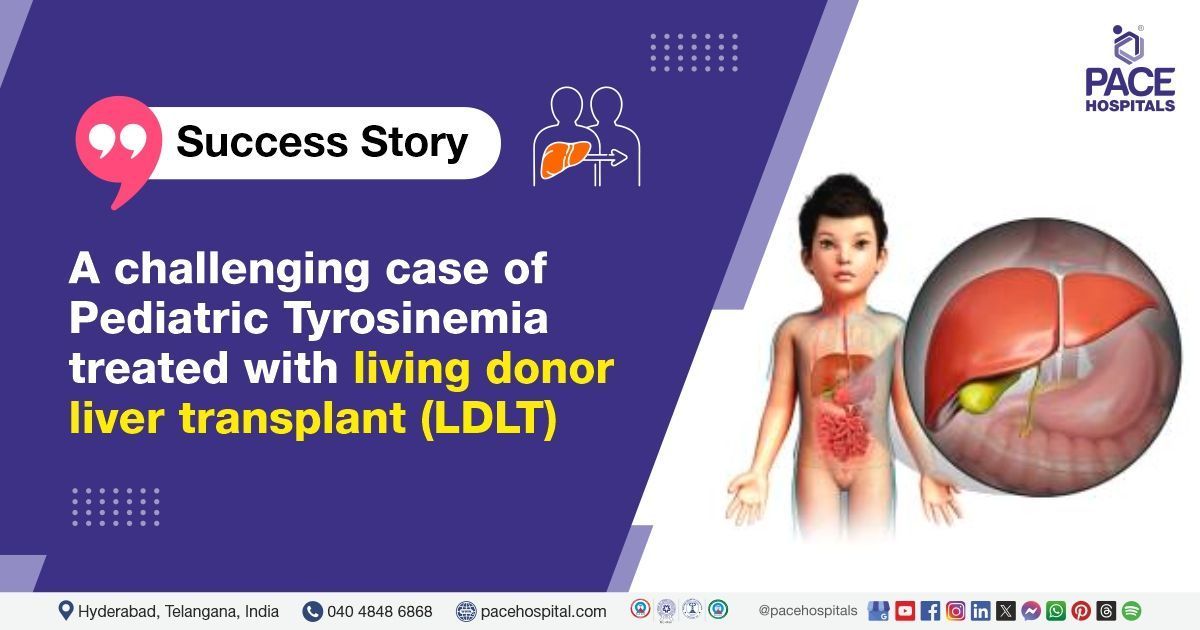
Pediatric Tyrosinemia treated with Living Donor Liver Transplant (LDLT)
A 3-year-old patient was admitted to PACE Hospitals, Hyderabad, with complaints of developmental delays. The team of Gastroenterologists asserted to perform Fumarylacetoacetate hydrolase (FAH) surgery. The patient also has been a known case of chronic liver dysfunction. She was opinioned for Living Donor Liver transplantation (LDLT), and this surgery was successful without any complications.
Chief complaints
A 3-year-old girl was presented to
PACE Hospitals, Hyderabad, with complaints of developmental delays since she was 8 months of age. The parents noticed that the child was not achieving typical developmental milestones and exhibited signs of growth retardation. Upon further clinical evaluation, the patient was diagnosed with Tyrosinemia type 1, a rare inherited metabolic disorder affecting liver function and leading to proximal renal tubular acidosis (RTA) (a condition in which the kidneys' proximal tubules fail to properly reabsorb bicarbonate, leading to metabolic acidosis). The child also had a history of a pathological fracture (a bone break caused by disease or weakened bone) of the right humerus.
Medical history
The patient was admitted to the hospital with the following notable past medical history for additional management:
- Tyrosinemia Type 1: The patient was diagnosed with Tyrosinemia type 1 at a young age. This condition is caused by a deficiency in the enzyme fumarylacetoacetate hydrolase (FAH). It impairs the metabolism of tyrosine and leads to the accumulation of toxic metabolites in the liver and kidneys, resulting in liver dysfunction, kidney abnormalities, and neurological impairments. The patient had been previously managed with tyrosine restriction and liver function monitoring.
- Proximal Renal Tubular Acidosis (RTA): A complication of her metabolic disorder that affected kidney function, leading to the accumulation of acid in the body, which required supportive management.
- Pathological Fracture: The patient had a history of pathological fracture of the right humerus, likely due to the systemic effects of the metabolic disorder, including compromised bone health.
- Liver Dysfunction: On further evaluation, the patient’s
liver function tests indicated hepatic failure and a CECT scan of the abdomen revealed multiple space-occupying lesions (SOLs) in the liver, indicating advanced liver damage.
Diagnosis
As mentioned, the patient was primarily diagnosed with Tyrosinemia type 1 (a known case) and later developed complications including Proximal Renal Tubular Acidosis (RTA), a pathological fracture, and Liver Dysfunction with Multiple SOLs (space-occupying lesions) in the liver.
