormal immune response that damages peripheral nerves and leads to Guillain-Barré syndrome.
Vaccinations: While rare, certain vaccines, such as the influenza vaccine and some COVID-19 vaccines have been associated with a slight increase in GBS risk.
Other factors: Trauma, certain medical conditions like Hodgkin's lymphoma, and exposure to other pathogens like Mycoplasma pneumoniae and hepatitis viruses have also been linked to GBS.
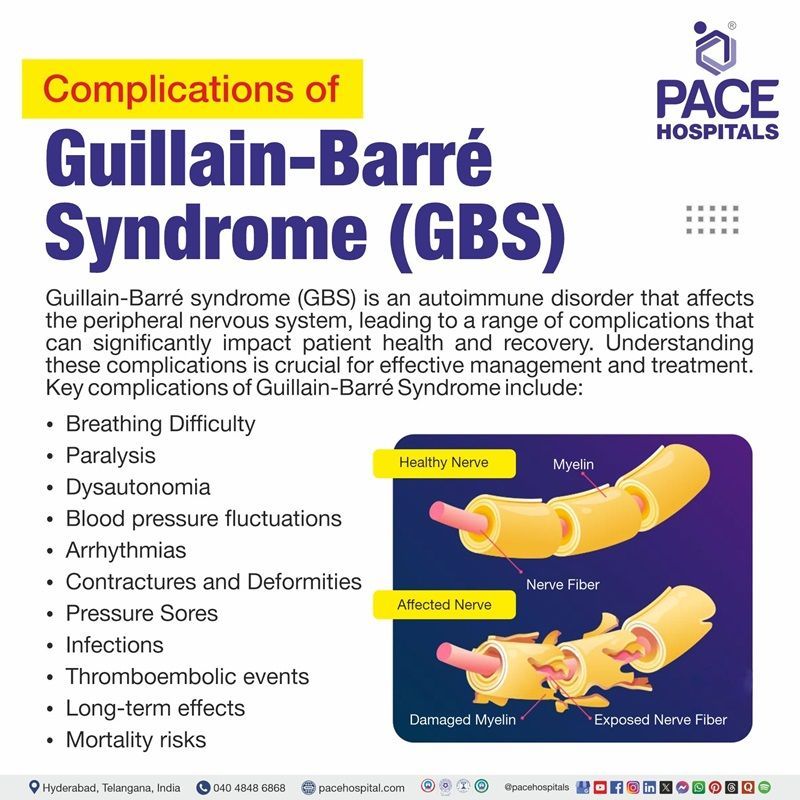
Guillain-Barré syndrome complications
While many people are fortunate enough to make a full recovery from Guillain-Barré syndrome, others face a more challenging journey. For them, GBS can lead to serious complications that profoundly affect their quality of life and even survival. These complications often stem from extensive damage to the nerves, which can disrupt the body's ability to perform its most basic yet vital functions.
Key complications of Guillain barre syndrome include:
- Breathing difficulty
- Paralysis
- Dysautonomia
- Blood pressure fluctuations
- Arrhythmias
- Contractures and Deformities
- Pressure sores
- Infections
- Thromboembolic events
- Long-term effects
- Mortality risks
Breathing difficulty: Approximately 22% of patients may require mechanical ventilation due to respiratory muscle weakness, particularly in the early stages of disease. Severe cases can lead to respiratory failure, which is life-threatening.
Paralysis: Many patients experience varying degrees of paralysis, which can be temporary or, in rare cases, permanent.
Dysautonomia: This condition affects autonomic functions like heart rate and blood pressure, leading to instability and potentially life-threatening complications.
Blood pressure fluctuations: Patients often experience low or unstable blood pressure, which can complicate their clinical management.
Arrhythmias: Cardiac irregularities are common and can increase mortality risk, particularly in older patients.
Contractures and Deformities: Prolonged immobility can lead to shortening of tissues in the joints (contractures), causing deformities over time.
Pressure sores: Patients are at risk of developing bedsores due to extended periods of inactivity.
Infections: Patients with GBS are more susceptible to infections such as pneumonia and urinary tract infections due to reduced mobility and respiratory function.
Thromboembolic events: GBS increases the risk of deep vein thrombosis (DVT), necessitating preventive measures like blood thinners and compression stockings.
Long-term effects: While many individuals recover fully, about 15-30% may experience persistent weakness or other neurological deficits long after the initial episode.
Mortality risks: The overall mortality rate ranges from 2% to 12%, with higher rates in older populations due to complications such as sepsis or acute respiratory distress syndrome (ARDS).
Guillain-Barré syndrome diagnosis
Diagnosing Guillain-Barré syndrome (GBS) can be a deeply concerning experience for patients, as symptoms like weakness or tingling often appear suddenly and progress quickly. Health care experts carefully listen to the patient’s history and perform detailed exams to provide clarity and guide the next steps toward care.
