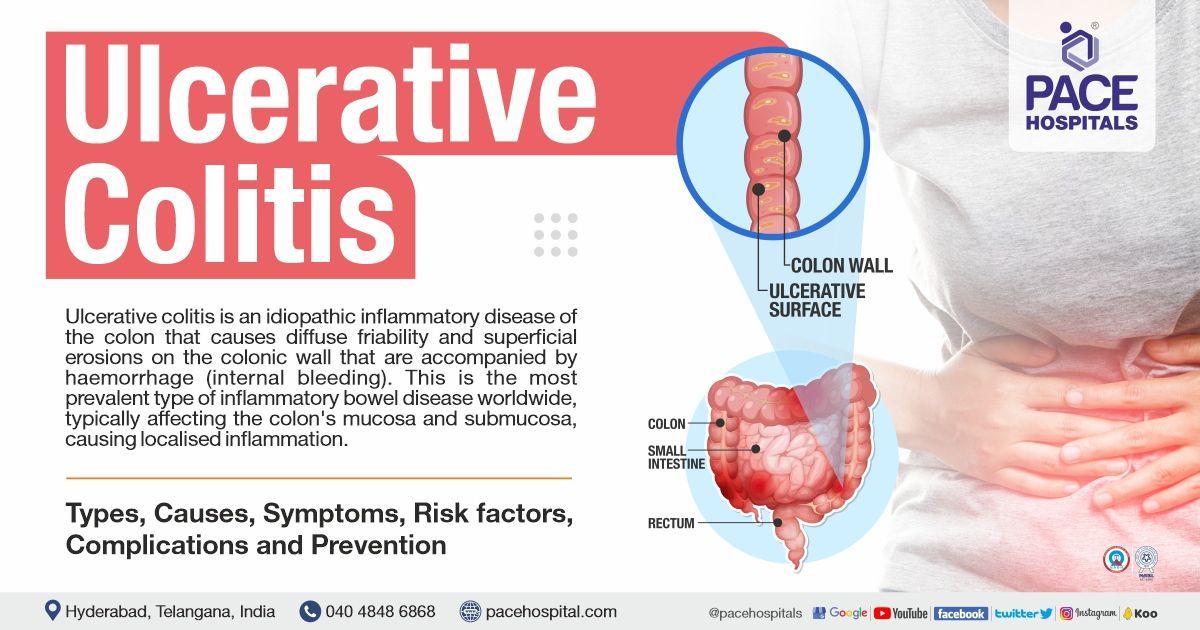
Ulcerative Colitis – Symptoms, Causes, Types, Risk Factors, Complications & Prevention
Ulcerative colitis meaning
Ulcerative colitis (UC) is an idiopathic (unknown reason) inflammatory disease of the colon that causes diffuse friability and superficial erosions on the colonic wall that are accompanied by haemorrhage (internal bleeding).
This is the most prevalent type of inflammatory bowel disease worldwide, typically affecting the colon's mucosa and submucosa, causing localised inflammation. The disease usually initiates in the rectum and progresses continuously inward (towards the colon). The disease severity can also vary histologically, ranging from mild to severe ulceration and dysplasia.
Adults are more likely to have ulcerative colitis than Crohn's disease. However,
Crohn's disease and ulcerative colitis are less common compared to the paediatric population. Ages between 15 and 30 are when the initial onset peaks. Ulcerative colitis has an unknown precise cause, and a family history of the ailment is the most significant independent risk factor (8 % to 14 % of patients). The condition usually develops gradually, and individuals will probably go through periods of spontaneous remission before relapsing.