On further evaluation, the patient’s liver function tests indicated hepatic failure and a CECT scan of the abdomen revealed multiple SOLs in the liver, indicating advanced liver damage. Given the advanced liver damage and deteriorating liver function, Living Donor Liver Transplantation (LDLT) was deemed necessary. The child was thoroughly assessed for transplant eligibility, with preoperative workup including imaging studies, liver function tests, and renal function tests.
Treatment Plan
After careful observation of the patient’s clinical symptoms and medical condition, the Senior Consultant Surgical Gastroenterologist and Liver Transplant Surgeon
Dr. CH. Madhusudhan along with
Dr. Govind Verma, Chief Transplant Hepatologist, recommended a Living Donor Liver Transplant (LDLT) to save the patient.
After a detailed preoperative evaluation, she was admitted for Living Donor Liver Transplantation. Her parents, as donor, were carefully assessed for suitability, and the risks and benefits of the transplant were thoroughly explained to the family. A detailed pre-anesthesia check-up (PAC) was completed to ensure the patient was fit for surgery.
Surgical Procedure: Living Donor Liver Transplantation (LDLT)
The patient underwent liver transplant procedure, where a portion of the liver was transplanted from the living donor (her parent) to replace the patient's damaged liver. The surgery was conducted successfully after thorough discussions with the family regarding the perioperative risks, including the potential for complications such as rejection, infection, and bleeding.
Postoperative Course
The initial postoperative period was uneventful. The patient was monitored closely in the intensive care unit (ICU), where regular liver Doppler studies were performed. These tests showed that the blood flow to the transplanted liver was normal, and the immediate graft function appeared satisfactory.
However, on Postoperative day 3 (POD 3), the patient developed a sudden hypoxic event (a condition characterized by insufficient oxygen supply to tissues), followed by cardiac arrest. Immediate cardiopulmonary resuscitation (CPR) was performed, and the patient was successfully revived. She was intubated and stabilized in the ICU. The cause of the hypoxia and cardiac arrest was determined to be a metabolic imbalance related to her underlying metabolic condition, which was exacerbated by the stress of the surgery and the use of immunosuppressive drugs.
After stabilization, the patient developed ileus, a condition in which the intestines temporarily stop functioning, which is common in postoperative patients. The ileus was managed conservatively with bowel rest, hydration, and medications to promote bowel motility. Additionally, the patient had minimal bilious drain output, which was closely monitored and managed conservatively to prevent further complications such as bile leakage.
Medications and Postoperative Care
During the postoperative period, the following treatments were administered:
- IV Fluids: To maintain hydration and correct electrolyte imbalances.
- Immunosuppressive Medications: An immunosuppressant to prevent organ rejection.
- Antibiotics: IV antibiotics were given to prevent infection, especially since immunosuppressive therapy, which can increase the risk of infection.
- Proton Pump Inhibitors (PPIs): To protect against the development of gastric ulcers.
- Multivitamins: To support overall recovery and nutrition.
- Antiemetics: For nausea management post-surgery.
- Analgesics and Antipyretics: These are used for pain relief and to manage fever or discomfort.
Postoperative Monitoring
During the postoperative period, the following diagnostic tests were performed to monitor the patient's condition:
- Liver Function Tests: Liver enzyme levels (e.g., ALT, AST) were closely monitored and showed improvement, indicating that the transplanted liver was functioning properly.
- Immunosuppressive Doses: The doses of immunosuppressive medications were adjusted based on the patient's liver function and response to therapy.
- Drain Output: The bilious drain output was monitored for any signs of leakage or complications, and minimal output was noted and managed conservatively.
- Neurological Assessment: Given the underlying developmental delays and neurological risks associated with Tyrosinemia Type 1, the patient was monitored closely for any signs of neurological deterioration.
Discharge Plan
The patient was discharged in a hemodynamically stable condition with the drain in situ for ongoing monitoring. The child’s condition improved over the hospital stay, with normalization of liver enzymes and stable kidney function.
Follow-up Plan
- Immunosuppressive Therapy: Continued treatment to prevent liver rejection. Blood levels of these drugs will be monitored regularly.
- Infection Prevention: Continue the prescribed antibiotics until the healthcare team determines that the risk of infection has decreased.
- Nutritional Support: The child should adhere to a low-tyrosine diet to manage Tyrosinemia Type 1 and ensure adequate nutrition.
- Regular Monitoring: Follow-up visits will include regular liver and renal function tests and immunosuppressive drug levels. The family will be educated on signs of organ rejection (e.g., jaundice, fever, abdominal pain) and infection (e.g., fever, redness, swelling).
Review Notes
The patient was advised to follow up with Dr. CH Madhusudhan in the OPD after 5 days, ensuring a prior appointment is scheduled and the HPE report is brought along for discussion. Additionally, a follow-up appointment in the OPD with Dr. A Kishore Kumar with serum calcium, serum magnesium, serum electrolytes, serum phosphorus report 5 days later to assess progress and provide further care as needed.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868