Guillain-Barré syndrome diagnosis criteria include:
Medical history and Physical examination
- Assessing symptoms, reflexes, and muscle strength.
Lumbar puncture (Spinal tap)
- To analyze cerebrospinal fluid for elevated protein levels.
Electromyography (EMG)
- To evaluate nerve and muscle function.
Nerve conduction studies (NCS)
- To measure the speed of nerve signals.
Blood tests
- To rule out other conditions or infections.
Imaging tests
- Magnetic resonance imaging (MRI) of the spine may show nerve root enhancement, supporting the diagnosis of Guillain-Barré syndrome.
Guillain-Barré syndrome treatment
While there is no cure for Guillain-Barré syndrome, early treatment can significantly improve outcomes. Guillain-Barré syndrome is usually treated in a hospital, generally in the intensive care unit, where the patient can be constantly watched 24 hours a day, seven days a week, and intensive nursing, respiratory support, and other required services are readily available.
The recommendations for treating and taking care for patients with Guillain-Barré syndrome are as follows:
- Intravenous immunoglobulin (IVIG)
- A therapy that uses antibodies to reduce the immune system's attack on nerves.
- Plasma exchange (Plasmapheresis)
- A procedure to remove harmful antibodies from the blood.
- Supportive care
- Physical therapy to maintain muscle strength and mobility.
- Mechanical ventilation for patients with respiratory failure.
- Pain management with medications.
- Medications to prevent blood clots.
- Long-term rehabilitation
- Occupational therapy and counseling help patients regain independence and cope with emotional challenges.
Prevention of Guillain-Barré syndrome
Preventing Guillain-Barré syndrome (GBS) is challenging due to its complex autoimmune nature. Since Guillain barre syndrome is often triggered by infections, preventive measures include:
- Practicing good hygiene: To reduce the risk of bacterial and viral infections.
- Staying updated on vaccinations: Staying up to date on vaccines (e.g., flu vaccine) to prevent infections that may trigger GBS.
- Early treatment of infections: Promptly treating infections to reduce the risk of complications.
- Avoiding contaminated food and water: To prevent infections like Campylobacter jejuni.
- Prompt treatment of infections: Early medical intervention helps prevent complications from infections that might trigger GBS.
Difference between Guillain-Barré syndrome and Transverse myelitis
Guillain-Barré syndrome vs transverse myelitis
Guillain-Barré syndrome (GBS) and Transverse myelitis (TM) are both neurological disorders that can cause weakness and paralysis, although they have different causes, symptoms, and areas of involvement. The six significant differences between these two circumstances are listed below.
| Aspect | Guillain-Barré syndrome | Transverse myelitis |
|---|---|---|
| Primary Affected Area | Affects the peripheral nervous system (nerves outside the brain and spinal cord). | Affects the spinal cord (part of the central nervous system). |
| Pattern of Paralysis | Ascending paralysis, often starting from the feet and legs, moving upward. | Symmetrical weakness at the level of the spinal cord, usually affecting both sides of the body. |
| Cause/Triggers | Often triggered by infections like respiratory or gastrointestinal viruses or bacteria. | Triggered by inflammation of the spinal cord, often due to infections, autoimmune conditions, or vaccinations. |
| Immune System Involvement | The immune system attacks the peripheral nerves, often damaging the myelin. | Inflammation in the spinal cord often damages the myelin, affecting nerve function. |
| Diagnosis | Diagnosed with nerve conduction studies, lumbar puncture, and clinical evaluation. | Diagnosed primarily with MRI of the spine and lumbar puncture. |
| Prognosis | Recovery can take months to years, with a high rate of recovery, but severe cases may result in permanent disability. | Recovery varies, but some individuals experience long-term paralysis or deficits, while others may improve significantly. |
Frequently Asked Questions (FAQs) on Guillain-Barré syndrome
What virus causes Guillain-Barré syndrome?
The most common viral cause of Guillain-Barré syndrome is the campylobacter jejuni infection, which often precedes GBS. Other viral infections associated with GBS include cytomegalovirus (CMV), Epstein-Barr virus (EBV), and Zika virus, which can trigger an autoimmune response leading to nerve damage.
What causes Guillain-Barré syndrome in children?
Guillain-Barré syndrome (GBS) in children is an autoimmune disorder where the body's immune system mistakenly attacks the peripheral nervous system. The exact cause of GBS is not fully understood, but it often follows a viral or bacterial infection, surgery, injury, or rarely, a reaction to vaccination.
Can the swine flu vaccine cause Guillain-Barré syndrome?
The swine flu vaccine was linked to an increased incidence of Guillain-Barré syndrome during the 1976 vaccination campaign. However, subsequent studies indicate that modern vaccines pose a much lower risk of triggering Guillain-Barré syndrome.
Can Guillain-Barré syndrome be passed on to others?