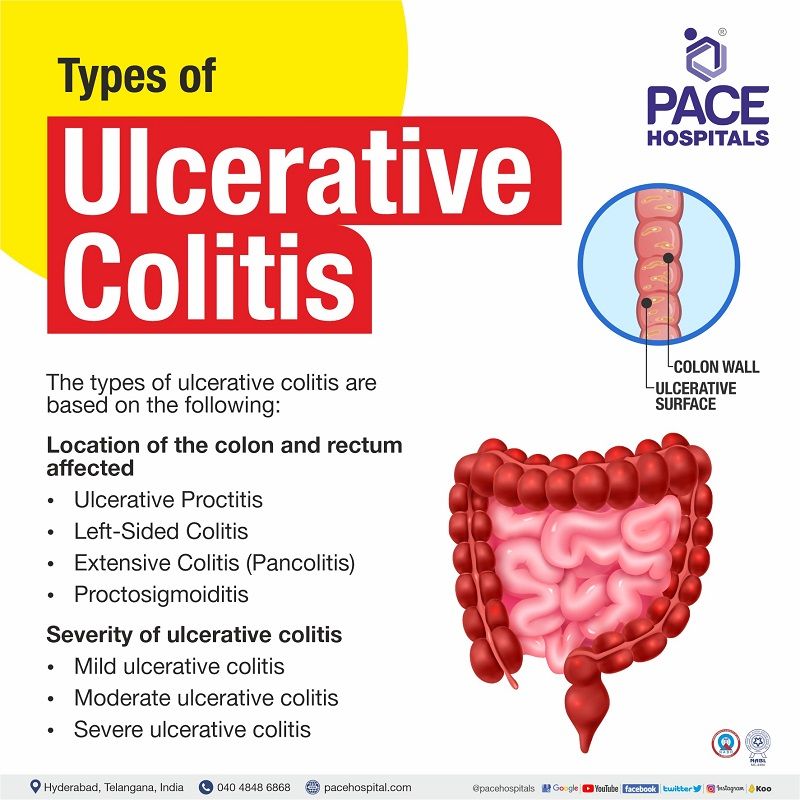
Types of ulcerative colitis
The types of ulcerative colitis are based on the following:
- Location of the colon and rectum affected
- Severity of ulcerative colitis
Location of the colon and rectum affected
Based on the location of the colon and rectum affected, they are usually four types of ulcerative colitis as:
- Ulcerative Proctitis
- Left-Sided Colitis
- Extensive Colitis (Pancolitis)
- Proctosigmoiditis
- Ulcerative Proctitis: In this type, the inflammation only occurs in the rectum (usually less than 6 inches), the final section of the large intestine. About one-third of those who have ulcerative colitis (UC) are affected by this type of ailment. The sudden need to defecate, pain and bleeding in the rectum are the symptoms of this condition.
- Left-Sided Colitis: This type of ulcerative colitis can cause inflammation anywhere from the rectum to the splenic flexure of the colon (curve in the upper left portion of the abdomen, where the descending colon and transverse colon meet). Loss of hunger, left-side abdominal pain, bloody diarrhoea and loss of weight are the symptoms of this condition.
- Extensive Colitis (Pancolitis): This type of ulcerative colitis frequently affects the entire colon. The inflammation occurs from the rectum and extends past the splenic flexure. The symptoms include abdominal pain, loss of hunger, increased body temperature, cramps and bloody diarrhoea.
- Proctosigmoiditis: This type of ulcerative colitis affects only the rectum and sigmoid colon, the bottom portion of the colon above the rectum. The symptoms include tenesmus, bloody diarrhoea, cramps and pain in the abdomen.
Severity of ulcerative colitis
Based on the disease severity or stages, it is graded as mild to moderate ulcerative colitis, such as:
- Mild ulcerative colitis
- Moderate ulcerative colitis
- Severe ulcerative colitis
- Mild ulcerative colitis: having four rectal bleeding episodes in a day.
- Moderate ulcerative colitis: having more than four rectal bleeding episodes in a day.
- Severe ulcerative colitis: having more than six rectal bleeding episodes in a day accompanied by hypoalbuminemia.
Fulminant Ulcerative Colitis
Fulminant ulcerative colitis is a rare yet dangerous form of ulcerative colitis, characterised by complete inflammation of the colon lining, leading to severe symptoms like stomach discomfort and bloody diarrhoea.
Most ulcerative colitis patients don't experience this, as it affects less than 10% of those who have it, typically during the initial episode of symptoms.