No. Guillain-Barré syndrome cannot be passed from one person to another. It is an autoimmune disorder triggered by infections or other factors that lead to nerve inflammation.
Can Guillain-Barré syndrome affect fertility?
Guillain-Barré syndrome does not directly affect fertility. However, complications related to severe cases or prolonged recovery may impact reproductive health. Women who have experienced GBS should consult their healthcare expert regarding pregnancy planning.
Why are corticosteroids contraindicated in Guillain-Barré syndrome?
Corticosteroids are contraindicated in Guillain-Barré syndrome (GBS) because they may interfere with the natural recovery process and potentially worsen outcomes. Studies have shown that corticosteroids do not improve functional recovery and may delay the onset of effective treatments like intravenous immunoglobulin (IVIg) or plasmapheresis, which are more beneficial for patients.
When was Guillain-Barré syndrome first discovered?
Guillain-Barré syndrome was first described in 1916 by French neurologists Georges Guillain and Jean Alexandre Barré. Their initial observations focused on the clinical features of the syndrome, which have since been expanded upon through extensive research into its pathophysiology and treatment.
What vaccines can cause Guillain-Barré syndrome?
Vaccines that have been associated with Guillain-Barré syndrome include the 1976 swine flu vaccine and, to a lesser extent, the seasonal influenza vaccine. Current vaccines are monitored for safety, and the risk of developing GBS remains very low in comparison to the benefits of vaccination.
Do Guillain-Barré syndrome patients have normal deliveries?
Patients with Guillain-Barré syndrome can have normal deliveries, although individual circumstances may vary based on the severity of their condition and overall health during pregnancy. Close monitoring by healthcare expert is essential.
In Guillain-Barré syndrome, cranial nerves affected may include those responsible for facial movements (facial nerve), eye movements (oculomotor, trochlear, abducens nerves), and swallowing (glossopharyngeal and vagus nerves). The extent of cranial nerve involvement varies among patients.
The bacteria most commonly associated with triggering Guillain-Barré syndrome is campylobacter jejuni, which is known to cause gastrointestinal infections. Other bacterial infections can also precede GBS but are less frequently implicated.
Is Guillain-Barré syndrome hereditary?
Guillain-Barré syndrome is not considered hereditary; it is primarily an autoimmune disorder triggered by infections or other environmental factors. Genetic predisposition may play a role in susceptibility, but there is no direct inheritance pattern.
Is Guillain-Barré syndrome an autoimmune disease?
Yes, Guillain-Barré syndrome is classified as an autoimmune disease. In this condition, the immune system mistakenly attacks peripheral nerves, leading to inflammation and damage that results in muscle weakness and paralysis.
Can a blood test detect Guillain-Barré syndrome?
There is no specific blood test for diagnosing Guillain-Barré syndrome. Diagnosis is primarily based on clinical evaluation, patient history, and tests such as lumbar puncture for cerebrospinal fluid analysis or electromyography (EMG) for nerve function assessment.
What is the main cause of Guillain-Barre syndrome?
The main cause of Guillain-Barré syndrome is believed to be an autoimmune response triggered by preceding infections, particularly those caused by Campylobacter jejuni. This immune response leads to damage of peripheral nerves.
What are the three stages of Guillain-Barre syndrome?
The three stages of Guillain-Barré syndrome include:
- Acute phase: Rapid onset of symptoms from days to weeks.
- Plateau phase: Stabilization of symptoms where no new weakness occurs.
- Recovery phase: Gradual improvement over weeks to months as nerve function returns.
Can Guillain-Barré syndrome be mistaken for other conditions?
Yes, Guillain-Barré syndrome can be misdiagnosed as conditions like transverse myelitis, myasthenia gravis, polio, or acute flaccid myelitis. Differentiation is done through nerve conduction studies, Cerebro spinal fluid analysis, and clinical examination.
How does Guillain-Barré syndrome affect breathing?
In severe cases, Guillain-Barré syndrome can weaken respiratory muscles, causing breathing difficulties. Mechanical ventilation may be needed until nerve function recovers. Early monitoring of respiratory function is essential.
What role does physiotherapy play in Guillain-Barré syndrome recovery?
Physiotherapy is crucial for regaining muscle strength, improving mobility, and preventing contractures or joint stiffness. Rehabilitation also includes occupational therapy to help patients regain daily functional abilities.
Can Guillain-Barré syndrome lead to permanent paralysis?
Permanent paralysis is rare, but prolonged nerve damage can lead to residual weakness or muscle atrophy. Early treatment significantly reduces the risk of permanent disability.
What is Miller fisher syndrome (MFS), and how is it related to GBS?
Miller fisher syndrome is a type of Guillain-Barré syndrome characterized by ataxia, ophthalmoplegia (eye movement paralysis), and areflexia. It is caused by autoantibodies against the GQ1b ganglioside and responds well to IVIG or plasmapheresis.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868