Severity of ulcerative colitis classification
| Elements | Mild | Moderate | Severe | Fulminant |
|---|---|---|---|---|
| Stools (count/day) | Less than 4 | 4-6 | More than 6 | More than 10 |
| Presence of blood in stool | Intermittent | Between mild and severe | Frequent | Continuous |
| Haemoglobin | Normal | Normal | Less than 75% of the normal value | A blood transfusion is required |
| ESR rate (mm/hr) | ≤ 30 | ≤ 30 | >30 | >30 |
| Temperature (degree Celsius) | Normal | Normal | >37.5 | >37.5 |
| Clinical Signs | Absence of abdominal tenderness | NA (Unavailability of data) | Presence of Abdominal tenderness | Presence of Abdominal tenderness and distention |
Ulcerative colitis causes
Etiology of ulcerative colitis
The ulcerative colitis causes are uncertain, and it is believed to be the outcome of any of the following causative factors:
- Abnormal immune reactions
- Environment
- Genes
Abnormal immune reactions:
The body's immune system aids in providing a defensive mechanism against infections. In order to eliminate the infection's source, the white blood cells are typically released into the blood by the immune system to combat infections.
According to some researchers, ulcerative colitis is an autoimmune disease where the immune system misinterprets good bacteria (helps in digestion) in the colon as dangerous bacteria or infection and attacks the healthy tissue, resulting in inflammation and redness of the body tissue at the infected area.
Environment:
The likelihood of getting ulcerative colitis also appears to be influenced by the place of living. Researchers have looked into several environmental factors that may be connected to ulcerative colitis, including air pollution, medications, and particular diets.
Genes:
Sometimes, ulcerative colitis runs in families. Studies have demonstrated that individuals with ulcerative colitis may carry specific abnormal genes. However, researchers are unable to show a direct causal relationship between the abnormal genes and ulcerative colitis.
Ulcerative colitis symptoms
The primary ulcerative colitis symptom is bloody diarrhoea with or without mucous. In addition, the following are the ulcerative colitis disease symptoms:
- Tenesmus (a painful urge to pass stools without excreting stool)
- Unable to hold stool
- Pain in abdomen
- General malaise
- Decrease in body weight
- Increase in body temperature
- Loss of body fluids
- Reduce hunger
- Skin sores
- Anaemia
- Eye pain while exposed to bright light
- Joint pain
- Canker sores (mouth ulcers)
- Vomiting and it's feeling
Ulcerative colitis emergency symptoms
Even if the patient only has minor or moderate symptoms, serious problems can still develop. It's critical to recognise emergencies and seek urgent assistance, such as:
- Rectal bleeding
- Unable to take food or liquids for longer than 24 hours
- Increase in body temperature with chills or rigours
- Loss of body fluids
- Swooning (fainting)
Ulcerative colitis symptoms in females
Although ulcerative colitis (UC) symptoms differ from person to person, they frequently have a comparable impact on both men and women. Nevertheless, in females, hormonal changes may cause UC symptoms to worsen during the menstrual cycle. Symptoms include:
- Irregular periods
- Menstrual pain
- Severe abdominal pain and diarrhoea
Ulcerative colitis risk factors
The presence of the following triggering factors can elevate the risk of having ulcerative colitis
- Age: It is most likely to be in older age (>60 years) or between the ages of 15 and 30.
- Family history: The presence of Ulcerative colitis in a family increases the risk by up to 30 %. There is a four-fold increased risk of acquiring ulcerative colitis in a first-degree relative of a patient.
- Ethnicity: Jews experience ulcerative colitis more frequently than people of other races.
- Medications: Consumption of birth control pills and broad-spectrum antibiotics can elevate the risk of UC.
- Diet: Researchers believe westernised eating habits (low in fruits & vegetables and high in fat & sodium) or lifestyles may trigger factors causing Inflammatory bowel disease (IBD) symptoms.
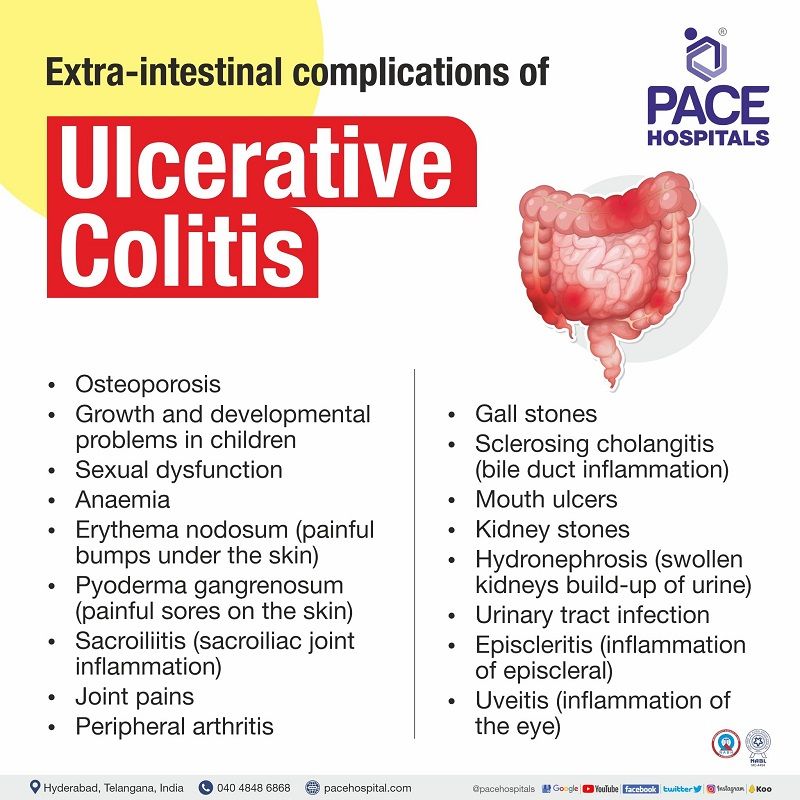
Ulcerative colitis complications
The symptoms of ulcerative colitis remit and relapse throughout the course of a lifetime. Ulcerative colitis complications are broadly classified into two categories.
- Extra-intestinal complications
- Intestinal complications
Extra-intestinal manifestations of ulcerative colitis
- Osteoporosis
- Growth and developmental problems in children
- Sexual dysfunction
- Anaemia
- Erythema nodosum (painful bumps under the skin)
- Pyoderma gangrenosum (painful sores on the skin)
- Sacroiliitis (sacroiliac joint inflammation)
- Joint pains
- Peripheral arthritis
- Gall stones
- Sclerosing cholangitis (bile duct inflammation)
- Mouth ulcers
- Kidney stones
- Hydronephrosis (swollen kidneys, build-up of urine)
- Urinary tract infection
- Episcleritis (inflammation of episcleral)
- Uveitis (inflammation of the eye)
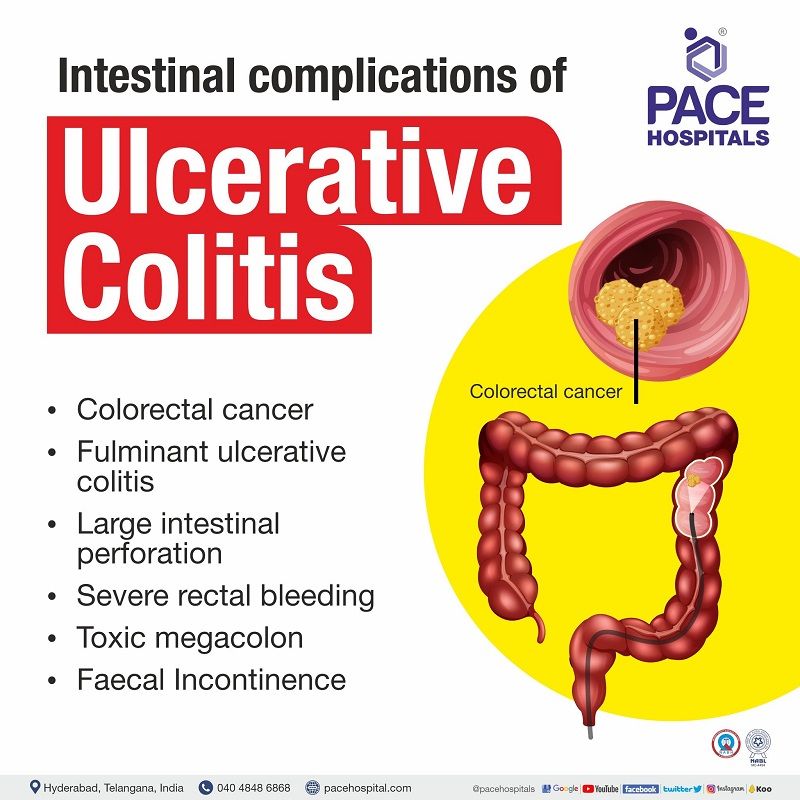
Intestinal complications
- Colorectal cancer
- Fulminant ulcerative colitis
- Large intestinal perforation
- Severe rectal bleeding
- Toxic megacolon
- Faecal Incontinence (Inability to pass stool from the rectum)
- Complications in females:
- Anaemia
- Osteoporosis
- Delay in puberty
- Sexual dysfunction
Ulcerative colitis diagnosis
The gastroenterologist will ask about the patient's medical and family history, which includes medications, and jot down the patient's symptoms. The gastroenterologist would do a complete physical examination and would like to prescribe any or a combination of the following Ulcerative colitis tests.
- Blood tests
- Stool samples
- Endoscopic tests
- Imaging tests
Ulcerative colitis treatment
Ulcerative colitis treatment is based on the severity of the condition and frequency of symptoms flare up. The treatment includes medication and surgery.
The medication therapy is chosen based on the patient's condition, such as:
- Aminosalicylates
- Corticosteroids
- Immunosuppressants
- Biological agents
- JAK inhibitors
- Surgical applications include:
- Ileoanal reservoir surgery
- Ileostomy
Fulminant ulcerative colitis treatment
Fulminant ulcerative colitis treatment includes intravenous (IV) corticosteroid medications as the first-line medication. In the event of corticosteroid ineffectiveness, the gastroenterologist would prescribe immunosuppressants or biologic agents. However, surgery (colectomy) might be an option if medication therapy fails to alleviate the symptoms.
Ulcerative colitis prevention
The root cause of ulcerative colitis is idiopathic (unknown), where some researchers believe it might be due to an autoimmune condition. Hence, it cannot be prevented. However, proper nutrition can play a significant role in disease control.
The following can aid in alleviating symptoms after making dietary changes.
- Avoiding carbonated beverages
- Avoiding high-fibre foods
- Increase fluid intake
- Consuming food more frequently and less quantitatively
- Maintaining a food diary to identify the triggering factors
- Intake of probiotics (yoghurt, Kimchi etc.)
Ulcerative colitis remission
- Remission happens when Ulcerative Colitis drugs reduce or eliminate colon inflammation, which controls symptoms. Remissions can last anything from a few weeks or months to several years.
- The condition Ulcerative Colitis can stay in remission for a long time if the prescribed treatments are effective and no other factors trigger a flare-up.
- It is crucial to continue taking the drugs even if Ulcerative Colitis is in remission for years in order to help avoid further flare-ups.
One should consult a medical professional if they experience a persistent change in their bowel habits or have the following signs and symptoms, such as:
- Pain in the abdomen
- Blood in stools
- Diarrhoea unresponsive to over-the-counter (OTC) medications
- Sleep disturbance due to diarrhoea
- An unexplained fever that lasts more than 24 to 48 hours
Although ulcerative colitis is typically not deadly, it is a serious condition that can occasionally result in life-threatening complications.
Frequently asked questions, FAQs
Related article

Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868